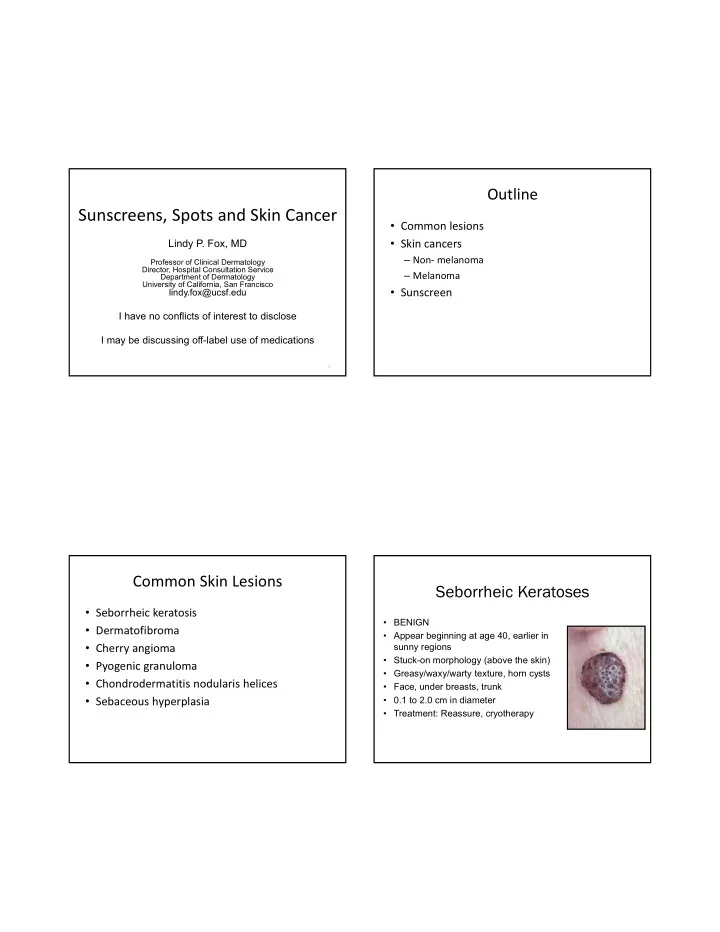
Outline Sunscreens, Spots and Skin Cancer • Common lesions • Skin cancers Lindy P. Fox, MD – Non‐ melanoma Professor of Clinical Dermatology Director, Hospital Consultation Service – Melanoma Department of Dermatology University of California, San Francisco • Sunscreen lindy.fox@ucsf.edu I have no conflicts of interest to disclose I may be discussing off-label use of medications 1 Common Skin Lesions Seborrheic Keratoses • Seborrheic keratosis • BENIGN • Dermatofibroma • Appear beginning at age 40, earlier in • Cherry angioma sunny regions • Stuck-on morphology (above the skin) • Pyogenic granuloma • Greasy/waxy/warty texture, horn cysts • Chondrodermatitis nodularis helices • Face, under breasts, trunk • Sebaceous hyperplasia • 0.1 to 2.0 cm in diameter • Treatment: Reassure, cryotherapy
Dermatofibroma • Firm, 3‐7 mm slightly rough surfaced, slightly elevated papules • Overlying hyperpigmentation • Firm to palpation; Dimple sign • Often at sites of minimal trauma – Bug bite, ingrown hair, etc • Treatment : Reassure, cryotherapy, removal • Often recur after removal • Association: Multiple (>15) of sudden onset may rarely signal T cell dysregulation (Lupus, HIV) Cherry Angioma • Very Common • Increases with age (senile angioma) • F>M (?hormonal) • 1‐5 mm bright red dome‐shaped papule • Not easily compressible • Association: None • Complications: None
Pyogenic Granuloma • Friable, 5‐10 mm papule • Occurs after trauma • Children and adults • Biopsy: Excess granulation tissue • Treatment: Surgical removal (curette), electrodesiccation of base, topical timolol? • Complication: Rarely may recur and form satellites Chondrodermatitis Nodularis Helices • Benign nflammation of the cartilage of the helix or antihelix • Middle aged men • Painful! • “can’t sleep on that side” • May mimic NMSC • Treatment – Relieve pressure, surgical removal, time – LN2, IL kenalog, laser therapy
“CNH pillow” Sebaceous Hyperplasia • Common, benign • Single or multiple pink to yellow papules on the face, often with telangiectasias and central dell • May mimic BCC • Multiple associated with calcineurin inhibitors • When associated with sebaceous adenoma or sebaceous carcinoma, rule‐out Muir Torre (Lynch) syndrome • Treatment‐ low dose isotretinoin, electrodesiccation, laser, shave removal, PDT, cryotherapy Nonmelanoma Skin Cancer (NMSC) • Actinic Keratosis • Basal Cell Carcinoma • Squamous Cell Carcinoma • Caused primarily by ultraviolet radiation • SCC and Actinic Keratoses – P53 tumor suppression gene mutated by UV • BCC – PTCH gene
Actinic Keratosis Actinic Keratosis • In-situ dysplasia from ultraviolet exposure. • Diagnosis ‐ Clinical • Sign of sufficient sun injury to develop NMSC. inspection • • Precancerous (low rate <1%) Red, scaly patch < 6mm. • • Prevented by sun screen use, even in adults. Tender to touch. • Sandpaper consistency. • Location ‐ Scalp, face, dorsal hands, lower legs (women) • When very thick, suspect hypertrophic AK or SCC
Actinic Keratoses and SCC Actinic Keratoses Actinic Keratoses- Treatment Actinic Keratoses‐ Treatment • Liquid nitrogen (single freeze‐thaw cycle) • Always biopsy if an AK is not responding • Topical treatment • 5‐fluorouracil (0.5‐5%) (Efudex) to appropriate therapy • 5% qd or BID for 2‐4 weeks • Imiquimod 5% cream (Aldara) – r/o SCC, superficial BCC • TIW x 4 weeks, with repeated cycles PRN • BIW or TIW x 16 weeks • QW x 24 weeks • Diclofenac (Solareze) • BID x 60‐90 days • Long term treatment (>120 days), moderately effective, side effects • Ingenol mebutate (Picato); 0.015%, 0.05% • Face/scalp‐ 0.015% QD x 3d • Trunk/extrem‐ 0.05% QD x 2d • Photodynamic therapy
Basal Cell Carcinoma Basal Cell Carcinoma‐ Clinical Subtypes • Most common of all cancers • Nodular (classic) – > 1,000,000 diagnosed annually in USA • Superficial – Lifetime risk for Caucasians: up to 50% • Pigmented • Intermittent intense sun exposure and • Morpheaform (scar‐like) overexposure (sunburns) • Locally aggressive, very rarely • Clinical subtypes have different biologic metastasize behavior • Histologic subtypes also influence behavior Basal Cell Carcinoma‐ Nodular
Basal Cell Carcinoma‐ Superficial Basal Cell Carcinoma‐ Pigmented • Clinically pink, slightly scaly, slightly shiny • May be entirely pigmented or there may patch be specks of pigment within what otherwise looks like a nodular or • Looks like an actinic keratosis superficial BCC • May be treated with imiquimod, ED+C • Melanoma is on the differential!! Basal Cell Carcinoma‐ Morpheaform • Clinically scar-like • Difficult to determine clinically where lesion begins and ends • Treat with excision (have pathologist check margins) or Mohs micrographic surgery – DO NOT ED+C
Basal Cell Carcinoma‐ Treatment Location, Size, and Subtype Guide Therapy • Superficial • Imiquimod • Electrodesiccation and curettage (ED+C) • Nodular or pigmented • ED+C • Excision (4mm margins) • Mohs micrographic surgery • Radiation‐ comorbidities, tumor size and location • Morpheaform, infiltrative, micronodular • Excision (4mm margins) • Mohs micrographic surgery J Am Acad Dermatol 2018;78:540-59 Topical Treatment of Skin Cancer Topical Treatment of Skin Cancer • Patient selection is the key • Scarring may be reduced compared to surgery • Work for superficial cancers (NOT invasive ones) • Superficial BCC ’ s and SCC in situ • Superficial BCC, SCC in situ • Long courses (months) may be required • Imiquimod 5% cream • – 5X per week for 6-10 weeks depending on the host Biopsy to confirm diagnosis before reaction treating – Efficacy 75%-85% • 5FU- – Topically twice daily for up to 12 weeks
Basal Cell Carcinoma‐ Treatment Squamous Cell Carcinoma Mohs micrographic surgery • Presents as red • Recurrent or incompletely excised tumors plaque, ulceration, or • Aggressive histologic subtype (infiltrative, wart like lesion morpheaform, micronodular) • Risk factors: • Poorly defined clinical margins – Fair skin • High risk location (face, ears, eyes) – Inability to tan – Chronic sun exposure • Large (>1.0 cm face, >2.0 cm trunk, extrem) • Special situations: • Tissue sparing location (face, hands, genitalia) – Organ transplant • Immunosuppressed patients recipients • Tumors in previously irradiated skin or scar • Tumors arising in setting of genetic diseases Keratoacanthoma • Rapidly growing (1month) • Dome-shaped nodule with central core of keratin • May spontaneously regress, but treat as an SCC
Squamous Cell Carcinoma Treatment • SCC in situ – 5-FU – Imiquimod – Liquid nitrogen – Electrodesiccation and curettage • Invasive SCC – Excision with 4-6 mm margins – Mohs micrographic surgery J Am Acad Dermatol 2018;78:560-78 J Am Acad Dermatol 2018;78:560-78 Squamous Cell Carcinoma‐ Treatment Skin Cancers on the Lower Legs Mohs micrographic surgery • • BCC and SCC in situ is common on the Recurrent or incompletely excised tumors • lower legs, especially in women Aggressive histologic subtype (perivascular, perineural) • Poorly defined clinical margins • Fixed, red, scaly patch(es) • High risk location (face, ears, eyes) – Mimic eczema • Large (>1.0 cm face, >2.0 cm trunk, extrem) • Think of skin cancer when red patches on • Tissue sparing location (face, hands, genitalia) the lower legs don ’ t clear with • Immunosuppressed patients moisturizing. • Tumors in previously irradiated skin or scar • Tumors arising in setting of genetic diseases
Case • 64M with psoriasis, hypertension, s/p renal transplant • Ulcer x 3 months of ulceration, thought to be due to venous insufficiency • 3 months of topical treatment fails to improve ulceration Skin Cancer in Organ Transplant Recipients • Skin Biopsy = Squamous • Skin cancer is most common malignancy in OTR Cell Carcinoma • Incidence increases with survival time post • Chronic phototherapy and transplant immunosuppressive • 90% are nonmelanoma skin cancer: SCC>BCC treatments have led to skin – Squamous cell carcinoma (SCC) cancer • 65 X the incidence in the general population • If leg ulcer doesn ’ t heal with – Basal cell carcinoma appropriate treatment—refer • 10 X the incidence in the general population or biopsy
Acquired Nevi (Moles) Skin Cancer in Organ Transplant Recipients • Biologic behavior much more aggressive than in the • Almost universal general population • Risk Factors • In areas of sun exposure – Older age • Change throughout life, appearing at preschool – Increased exposure to UV radiation age, growing during young adulthood, and – Increased immunosuppression involuting in old age – Fair skin • 5mm in diameter or less (size of pencil eraser) – Personal history of AK, NMSC, melanoma – Heart > kidney > liver transplants • Size (>6mm), number (more than 50) and pattern – HPV infection (not in sun exposed sites) predicts melanoma – Voriconazole • Refer OTR to a dermatologist for regular skin checks Atypical Moles • Not in sun exposed sites • Larger than 6 mm in diameter • Greater than 50
Recommend
More recommend