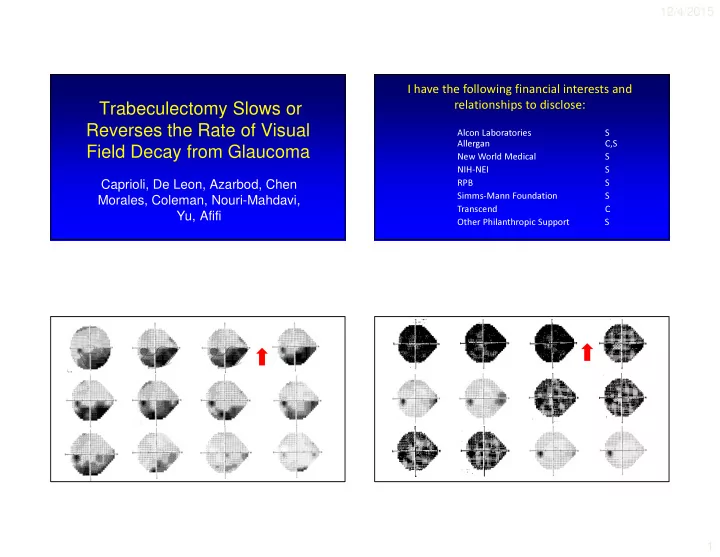
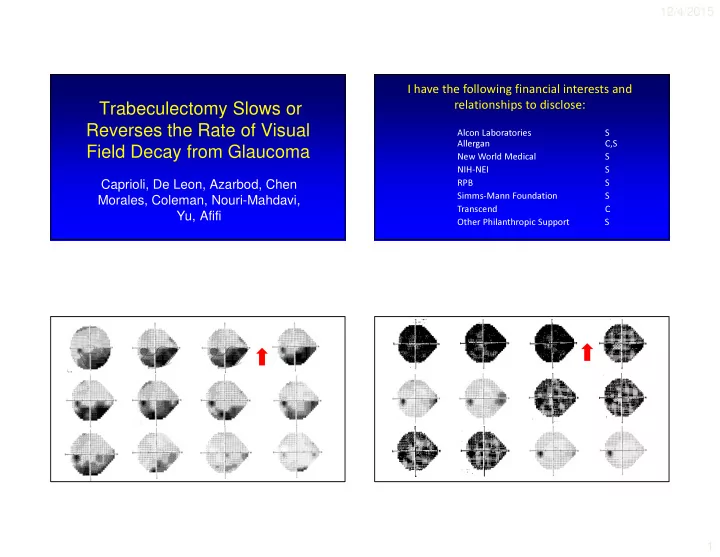
12/4/2015 I have the following financial interests and Trabeculectomy Slows or relationships to disclose: Reverses the Rate of Visual Alcon Laboratories S Allergan C,S Field Decay from Glaucoma New World Medical S NIH-NEI S Caprioli, De Leon, Azarbod, Chen RPB S Morales, Coleman, Nouri-Mahdavi, Simms-Mann Foundation S Transcend C Yu, Afifi Other Philanthropic Support S 1
12/4/2015 VF Improvement After Surgery: My Clinical Observations • Not a rare phenomenon • Not a learning effect • Acute reduction IOP with Diamox: • Can ’ t exclude acute pharmacologic events • Robust decrease in IOP Improvements with manual static perimetry • IOP often high pre-op • Damage not too bad independent of disease • Patients not too old Trans Am Acad Ophthalmol Otol 1974 • “ Unless improvement is noted to accompany • Relationship between IOP and VF damage • PERG, short term be…assured ” • RGC function partially restored after IOP reduction in glaucomatous eyes with early VF impairment lowering of IOP, adequacy of control cannot • No improvement in eyes with normal VF Trans Ophthalmol Soc UK 1985 Ophthalmol 2005 2
12/4/2015 • Substantial VF improvement at 5 years • Short term, 3 months • ∆ MD used as outcome, no rates • ∆ in TD and PSD probability maps used • IOP reduction associated with VF • No rates improvement • “Biomarker” for RGC response to treatment* Am J Ophthalmol 2014 Am J Ophthalmol 2015 Approach Problems to overcome: • Measure change in rates of individual VF test • Signal/Noise; Variability Many tests, Fitted trend, locations before and after trabeculectomy Comparison group • Regression to mean – Long-term (years) Experience – Allow for decaying or improving rates • Learning effect Magnitude of change – Retain spatial information • Media effects Comparison group • Comparison Group, help control for – Cataract Magnitude of change – Noise No cataract surgery – Ocular surface – Regression to the mean 3
12/4/2015 Background Trabeculectomy Group • Open-angle glaucoma • ≥ 4 VFs before AND after surgery • ≥ 2 years before AND after surgery • No intercurrent cataract surgery • Absence of other VF causes IOVS, 2011,2012, and 2014 Comparison Group Methods • Open angle glaucoma • Pointwise exponential regression – No intercurrent glaucoma or cataract surgery • Allow for decay or improvement within testing boundaries, with (-) or (+) rates – Clinically “stable”, no ∆ number meds • Group analyses: • NOT a “treatment control” ! – Trabeculectomy group: pre and post surgery • ≥ 8 VFs, ≥ 4 years – Comparison group: pre and post “mock surgery” – “Mock surgery” at half follow-up • Entire analysis repeated with: – Rates fit for first and second half of follow-up – Linear model (PLR) – Requirement for tighter fits (p < .10) 4
12/4/2015 Methods Upper limit of age and location matched normal value • Rates at each location • Counts of decay and improving • Locations of decay and improving • Multivariate regression of potential factors Lower limit of associated with improving perimetric testing, 0 dB 5
12/4/2015 Pre- and Post- Op IOP Trabeculectomy Group Trabeculectomy Group Comparison Group Number of eyes 74 71 Number of patients 65 55 Age (mean ± SD) 61.4 ± 12.6 62.5 ± 10.0 Mean 10.0 ± 3.6 Mean 14.3 ± 2.9 1 st half 2 nd half Pre Post 5.1 ± 2.1 5.4 ± 2.3 5.1 ± 2.0 5.0 ± 1.7 Number of VF’s ± SD 8.9 ± 4.7 9.0 ± 4.4 5.7 ± 2.7 6.2 ± 2.6 VF follow-up duration Initial MD (mean ± SD) -7.2 ± 5.3 -5.6 ± 4.3 Final MD (mean ± SD) -10.7 ± 6.4 -8.2 ± 5.1 x x x x x Gray scale of Rates x x x x 6
12/4/2015 Decay followed by Improvement What about eyes? Proportion of eyes with ≥ 5 more 80% locations improving post op: Proportion of eyes with ≥ 10 more 57% Improvement followed by Decay locations improving post op: Difference from Comparison Group: p = 0.0000 Χ 2 for exp, linear, or only best fits Multivariate Analysis for Number of improving locations as a N Improving (post-pre) Improvement (Trabeculectomy) More VF improvement function of IOP reduction after surgery • Age (baseline) p = 0.76 • MD (baseline) p = 0.83 r = 0.33 • VFI (baseline) p = 0.65 p = 0.001 • ∆ IOP p = 0.009 More IOP reduction IOP (post – pre) 7
12/4/2015 Summary • Trabeculectomy slows or reverses glaucomatous VF damage • Reversal of rates from decay to improvement is common • Duration of improvement is years • The proportion of points improving post-op depends on the magnitude of IOP reduction • Similar results with linear model and requirement for tighter fits Ophthalmology 2015 Clinical Research Team Implications Authors Others • Robust IOP reduction can reverse glaucomatous • Niloufar Abdollahi • Niloufar Abdollahi • Abdolmonem Afifi visual loss! • Elena Bitrian • Elena Bitrian • Parham Azarbod • Hypothesis: Sick but not dead RGCs • Nila Cirineo • Nila Cirineo • Joseph Caprioli • Prolonged agonal period • Joon Mo Kim • Joon Mo Kim • Anne Coleman • Opportunity for intervention • Ji Woong Lee • Ji Woong Lee • Mark De Leon • Reversal of VF loss should be a goal of treatment * • Junmo Lee • Junmo Lee • Regional indices more meaningful than global • Esteban Morales indices (MD, VFI) when used as treatment outcome • Dennis Mock • Dennis Mock • Kouros Nouri-Mahdavi measure • Meera Ramanathan • Meera Ramanathan • Fei Yu 8
Recommend
More recommend