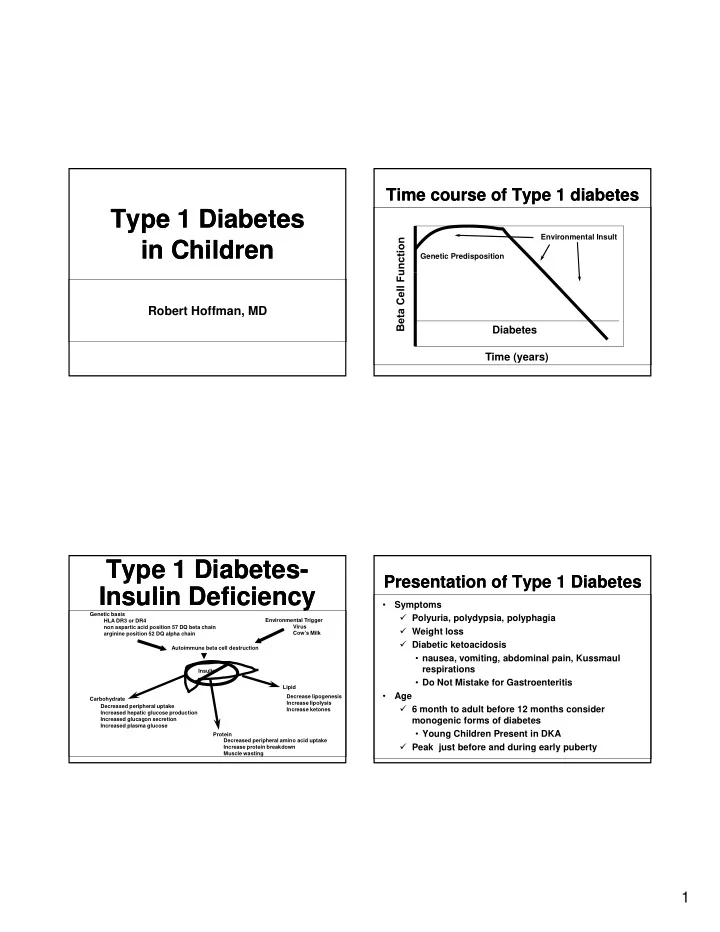
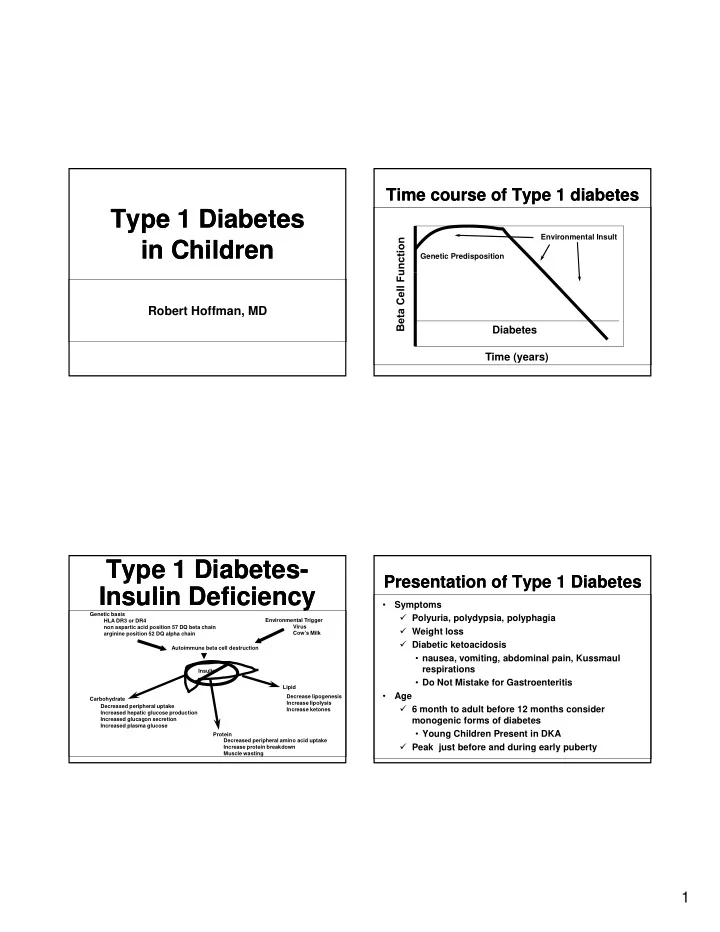
Time course of Type 1 diabetes Time course of Type 1 diabetes Type 1 Diabetes Type 1 Diabetes Environmental Insult in Children in Children Genetic Predisposition Robert Hoffman, MD Diabetes Time (years) Type 1 Diabetes- Type 1 Diabetes- Presentation of Type 1 Diabetes Presentation of Type 1 Diabetes Insulin Deficiency Insulin Deficiency • Symptoms Genetic basis � Polyuria, polydypsia, polyphagia HLA DR3 or DR4 Environmental Trigger Virus non aspartic acid position 57 DQ beta chain � Weight loss arginine position 52 DQ alpha chain Cow’s Milk � Diabetic ketoacidosis Autoimmune beta cell destruction • nausea vomiting abdominal pain Kussmaul nausea, vomiting, abdominal pain, Kussmaul respirations Insulin • Do Not Mistake for Gastroenteritis Lipid • Age Decrease lipogenesis Carbohydrate Increase lipolysis Decreased peripheral uptake � 6 month to adult before 12 months consider Increase ketones Increased hepatic glucose production Increased glucagon secretion monogenic forms of diabetes Increased plasma glucose • Young Children Present in DKA Protein Decreased peripheral amino acid uptake � Peak just before and during early puberty Increase protein breakdown Muscle wasting 1
Diagnosis Diagnosis How Does the DCCT How Does the DCCT Relate to Children? Relate to Children? • Urine dipstick positive for glucose and ketones • Plasma glucose >200 mg/dl at any time and • Are the risks of intensive diabetes therapy ketones greater? t ? • Fasting plasma glucose >126 mg/dl • Will intensive diabetes therapy in childhood • Stress induced hyperglycemia is a rare reduce the risks of long term confounder complications? � Usually no history of polyuria, polydypsia � Usually no ketones DCCT: Adolescents DCCT: Adolescents Goals of Diabetes Therapy Goals of Diabetes Therapy (13 to 18 years) versus Adults (13 to 18 years) versus Adults Adolescent Adults • Prevent Diabetic Ketoacidosis Mean HbA1c(%) 8.06 ± 0.13 7.12 ± 0.03 Intensive 9.76 ± 0.12 9.02 ± 0.05 • Prevent Severe Hypoglycemia yp g y Conventional Conventional • Maintain Normal Growth and Development Severe Hypoglycemia 85.7 56.9 • Prevent Long-Term Complications Rate (/100 pt-years) 2.93 3.30 Relative Risk 2
DCCT Retinopathy in DCCT Retinopathy in Summary Summary Adolescents Adolescents • Adolescents in the DCCT had poorer glycemic control than did adults regardless of treatment group • Intensive therapy was associated with improved glycemic control in adolescents • Good glycemic control still prevents or delays the onset of diabetic complications • Good glycemic control prolongs beta cell function DCCT Microalbuminuria DCCT Microalbuminuria Children less than 13 Children less than 13 in Adolescents in Adolescents • Children with diabetes onset before age 5 80 buminuria 70 have reduced neurocognitive test scores as 60 adolescents. 50 50 Percent Microalb 40 • This may be due to recurring 30 20 hypoglycemia. Conventional 10 Intensive 0 • The prepubertal years have less impact on 0 2 4 6 8 10 the development of diabetes complications. Years 3
Glucose Target Range Glucose Target Range Exercise Exercise • Adolescents � ADA target range 70-120 mg/dl before meals 100-150 • HbA1c improves and insulin sensitivity at bedtime increase with improved physical fitness � Raise target range if patient has hypoglycemic unawareness unawareness • Competitive athletes with IDDM have Competitive athletes with IDDM have • Preschool children poorer control than sedentary patients � Target range 100-180 mg/dl before meals and bedtime snack � Fear of hypoglycemia and abnormal eating schedules � Highs preferable to lows • School-age children � Adjust goals downward as recognition of lows develops Arslanian et al. Diabetes Care 1990;13:9 Huttunen et al. Diabetes Care 1989;12:737 Marrero et al. Pediatr 1988:81:519 Eberling et al. Diabetes 1995;44:477 Diet Diet Monitoring Complications Monitoring Complications • Goal Is Consistency, Not Calorie • Overt complications rare in children and Restriction adolescents • 60% Carbohydrate, 20%Fat, 20% Protein • Retinopathy • Insulin to Carbohydrate Ratios • Insulin to Carbohydrate Ratios � � Dilated eye exam yearly after 5 years and puberty Dilated eye exam yearly after 5 years and puberty • Nephropathy � Lispro, aspart, glulysine 1 unit per number of carbs � Blood pressure second most important predictor � Insulin should be taken before meals if patient can predict how � much they are going to eat Microalbumin measurement same schedule as eye exam • Smoking worsens every complication � Toddlers and sick days after meals 4
Treatment of Treatment of Hypoglycemia in IDDM Hypoglycemia in IDDM • Test blood sugar • If low 15 - 20 grams of simple carbohydrate wait 15 min What Goes Wrong? What Goes Wrong? What Goes Wrong? What Goes Wrong? � 1/2 cup juice or pop ,3 glucose tabs, 4 sugar cubes • Incoherent at home use glucagon � <30 kg 0.5 mg � >30 kg 1.0 mg • Hospital � 25 % dextrose 2 ml/kg Dawn and Somogyi Dawn and Somogyi Hypoglycemia Hypoglycemia Phenomena Phenomena • Why do low blood sugars happen � Inaccurate carbohydrate counting • Dawn Phenomena � Increasing insulin resistance from 3 AM to 8AM � Failure to plan appropriately for exercise Failure to plan appropriately for exercise � Nocturnal growth hormone secretion � N t l th h ti � Normal sugar at 3 AM, high at 8 AM � Inadequate glucose testing • Somogyi Phenomena � Alcohol � Rebound hyperglycemia following hypoglycemia � Unexplained � Low sugar at 3 AM, high at 8 am � Doesn’t exist � Most Somogyi is overtreatment of lows or waning insulin 5
Prevention of DKA Prevention of DKA Type 1 Diabetes Type 1 Diabetes • Management requires a multidisciplinary team approach, • Test urine ketones including a nurse educator, dietitian, social worker and/or � If glucose >250 mg/dl psychologist, and a physician • The keys to good control are assuring adherence to � With vomiting or illness testing and insulin usage. This is usually best accomplished through assuring ongoing parental • Extra short acting insulin involvement � Small or moderate ketones 10% of total There is no magic insulin regimen but use of the newer • daily insulin dose insulins lispro, aspart, and glargine are associated with better postprandial glucose control and less � Large ketones 20% of total daily dose hypoglycemia • Insulin pumps are one tool that can be used in the appropriate individual Prevention of DKA Prevention of DKA Type 1 Diabetes Type 1 Diabetes • Sick days with ketones � Glucose > 200 mg/dl: sugar free clear in the Adult in the Adult liquids � Glucose < 200 mg/dl: sugar containing � Glucose < 200 mg/dl: sugar containing clear liquids � Monitor glucose and ketones frequently Kathleen Dungan MD • 3-4 emesis in a row without any retention trip to ER • Have parent give injections 6
Post-Trial F/u of DCCT: Post-Trial F/u of DCCT: Classification of Diabetes Classification of Diabetes Metabolic Memory Metabolic Memory • Type 1 diabetes • Despite early loss of glycemic differences, a � Autoimmune/Non-autoimmune continued reduction in microvascular risk and emergent risk reductions for myocardial � Latent autoimmune diabetes of the adult infarction and all-cause mortality were y (LADA) (LADA) observed during 10 years post-trial follow-up. • Type 2 diabetes � Ketosis prone type 2 diabetes • MODY (monogenic forms) • Secondary forms ADA; Diabetes Care. 2010;33:S62-9. “The Persistence of Memory”, Dali, 1931 Metabolic Memory Metabolic Memory Target Blood Glucose Ranges Target Blood Glucose Ranges Long- Long -term follow term follow- -up of the DCCT up of the DCCT Retinopathy Nephropathy CV Disease 1. American Diabetes Association (2009) Clinical Practice Recommendations Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications 2. American Association of Clinical Endocrinologists (2002) (DCCT/EDIC) Research Group, Arch Intern Med 2009;169:1307-1316. 7
Insulin Profiles Insulin Profiles Basal Prandial Insulin Basal Prandial Insulin Insulin Onset of Action Peak Action Duration of Action Preparations • Education is important! BOLUS INSULIN Regular 30 minutes 2-4 hours 6-10 hours � Consistent carbohydrate diet Lispro ( Humalog ) Lispro ( Humalog ) 5 15 minutes 5-15 minutes 1-2 hours 1 2 hours 4-6 hours 4 6 hours Aspart ( Novolo g) � Carb counting (particularly for erratic Glulisine (Apidra) eating patterns) BASAL INSULIN NPH 1-2 hours 4-8 hours 10-20 hours • Target pre-meal BG 90-130 mg/dL Glargine (Lantus) 1-2 hours Flat ~ 24 hours Detemir (Levemir) ? Flat ~ 24 hours Mooradian, A. D. et. al. Ann Intern Med 2006;145:125-134 If all else fails… If all else fails… Pattern Management Pattern Management Think Like a Pancreas! Think Like a Pancreas! 1) First ask about missed doses, extra carbs Basal-Bolus Insulin: 3 Components 2) Look for lows 3) Evaluate FBG 1 ) Basal: 50% of total daily needs 4) Pre-meal readings Bolus 2) Prandial/nutritional: 50% of total daily needs 5) If no pattern, get more data 3) Supplemental (Correction) Clement S et al. Diabetes Care . 2004;27:553-591. 8
Recommend
More recommend