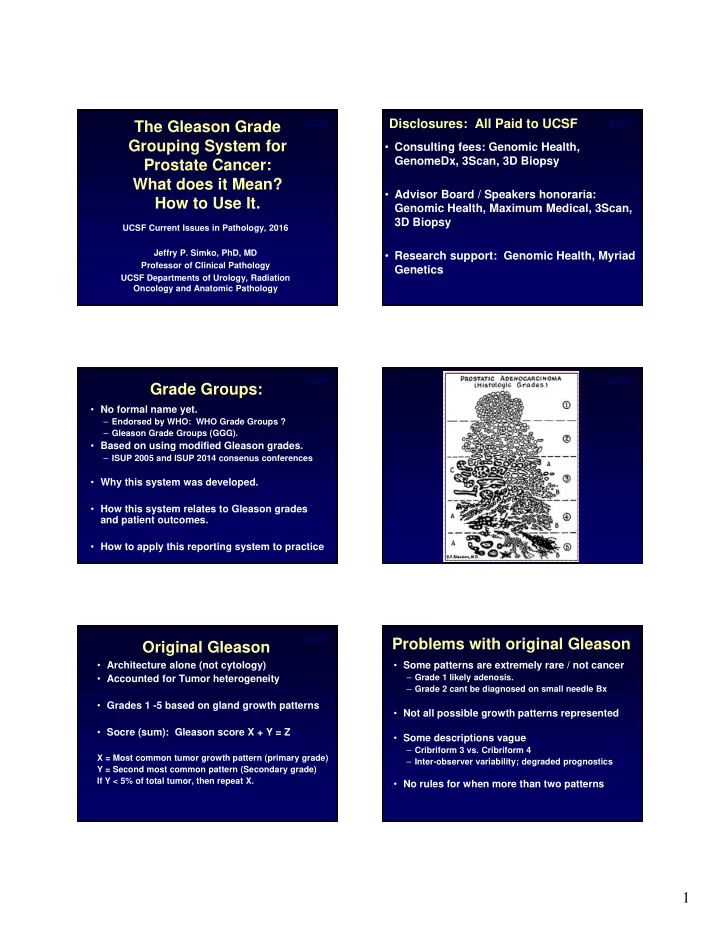
Disclosures: All Paid to UCSF UCSF UCSF The Gleason Grade Grouping System for • Consulting fees: Genomic Health, GenomeDx, 3Scan, 3D Biopsy Prostate Cancer: What does it Mean? • Advisor Board / Speakers honoraria: How to Use It. Genomic Health, Maximum Medical, 3Scan, 3D Biopsy UCSF Current Issues in Pathology, 2016 Jeffry P. Simko, PhD, MD • Research support: Genomic Health, Myriad Professor of Clinical Pathology Genetics UCSF Departments of Urology, Radiation Oncology and Anatomic Pathology UCSF UCSF Grade Groups: • No formal name yet. – Endorsed by WHO: WHO Grade Groups ? – Gleason Grade Groups (GGG). • Based on using modified Gleason grades. – ISUP 2005 and ISUP 2014 consenus conferences • Why this system was developed. • How this system relates to Gleason grades and patient outcomes. • How to apply this reporting system to practice UCSF UCSF Problems with original Gleason Original Gleason • Architecture alone (not cytology) • Some patterns are extremely rare / not cancer – Grade 1 likely adenosis. • Accounted for Tumor heterogeneity – Grade 2 cant be diagnosed on small needle Bx • Grades 1 -5 based on gland growth patterns • Not all possible growth patterns represented • Socre (sum): Gleason score X + Y = Z • Some descriptions vague – Cribriform 3 vs. Cribriform 4 X = Most common tumor growth pattern (primary grade) – Inter-observer variability; degraded prognostics Y = Second most common pattern (Secondary grade) If Y < 5% of total tumor, then repeat X. • No rules for when more than two patterns 1
Gleason Modifications: ISUP UCSF UCSF Gleason Modifications: ISUP • Do not use Grades 1 or 2 (or use very sparingly) • International Society of Urologic Pathologists • All carcinomas with cribriform growth = 4 Consensus Meetings: 2005, 2014 – Glomerulations = 4 but outcome data not in yet. • Certain patterns (grades) better classified: – Dozens of prostate pathologists at the meetings Gleason growth pattern actually better than specific grades for some tumor morphologies. • Treating clinicians also attended the 2014 meeting – Identify common areas: Consensus statements – Tumor glands floating in mucin (mucinous carcinoma not all 4) – Tumor with columnar cells (Ductal Ca) not always 4 – Identify areas of confusion: Experiments to clarify – Tumor cells with vacuoles seen in Gleason patterns 3, 4 or 5. – Criticized at the time for no outcome data • Scoring rules changed to better represent biology – In Bx, primary grade + worst = score, not secondary • Outcome studies have now validated most – In Bx, if secondary lower grade and < 5%, ignore it. • Increased consistency in grading • Prostatectomy, score discreet tumors of different grades separately. • Recommend reporting percent tumor > pattern 3. UCSF UCSF Clinical Problems: • ”BEST” score now 3+3=6 on scale 2-10. – Confusing to patients – Difficult to explain – Patient anxiety precluding conservative management • (patient and clinician frustration) • 3+4=7 and 4+3=7 same score, but very different outcome!!! PROSTATECTOMY UCSF UCSF Pierorazio, et al. Br J Urol Int 111: 753-60 (2013). Pierorazio, et al. Br J Urol Int 111: 753-60 (2013). 2
How to apply Grade Groups: UCSF UCSF Grade Groups (Epstein): • Use ISUP modified Gleason Grades works best • Grade Group 1 = Gleason score < 7 • Grade Group 2 = Gleason score 3+4 = 7 • Use Biopsy with highest score • Grade Group 3 = Gleason score 4+3 = 7 – Subsequent study showed that using overall Bx grade group or highest Bx grade group gave similar prognosis • Grade Group 4 = Gleason score 8 (4+4, 3+5, 5+3) (Berney et al., Br J Cancer Apr 21, 2016 epub) • Grade Group 5 = Gleason score > 8 (4+5, 5+4, 5+5) • Prostatectomy: If Grade 5 > 5%, then secondary • Validated in numerous f/u studies – Does not strictly follow ISUP, but makes biologic sense – Probably works either way. • Endorsed by WHO • Simple translation from Gleason score to GGG – Clinicians can easliy translate to grade groups • UCSF Data: 4+4, 4+5, 5+4 same, 5+5 worse (unpubl) – Keeps report cleaner / less confusion Future Directions: UCSF UCSF That’s all Folks!!!!! • Simple system to report meaningful grade info. – Independent validations done – Improve communication with patients – Grade compression not compromising prognostics • Some tumor growth patterns still need improved correlation with outcome data – Glomeruations – Discriminating some patterns of 4 from 5 difficult – Stromal changes as a prognostic factor 3
Recommend
More recommend