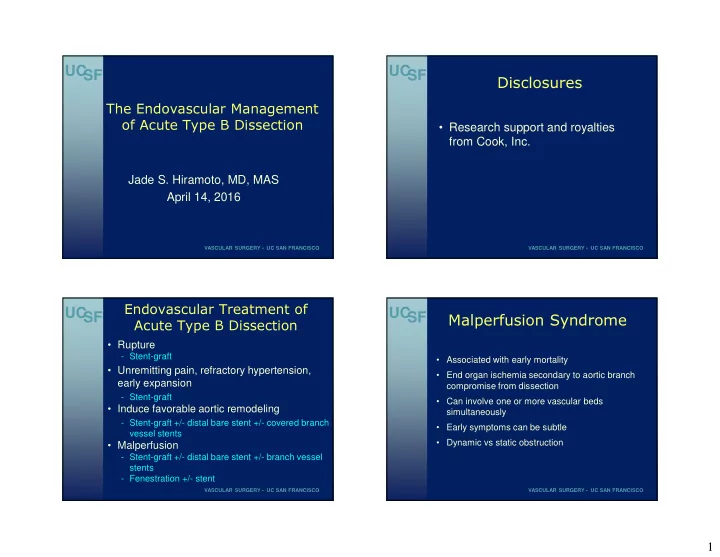
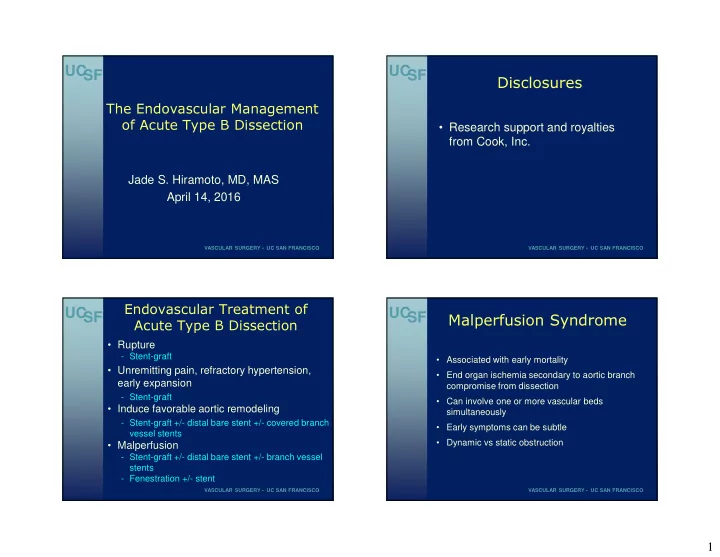
UC UC SF SF Disclosures The Endovascular Management • Research support and royalties of Acute Type B Dissection from Cook, Inc. Jade S. Hiramoto, MD, MAS April 14, 2016 VASCULAR SURGERY • UC SAN FRANCISCO VASCULAR SURGERY • UC SAN FRANCISCO UC UC Endovascular Treatment of SF SF Malperfusion Syndrome Acute Type B Dissection • Rupture - Stent-graft • Associated with early mortality • Unremitting pain, refractory hypertension, • End organ ischemia secondary to aortic branch early expansion compromise from dissection - Stent-graft • Can involve one or more vascular beds • Induce favorable aortic remodeling simultaneously - Stent-graft +/- distal bare stent +/- covered branch • Early symptoms can be subtle vessel stents • Dynamic vs static obstruction • Malperfusion - Stent-graft +/- distal bare stent +/- branch vessel stents - Fenestration +/- stent VASCULAR SURGERY • UC SAN FRANCISCO VASCULAR SURGERY • UC SAN FRANCISCO 1
UC UC Malperfusion Syndrome: Malperfusion Syndrome: SF SF Dynamic Obstruction Static Obstruction • Compressed true lumen unable to provide • Dissecting process extends into branch adequate volume flow vessel, causing narrowing • Motion of intimal flap within aortic lumen • Unlikely to resolve with restoration of obstructs orifice of branch vessel aortic true lumen flow alone • Responsible for ~80% of malperfusion • Re-assess after stent graft/fenestration • May vary depending on blood pressure • May require branch vessel stenting • Would be expected to respond to exclusion of entry tear or aortic fenestration VASCULAR SURGERY • UC SAN FRANCISCO VASCULAR SURGERY • UC SAN FRANCISCO Uchida et al; ICTVS 2009;8:75-78 Uchida et al; ICTVS 2009;8:75-78 UC UC SF SF Goals of Treatment Treatment Strategies • Focus on most minimal/expedient intervention • Stent-graft repair to restore perfusion as soon as possible - Advantages: restore true lumen flow; prevent late aneurysm formation; favorable aortic remodeling with lower risk of aortic rupture • Primary goal: Expansion of true lumen with - Disadvantages: paraplegia; retrograde dissection restoration of flow to visceral vessels/lower extremity - Stent-graft repair with coverage of proximal entry tear • Fenestration - Advantages: restore true lumen flow; minimal risk of - Fenestration (convert complicated into uncomplicated dissection) paraplegia - Disadvantages: promotes blood flow through false lumen, potentially leading to progressive • Secondary goal: obliteration of false lumen flow dilation/aneurysmal degeneration with subsequent complete thrombosis VASCULAR SURGERY • UC SAN FRANCISCO VASCULAR SURGERY • UC SAN FRANCISCO 2
UC UC SF SF Endovascular Treatment of Intravascular Ultrasound Acute Type B Dissection • Pre-operative imaging - CT angiography - Assess vertebral circulation • IVUS and angiography - Verify preoperative anatomy - Verify true lumen passage of guidewire - Avoid inadvertent deployment in false lumen • Consider transesophageal echo VASCULAR SURGERY • UC SAN FRANCISCO VASCULAR SURGERY • UC SAN FRANCISCO Sfyroeras et al; JEVT 2011;18:78-86 UC UC SF SF Angiography Treatment: Stent-graft Repair • Avoid aggressive oversizing • Avoid ballooning of seal zones • Minimize aortic coverage (<20cm) to reduce risk of spinal ischemia • Coverage of left subclavian artery (~50%) • Re-assess distal perfusion after stent-graft deployment - May still have inadequate true lumen flow - Consider placement of uncovered distal stent: support true lumen and stabilize dissection flap - Additional stent placement for visceral branch vessel •Long sheath inserted into aortic arch •“Viscera on a stick” obstruction •Angiography at different levels to verify true lumen position VASCULAR SURGERY • UC SAN FRANCISCO VASCULAR SURGERY • UC SAN FRANCISCO 3
UC UC SF SF •Subsequent angiography at different levels VASCULAR SURGERY • UC SAN FRANCISCO VASCULAR SURGERY • UC SAN FRANCISCO UC UC SF SF The Petticoat Concept The Petticoat Concept • Provisional extension to induce complete • Placement of bare stent scaffold attachment extension into implanted stent-graft - Abolish distal true lumen collapse • Placement of scaffolding distal stent after - Enhance remodeling process of entire sealing proximal tear with stent-graft dissected aorta by fixation of distal lamella • Why do this? • STABLE trial (complicated dissections): - Even after successful thoracic stent-graft placement, fate of distal abdominal segment - Favorable early clinical outcomes unresolved - Favorable aortic remodeling - With large distal reentry points, abdominal segment of false lumen tends not to thrombose and remodel completely - Try to diminish late complications Nienaber et al; JEVT 2006;13:738-746 Nienaber et al; JEVT 2006;13:738-746 VASCULAR SURGERY • UC SAN FRANCISCO VASCULAR SURGERY • UC SAN FRANCISCO Lombardi et al; J Vasc Surg 2014;59:1544-1554 4
UC UC SF SF Modified Petticoat Technique Modified Petticoat Technique • Concern regarding original Petticoat concept: - Further aortic dissection/damage from initial TEVAR deployment into distal diseased aorta • Pre-placement of distal bare stent as adjunct to proximal TEVAR - Prevent excessive force of the distal end of the stent graft on the aorta - Prevent early aortic wall damage, distal re- dissection • Restricts effect of oversizing of distal stent-graft - Reduces potential for distal true lumen collapse and visceral malperfusion Initial release of distal bare stent at distal landing zone Subsequent deployment of proximal stent-graft VASCULAR SURGERY • UC SAN FRANCISCO VASCULAR SURGERY • UC SAN FRANCISCO He et al; Eur J Vasc Endovasc Surg 2015;50:450-459 He et al; Eur J Vasc Endovasc Surg 2015;50:450-459 UC UC SF SF Modified Petticoat Technique Treatment: Fenestration • Diameter of adjunctive bare stent: • Relieve dynamic obstruction by creating flap - Select using greatest diameter of TL at fenestration to generate large reentry tear intended distal edge of stent-graft - Bare stent not oversized compared to aorta • Potential use in patients who cannot be treated with a thoracic stent-graft because of anatomic • Anticipate 3-4 cm of overlap with distal constraints end of proximal covered stent-graft • Flow ensured within false lumen, precluding • Sinus XL-stent (OptiMed, Ettlingen, thrombosis Germany): - Diameter: 18-26 mm • Branch vessel compromise (malperfusion) is - Length: 60-80 mm treated, but not the aorta - Available in diameters 16-36 mm in varying • If static obstruction exists, perform branch lengths vessel stent placement • Largest wallstent: 24 mm VASCULAR SURGERY • UC SAN FRANCISCO VASCULAR SURGERY • UC SAN FRANCISCO He et al; Eur J Vasc Endovasc Surg 2015;50:450-459 5
UC UC SF SF Fenestration: Technique Fenestration: Technique • Smaller (true) to larger (false) lumen • May require membrane puncture with re- entry catheter • Rosch-Uchida needle, Colopinto needle, or • Guidewire passed through re-entry back end of 0.014 wire to create fenestration catheter and across membrane close to compromised aortic branch • Guidewire snared through contralateral • After needle and stiff wire advanced from true transfemoral access (through and through to false lumen, catheter advanced and wire access) confirmation by angiography • Cheese-wire maneuver • Large angioplasty balloon used to create • Portions of fenestrated membrane can fenestration tear occlude iliac artery – be prepared to stent VASCULAR SURGERY • UC SAN FRANCISCO VASCULAR SURGERY • UC SAN FRANCISCO Kos et al; Cardiovasc Intervent Radiol 2011;34:1296-1302 UC UC Fenestration with Bare Metal Stent SF SF Stent-graft or Fenestration? Placement • “Funnel technique” • Endograft therapy first line of treatment - Aims to restore native aortic anatomy by closure of • Uncovered stent primary tear - True lumen to false lumen - Above level of visceral vessels • Percutaneous fenestration - Aims to increase true lumen perfusion by equalizing • May require additional pressures in true/false lumens fenestration/stent placement - Does not address underlying abnormality of below visceral vessels dissection itself - Limit to patients who lack suitable proximal landing - For persistent malperfusion of zone or complex multilumen dissections not easily lower extremities corrected by closure of primary tear VASCULAR SURGERY • UC SAN FRANCISCO VASCULAR SURGERY • UC SAN FRANCISCO Vendrell et al; J Thorac Cardiovasc Surg 2015;150:108-115 Miyachi et al; J Nippon Med Sch 2014;81:340-345 6
Recommend
More recommend