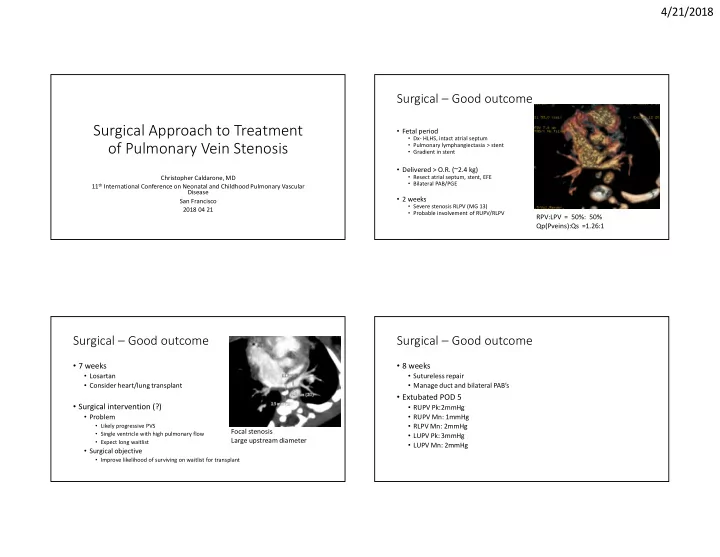
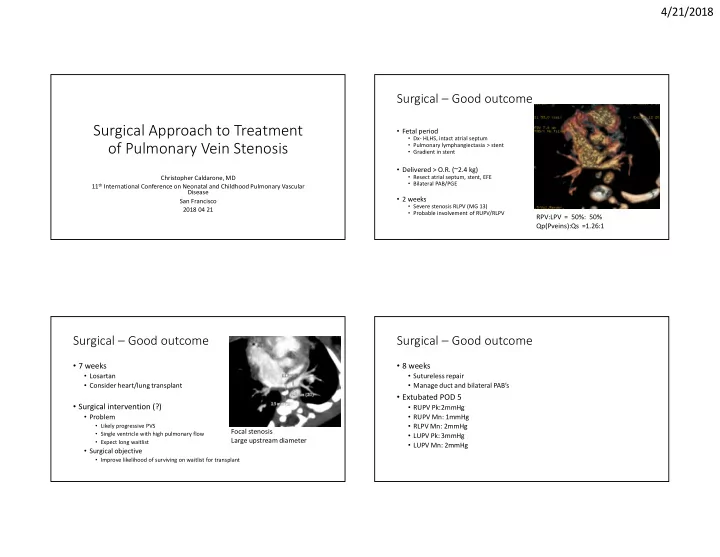
4/21/2018 Surgical – Good outcome Surgical Approach to Treatment • Fetal period • Dx- HLHS, intact atrial septum of Pulmonary Vein Stenosis • Pulmonary lymphangiectasia > stent • Gradient in stent • Delivered > O.R. (~2.4 kg) • Resect atrial septum, stent, EFE Christopher Caldarone, MD • Bilateral PAB/PGE 11 th International Conference on Neonatal and Childhood Pulmonary Vascular Disease • 2 weeks San Francisco • Severe stenosis RLPV (MG 13) 2018 04 21 • Probable involvement of RUPV/RLPV RPV:LPV = 50%: 50% Qp(Pveins):Qs =1.26:1 Surgical – Good outcome Surgical – Good outcome • 7 weeks • 8 weeks • Losartan • Sutureless repair • Consider heart/lung transplant • Manage duct and bilateral PAB’s • Extubated POD 5 • Surgical intervention (?) • RUPV Pk:2mmHg • Problem • RUPV Mn: 1mmHg • Likely progressive PVS • RLPV Mn: 2mmHg Focal stenosis • Single ventricle with high pulmonary flow • LUPV Pk: 3mmHg Large upstream diameter • Expect long waitlist • LUPV Mn: 2mmHg • Surgical objective • Improve likelihood of surviving on waitlist for transplant 1
4/21/2018 Surgical – Good outcome Surgical – Good outcome • 3 months • Favorable pulmonary vein anatomy ….No change • PDA stented, transfer to home • Expectation of recurrent disease • Plan to list for transplant when recurrence evident Surgical – Good outcome Surgical – Good outcome (?) • One year 7 months • Qp/Qs = 0.6 • Norwood • LPA small > stent • 4mm central BT shunt (Ab RSCA) • Pulmonary veins OK • Resection of RUPV and RLPV scars (?) • Unobstructed pulmonary veins on postop TEE • 15 months • Extensive pulmonary artery plasty • BCPS • Arch reconstruction with interposition • Pulmonary veins OK • Mediastinitis 2
4/21/2018 Learning points Learning points • Upstream diameters are important • Upstream diameters are important • Worst substrate • Worst substrate • Single ventricle - High flow pulmonary veins • Single ventricle - High flow pulmonary veins • Fetal pulmonary venous hypertension • Fetal pulmonary venous hypertension • But – large upstream vessels • But – large upstream vessels LoRito, JTCVS 2016 Learning points Learning points • Sutureless repairs best for local disease and complex geometry • Sutureless repairs best for local disease and complex geometry • Poor outcomes with congenital PVS Viola, JTCVS 2011 3
4/21/2018 Learning points Learning points • Sutureless repairs are best for local disease and complex geometry • Sutureless repairs best for local disease and complex geometry • Good outcomes with pre-op obstruction • Good outcomes with mixed TAPV • n=768 Honjo, Ann Thos Surg 2010 Shi, Circulation 2017 Learning points Surgical – Poor outcome • 2 months • Sutureless repairs best for local disease and complex geometry • Cor triatriatum, Anomalous drainage LUPV • O.R. • Post-repair PVS • Resection of the cor triatriatum membrane • Sutureless repair of atrial junction with LLPV • LUPV branch to VV to innominate • Kalfa – AATS 2017 – in press • 6 months postop • N=75, 14 centers • RUPV pg 1; mg 0 • PVS score risk adjustment • RLPV pg 4; mg 1 • LUPV to VV to inomminate vein; no obstruction • Sutureless repair > less reoperation/reintervention • LLPV pg 6; mg 2 Kalfa, JTCVS, in press 4
4/21/2018 Surgical – Poor outcome Surgical – Poor outcome • 15 months postop • LUPV to vertical vein and innominate vein • LLPV severely narrowed • Flow • Anomalous LUPV: 2.1 L/min/m2 • LLPV: 0.18 L/min/m2 • Qp:Qs =1.67:1 • RPA:LPA = 63%:27% • Cath lab, dilation, cutting balloon – minimal improvement Good surgical substrate Surgical – Poor outcome Surgical – Poor outcome • Options: • Options: • No operation • Repair LLPV and attach LUPV to LA 2.1 L/min/m2 RISK Left Lung Left Lung Right Left Right Left atrium atrium atrium atrium RISK 0.2 L/min/m2 5
4/21/2018 Surgical – Poor outcome Surgical – Poor outcome • One month postop • Options: • LLPV pg 11mmHg • Repair LLPV • LLPV mg 4mmHg • 4 months postop 2.1 L/min/m2 • Narrow/occluded LLPV • Interstitial edema/lymphangiectasia • Areas of segmental collapse or venous infarction Left Lung Right Left atrium atrium RISK Learning points Learning points • Flow redistribution • Competing flow can jeopardize an anastomosis • Can be high volume! • Introduces error in echo gradients • False security 2.1 L/min/m2 • Implications for surgical decisions Left Lung Right Left atrium atrium RISK Chiu, Phys Rev, 2011 Greenway , J Cardiovasc Mag Res 2011 6
4/21/2018 Learning points • LUPV anastomosis can cause problems! Don’t poke a skunk…. Kotani, Ann Thor Surg 2013 Sampling bias Sampling bias • Small samples – weak evidence • Who is Henri Justino? • Not always representative • Test a research question: • Who is Henri Justino? • Methodology: 7
4/21/2018 Sampling bias Sampling bias • Who is Henri Justino? • Who is Henry Justino? Is this representative of truth? Bearded? 1/6 >Not representative Further study required! Combined surgical/cath-based therapy Sampling bias • Who is Henri Justino? Is this representative of truth? Conclusions: Frequency of incarceration : 8/14 images Dr Justino is fond of orange jumpsuits Future study: What is Dr Justino doing in Hays County? In-stent restenosis: 50% @ 1 year Balasubramanian, Circ 2012 8
4/21/2018 Combined surgical/cath-based therapy Combined surgical/cath-based therapy Better performance > 7mm Survival: 50-60% @ 3 years Balasubramanian, Circ 2012 Balasubramanian, Circ 2012 Lung transplant and PVS 5yr survival: 60% ECMO was main predictor of 1 year mortality Bharat, J HeartLungTransplant 2013 9
4/21/2018 Sutureless repairs Mavroudis / Pediatric Cardiac Surgery 5th Edition JS Most recent Most recent JS 10
4/21/2018 JS Most recent 11
Recommend
More recommend