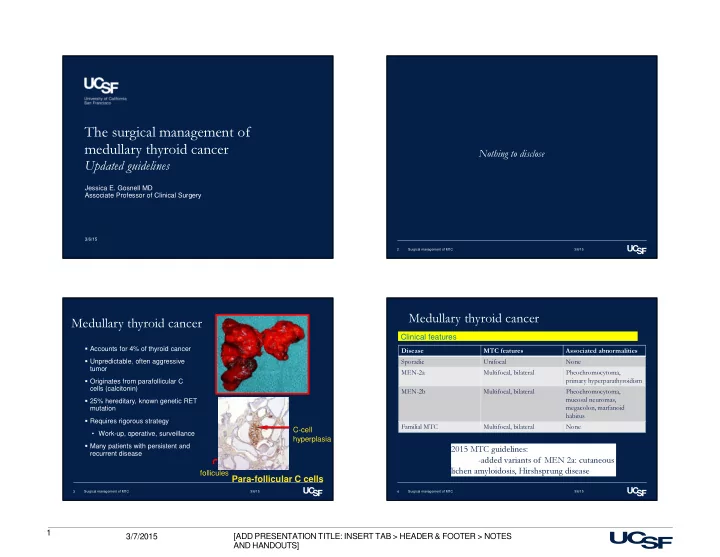
The surgical management of medullary thyroid cancer Nothing to disclose Updated guidelines Jessica E. Gosnell MD Associate Professor of Clinical Surgery 3/6/15 2 Surgical management of MTC 3/6/15 Medullary thyroid cancer Medullary thyroid cancer Clinical features � Accounts for 4% of thyroid cancer Disease MTC features Associated abnormalities � Unpredictable, often aggressive Sporadic Unifocal None tumor MEN-2a Multifocal, bilateral Pheochromocytoma, � Originates from parafollicular C primary hyperparathyroidism cells (calcitonin) MEN-2b Multifocal, bilateral Pheochromocytoma, � 25% hereditary, known genetic RET mucosal neuromas, mutation megacolon, marfanoid habitus � Requires rigorous strategy C-cell Familial MTC Multifocal, bilateral None • Work-up, operative, surveillance hyperplasia � Many patients with persistent and 2015 MTC guidelines: recurrent disease -added variants of MEN 2a: cutaneous follicules lichen amyloidosis, Hirshsprung disease Para-follicular C cells 3 Surgical management of MTC 3/6/15 4 Surgical management of MTC 3/6/15 1 3/7/2015 [ADD PRESENTATION TITLE: INSERT TAB > HEADER & FOOTER > NOTES AND HANDOUTS]
Preoperative work-up: clinical disease Clinical disease � Extent of disease � Hereditary disease • Hx/ exam • RET mutational analysis • Calcitonin/CEA level • Calcium, iPTH, fractionated plasma metanephrines,24- • Neck ultrasound Disease diagnosed by genetic test hour urine metanephrines and normetanephrines • laryngoscopy Recurrent disease 2015 MTC guidelines: -Rule out pheochromocytoma. If present, resect the pheo first after appropriate preoperative preparation, prior to surgery for MTC 5 Surgical management of MTC 3/6/15 6 Surgical management of MTC 3/7/2015 Preoperative work-up: clinical disease 63yo man � Calcitonin levels (2009 guidelines) ‒ <400 pg/ml -> high resolution neck ultrasound ‒ >400 pg/ml -> metastatic workup Revised 2015 MTC guidelines: Calcitonin 308 (<2) >500pg/ml or N1 disease -> chest CT, neck CEA 19 (<5) CT and 3-phase contrast enhanced CT abdomen, or contrast enhanced MRI 7 Surgical management of MTC 3/7/2015 8 Surgical management of MTC 3/6/15 2 3/7/2015 [ADD PRESENTATION TITLE: INSERT TAB > HEADER & FOOTER > NOTES AND HANDOUTS]
Surgical management of MTC: clinical disease “ Overall, the rate of persistent � Lack of effective adjuvant therapy hypercalcitoninemia is nearly 50% for � Aggressive patients with nonpalpable macroscopic disease � Difficult to cure biochemically and greater then 80% for patients presenting � Patient often live with disease for decades with a palpable MTC.” Surgical risk Completeness of resection Van Heerden et al Annals of Surgery, 2000 9 Surgical management of MTC 3/6/15 10 Surgical management of MTC 3/7/2015 Surgical management of MTC: clinical Surgical management of MTC: clinical disease disease � Total thyroidectomy & Lymph node dissection Cervical lymph nodes � Central neck • Hyoid to inominate, 2009/2015 MTC guidelines: between the carotid sheaths � Left and right lateral neck Total thyroidectomy • Lateral to the vessels, divided into submandibular, parajugular and posterior Sporatic MTC – 20% bilateral triangle Hereditary MTC- 90% 11 Surgical management of MTC 3/7/2015 12 Surgical management of MTC 3/7/2015 3 3/7/2015 [ADD PRESENTATION TITLE: INSERT TAB > HEADER & FOOTER > NOTES AND HANDOUTS]
High incidence of lymph node metastases in Surgical management of MTC: clinical patients with MTC disease � Over 50% involvement of cervical lymph nodes � Central lymph node dissection � Moley et al: 81% of central lymph nodes involved in patients with unilateral tumors 2009/2015 MTC guidelines: In patients with no evidence of advanced local disease, no evidence of cervical lymph metastasis on PE or US and no distant mets, patients should undergo Total tx and prophylactic VI neck dissection (Moley, Ann Surg 1999;240:1000) 13 Surgical management of MTC 3/7/2015 14 Surgical management of MTC 3/7/2015 Surgical management of MTC: clinical Surgical management of MTC: clinical disease METASTASES COMMON! disease Machens et al, Cancer 2000 � Unilateral lateral neck involvement • No cLNs 10% • 1-3 +cLNs 77% • >4 +cLNS 98% � Contralateral lateral neck involvement • No cLNs 5% • 1-9 +cLNs 38% • >10 +cLNS 77% LATERAL LYMPH NODE DISSECTION (II, III, IV, V) CENTRAL LYMPH NODE DISSECTION (VI, VII) 15 Surgical management of MTC 3/7/2015 16 Surgical management of MTC 3/7/2015 4 3/7/2015 [ADD PRESENTATION TITLE: INSERT TAB > HEADER & FOOTER > NOTES AND HANDOUTS]
Surgical management of MTC: clinical Surgical management of MTC: clinical disease disease � Compartment-based � Lateral neck lymph node dissection approach (no berry picking) 2009 MTC guidelines: � Image and biopsy driven � Preservation of vital structures Selective approach: not prophylactic, but � Modify extent based on Therapeutic (image-guided) metastatic load Revised 2015 MTC guidelines: (Robbins et al, Arch OHNS 1991) LATERAL LYMPH NODE DISSECTION (II, III, IV, V) No consensus 17 Surgical management of MTC 3/7/2015 18 Surgical management of MTC 3/7/2015 Surgical management of MTC (genetic) Ultra sound with lymph node mapping � An increasing proportion of patients with MTC are now identified by genetic testing 19 Surgical management of MTC 3/7/2015 20 Surgical management of MTC 3/6/15 5 3/7/2015 [ADD PRESENTATION TITLE: INSERT TAB > HEADER & FOOTER > NOTES AND HANDOUTS]
Genotype-phenotype Genetic testing for MTC correlation RET codon mutation � Identifies at-risk kindred � Obviates need for lifelong surveillance for Codon 634 most gene-negative patients common • Pheochromocytoma, primary HPT � Allows prophylactic/preclinical thyroidectomy in gene-positive patients • Durable biochemical cure � May help “tailor” operative approach parathyroids RET proto-oncogene 21 Surgical management of MTC 3/6/15 22 Surgical management of MTC 3/6/15 2001 Guidelines 2009 Guidelines � Level I (least high risk) • Total tx <10yrs or when pentagastrin stimulated calcitonin elevated � Level II (611,618, 620, 634) • Total tx <5yrs � Level III (918, 883) • Total tx < 6 months (Brandi et al, JCEM 2001) (Kloos RT et al, Thyroid 2009) 23 Surgical management of MTC 3/6/15 24 Surgical management of MTC 3/6/15 6 3/7/2015 [ADD PRESENTATION TITLE: INSERT TAB > HEADER & FOOTER > NOTES AND HANDOUTS]
2015 Guidelines 2015 Guidelines � ATA-highest � ATA-highest � ATA highest � Central neck • Thyroidectomy <1yr • If suspicious LNs-> CLND, dissection (level VI) consider only if parathyroids • -918 � ATA- high and be preserved � ATA high • Thyroidectomy <5 or earlier � ATA- high and moderate based on calcitonin levels, in • 634 consultation with family • CLND if calcitonin > 40 or � ATA moderate clinical evidence of mets � ATA- moderate • All others! • Timing of thyroidectomy should be based on calcitonin levels, in consultation with family, consider about age 5yrs 25 Surgical management of MTC 3/6/15 26 Surgical management of MTC 3/6/15 Preoperative work-up A note about parathyroid glands: beware and have a plan Patients presenting with genetic mutation � Sporadic MTC � Extent of disease (MTC) • Preserve parathyroids (uppers), autotransplant if necessary • High resolution neck ultrasound � Genetic disease • Calcitonin level • No primary hyperparathyroidism • CEA level ‒ identify and preserve parathyroids � Evaluate for other endocrinopathies • Primary hyperparathyroidism • PTH, calcium ‒ Resect abnormal glands (vs subtotal), use IOPTH • fractionated plasma metanephrines, 24- hour urine ‒ If low risk for recurrent MTC-> SCM ok for autotransplant metanephrines and normetanephrines ‒ If higher risk for recurrent MTC-> forearm autotransplant 27 Surgical management of MTC 3/6/15 28 Surgical management of MTC 3/6/15 7 3/7/2015 [ADD PRESENTATION TITLE: INSERT TAB > HEADER & FOOTER > NOTES AND HANDOUTS]
Recommend
More recommend