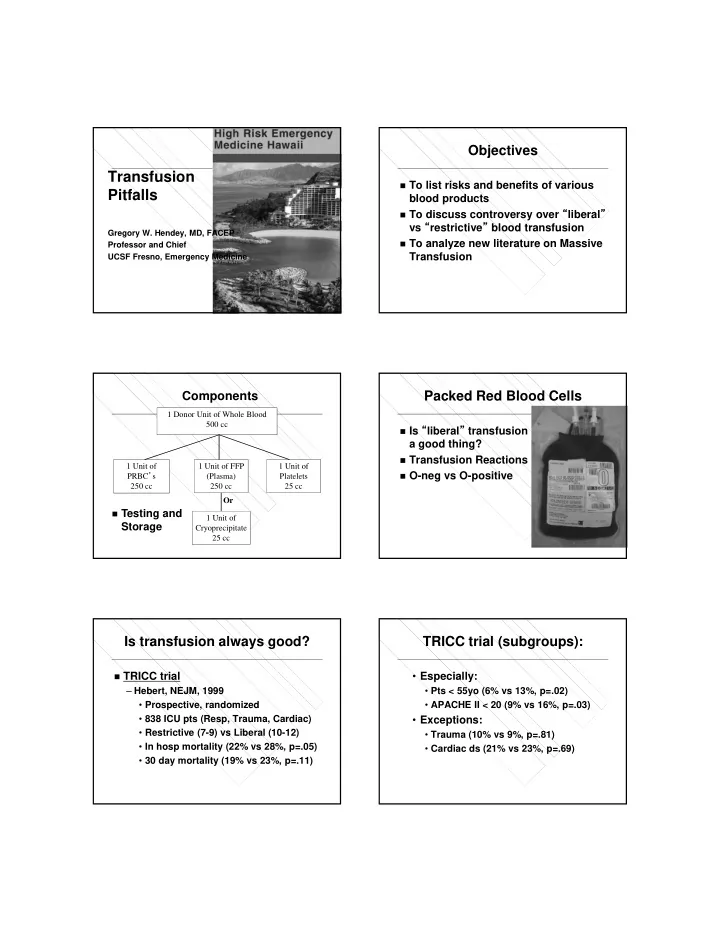
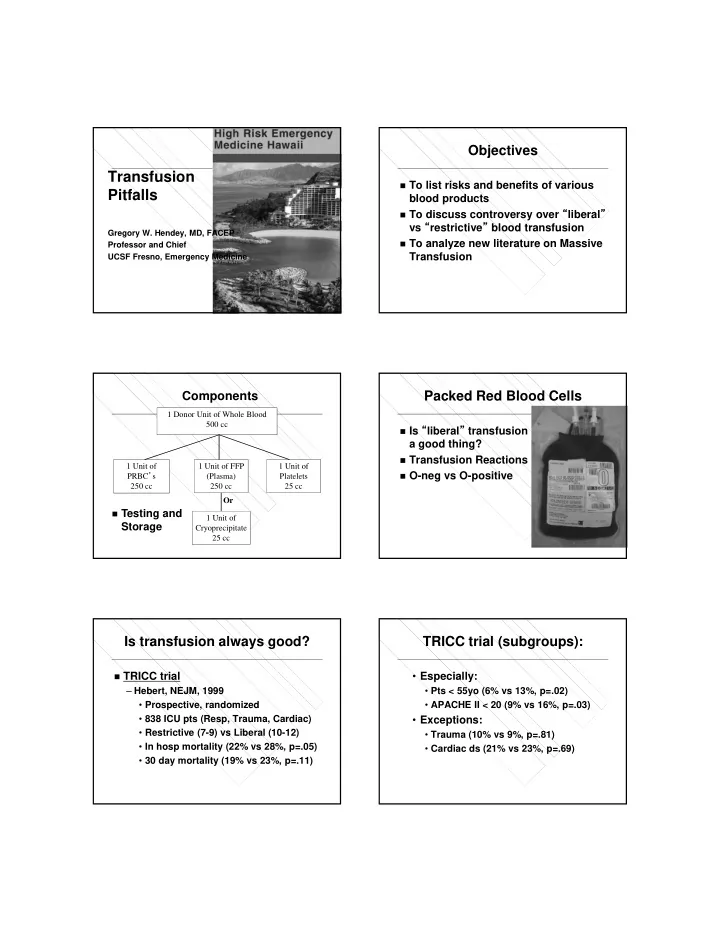
Objectives Transfusion To list risks and benefits of various Pitfalls blood products To discuss controversy over “ liberal ” vs “ restrictive ” blood transfusion Gregory W. Hendey, MD, FACEP To analyze new literature on Massive Professor and Chief Transfusion UCSF Fresno, Emergency Medicine Packed Red Blood Cells Components 1 Donor Unit of Whole Blood 500 cc Is “ liberal ” transfusion a good thing? Transfusion Reactions 1 Unit of 1 Unit of FFP 1 Unit of O-neg vs O-positive PRBC ’ s (Plasma) Platelets 250 cc 250 cc 25 cc Or Testing and 1 Unit of Storage Cryoprecipitate 25 cc Is transfusion always good? TRICC trial (subgroups): TRICC trial • Especially: – Hebert, NEJM, 1999 • Pts < 55yo (6% vs 13%, p=.02) • Prospective, randomized • APACHE II < 20 (9% vs 16%, p=.03) • 838 ICU pts (Resp, Trauma, Cardiac) • Exceptions: • Restrictive (7-9) vs Liberal (10-12) • Trauma (10% vs 9%, p=.81) • In hosp mortality (22% vs 28%, p=.05) • Cardiac ds (21% vs 23%, p=.69) • 30 day mortality (19% vs 23%, p=.11)
Non-randomized studies: Why would it be bad? CRIT trial Hemolysis – Corwin, Crit Care Med , 2004 Anaphylaxis Oxygen delivery – 4,892 ICU pts, prospective HIV, HCV Volume expansion observational Volume overload Coagulation – 44% were transfused, mean 5 units TRALI – Txn independently assoc with incr mort TRIM Several studies in Trauma, Critical Care – More transfusion = higher mortality Selection bias? Minor Transfusion Reactions: Severe Transfusion Reactions: Acute hemolysis Simple febrile (1%) – ABO error (non ABO) – Antibody vs donor Leukocyte antigens – 1 in 250K – Acetaminophen Anaphylaxis Simple allergic (0.1%) – Congenital IgA deficiency – Antibody vs donor plasma proteins – 1 in 150K Bacterial contamination – Diphenhydramine – Plts > PRBC – Babesia microti, S. aureus – 1 in 2-10K Delayed Transfusion Transfusion Fatalities Reactions: 2007-11 FDA data HIV – 1 in 1 million Hepatitis B – 1 in 137K Hepatitis C – 1 in 1 million Graft vs Host disease
TRALI Transfusion-related Acute Lung Injury TRALI 1 in 5K. FFP > PRBC > Plts – Transfusion related acute lung injury 50% transfusion related deaths TACO Immune-related, donor antibodies vs – Transfusion assoc circulatory overload patient WBC ’ s cytokines TRIM Prevention: – Transfusion related immunomodulation – Reduce female plasma donors TGIF Non-cardiogenic pulmonary edema – Thank God it ’ s Friday! TRIM Overload vs TRALI (Transfusion Related Immunomodulation) Immunosuppression, inflammatory PRBC FFP > PRBC – WBC ’ s and mediators (cytokines, IL) Cardiomegaly Normal Benefit: organ transplant survival High wedge/CVP Normal / low Harm: High BP Normal / low BP – Recurrence of malignancies – Pneumonia, post-op infections NTG, Diuresis Supportive – Increased mortality Prevention: Leukoreduction Is Old blood Bad blood? **So what should I do?** Storage lesion Napolitano, CCM and J Trauma , 2009: pH, K, free Hgb – Guideline from ACCCM and EAST – Txn indicated for hemorrhagic shock Might scavenge nitric oxide – Restrictive strategy (Hgb<7) for stable – NO vasodilates for tissue perfusion anemia (except ACS) Multiple studies: worse outcomes – Sepsis: EGDT 1st 6 hrs (Hgb 10) – Cardiac surg, Trauma, Critical care • Then Restrictive (Hgb 7) Multiple studies: no difference
CCM / Trauma Guideline (cont.) EXAMPLE – One unit at a time 50 yo M alcoholic, GI bleeding, BP 80/40, HR 130, Hgb 8.1 • Except acute hemorrhage – Must also consider clinical indicators Should I transfuse, or use restrictive trigger of Hgb<7? » Hemodynamics, ongoing loss TRANSFUSE – Txn incr risk of Infxn, SIRS, ARDS – Acute hemorrhage – Hemodynamically compromised 2 Units of O-negative, Stat! O+ blood transfusion O-neg to women of childbearing age Dutton, J Trauma , 2005: – Alloimmunization – Maryland Shock Trauma, one year – Hemolytic disease of newborn – O- to young women, O+ all others O-positive to men, older women – 581 units type O to 161 patients – Tiny chance of hemolysis if Rh negative – No transfusion reactions – Future emergency transfusion – One Rh- male developed Ab Type and Screen vs Massive transfusion Type and Cross Definition: T&S: test for atypical Ab in serum – Entire blood volume in 24 hrs T&C: mix pt serum and donor RBCs (75 cc/kg, 5L, 10 units PRBC) Electronic cross matching – 5 units in 3 hrs + ongoing hemorrhage Problems: – Coagulopathy, DIC – Hypothermia – Acidosis – Hypocalcemia (citrate toxicity)
Coagulopathy: Ho, Can J Surg , 2005: Multi-factorial Mathematical model – Dilution – Ongoing loss, various ratios of transfxn – Hypothermia, acidosis Assumptions: 2 approaches: – 30% blood loss, IVF, 2 U PRBC – 1) treat problems as they arise – Clotting factors already 50% – 2) treat prophylactically (Protocol) Only way to maintain or “ catch up ” is • 5 PRBC / 5 U FFP / 1 apheresis Plts 1:1 or higher (more FFP) • Approximates Whole blood No randomized trials Ho, Can J Surg , 2005 (cont): Vary PRBC:FFP 3:1, 2:1, 1:1 Only way to maintain or “ catch up ” is 1:1 or higher (more FFP) Borgman, J Trauma , 2007: Holcomb, Ann Surg , 2008: Retro, 246 pts, > 10 U PRBC Retro, 466 massive transfusion pts Higher FFP:PRBC, higher survival High FFP:PRBC ratio (>1:2) vs low Low ratio (1:8) Survival 35% 30 day survival: 60% vs 40% High ratio (1:1.4) Survival 81% Same effect with Plt:PRBC ratio Supports 1:1 massive transfusion Recommended 1:1:1
Massive Transfusion Pack Summary 5 U PRBC (O-negative) Transfusion indications and controversies 5 U FFP (AB, pre-thawed) Transfusion reactions 1 U Apheresis Platelets Massive Transfusion Thank you! And don’t worry . . . All bleeding eventually stops!
Recommend
More recommend