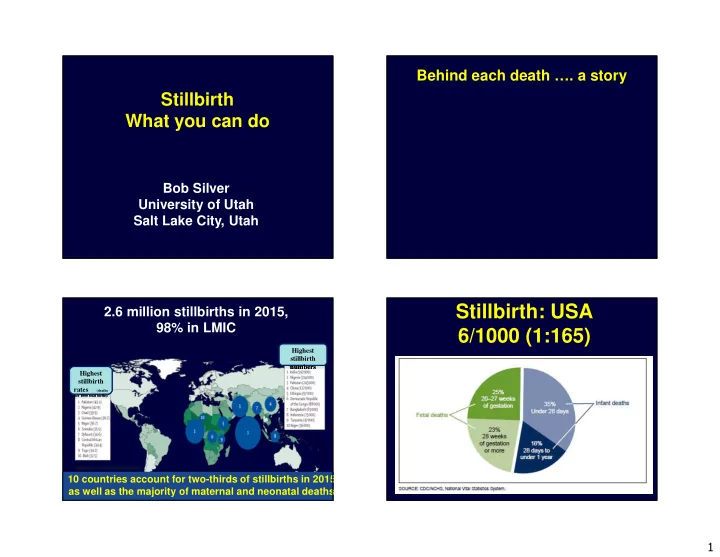
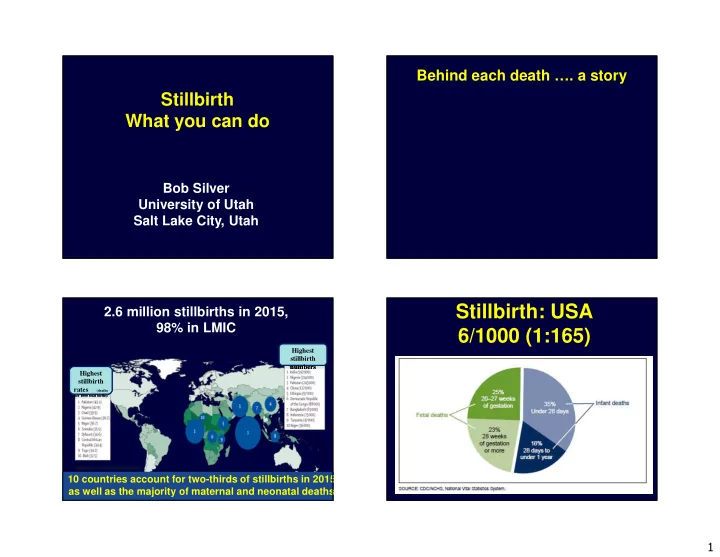
Behind each death …. a story Stillbirth What you can do Bob Silver University of Utah Salt Lake City, Utah Stillbirth: USA 2.6 million stillbirths in 2015, 98% in LMIC 6/1000 (1:165) Highest Highest stillbirth stillbirth numbers numbers Highest Highest stillbirth stillbirth rates (deaths rates (deaths per 1000 total births) per 1000 total births) 10 countries account for two-thirds of stillbirths in 2015 as well as the majority of maternal and neonatal deaths Source: Blencowe et al 2016 1
Stillbirth Stillbirth • Many stillbirths may be preventable De Bernis L, et al. Lancet. 2016. Woods, R. Bulletin of the WHO. 2008. Stillbirth rates and reductions Report card for stillbirths in United in high-income countries since 2000 States of America • ~ 46,200 stillbirths in 2015 WHO US national definition definition ~ 19,400 avoidable • ≥ 28 weeks ( ≥ 20 weeks) 2015 2013 stillbirths if stillbirth rate were ≤ 2/1000 in Stillbirth rate per 1000 births 3.0 6.0 all countries (Rank*) 25/186 • Large variation in Number of stillbirths per year 11,300 22,800 progress with 1.8% per year average Source: Flenady et al. Lancet 2016. Av annual rate of reduction 2000 0.4% YET Netherlands is progressing faster at – 2015 155/159 6.8% per year so faster progress is possible (Rank*) 2
Classification Systems 3
Stillbirth: Risk factors and Etiologies • Stillbirths are categorized by risk factors and by presumed etiology • Risk factors defined as maternal characteristics associated with stillbirth but without a known causal pathway leading to the death • Risk factors often present in live births Stillbirth Classification Systems Classification Systems • Over 80 systems • Numerous systems / Problems • No single “perfect” system • No gold standard to assess system • Best depends on goals • Cause of death hard to define • Wigglesworth • May be more than one cause • ReCoDe • May be multiple risk factors • TULIP • Granularity versus simplicity • What is the goal? • CODAC • Right tool for the job • INCODE Dudley et al. Obstet Gynecol 2010;116:254-60 4
Stillbirth Collaborative Research Stillbirths (Cases): Results Network (SCRN) • 663 stillbirths enrolled (03/06 – 08/08) • NICHD - RFA – 2001 workshop • 512 – complete postmortem exams • Population-based study � 425 (83%) antepartum stillbirth • 5 geographic catchment areas defined � 87 (17%) intrapartum stillbirth a priori by county lines • Race • 59 hospitals averaging >80,000 deliveries per year � White / Non-Hispanic: 35.7% � Black / Non-Hispanic: 22.5% • ≥ 90% of stillbirths (SBs) and live births (LBs) born to residents of the catchment � Hispanic: 34.4% areas are delivered in these 59 hospitals � Other: 7.2% SCRN; JAMA 2011;306:2459-68 INCODE INCODE Causes of Death Initial Causes of Fetal Death • Probable: high likelihood • Intended for research purposes • Possible: reasonable certainty - • Evidence based explicit definitions involved in a pathophysiologic • Evolving tool sequence • Each case reviewed by two MDs • Present: conditions of interest • Multidisciplinary panel for • May have ≥ 1 cause difficult cases Dudley et al. Obstet Gynecol 2010;116:254-60 Dudley et al. Obstet Gynecol 2010;116:254-60 5
INCODE INCODE Causes of Death: Diabetes Causes of Death: Broad Categories • Placental conditions • Probable: Macrosomia and poor • Obstetric complications control and / or embryopathy • Fetal / genetic abnormalities • Possible: Macrosomia or poor • Infections control only • Maternal medical conditions • Present: No macrosomia and • Umbilical cord abnormalities good control • Hypertensive disorders Dudley et al. Obstet Gynecol 2010;116:254-60 Genetic Conditions • The “ “ future ” ” of genetic testing “ “ ” ” Microarray Stillbirths: Cause of Death? for pregnancy loss (and everything else) • 61.1% - probable cause • 81.5% - possible or • Does not require live cells! probable cause • 40% - more than one possible • Identification of abnormalities not ascertained by conventional or probable cause cytogenetics SCRN; JAMA 2011;306:2459-68 6
Genetic Analysis Objective Karyotype - Microarray • Karyotype To determine if microarray – 5 – 10 megabase identifies abnormalities in – Losses and gains stillbirths not detected by • Microarray karyotype – Coverage at a higher density – 50 – 100 kilobase – Losses and gains (Copy number variants) Reddy et al, NEJM 2012;367:2185-2193 Results Results � Overall success rate � 157 Cases with failed karyotype – Karyotype: 70.5% – 74% normal array – Array: 87.4% (p<0.001) – 5.7% abnormal array � Abnormal (aneuploidy + pathogenic CNV) – Karyotype: 5.8% � Stillbirths with major anomalies (n=472) – 19.4% abnormal karyotype (13/67) – Abnormal Array: 8.3% (p=0.007) – 30% abnormal array (20/67) – 42% increased detection rate with array – 53.8% increased detection rate with array Reddy et al, NEJM 2012;367:2185-2193 Reddy et al, NEJM 2012;367:2185-2193 7
Case #1 Case #1 � 27 week stillbirth, 746 grams (AGA) � Multiple congenital malformations – Cranio-facial dysmorphism – Cleft soft palate – Limb deficiencies – Multiple cardiac defects Figure 3a: Case 1 Array Data 25 MB Deletion Panel A Panel B1 Region in q-arm, chro 4 of Loss Genes OMIM Loci SNPs CNPs Copy # x2 Chr. Band Copy Number State Panel B2 Region of Gain Panel C1 Genes Copy # x1 OMIM Loci SNPS 50 Genes CNPS Chr. Band Panel C2 Panel C3 7 OMIM loci 8
Array Data 2.5 MB Gain in p-arm, chro 17 Case #2 Copy # x3 � 37 week stillbirth, 2490 grams (AGA) Copy Number State � Multiple minor facial and lower extremity anomalies, no clear Copy # x2 recognized syndrome 20 Genes 6 OMIM loci Unbalanced translocation Array Data 2.5 MB Deletion Case #2 in q-arm, chro 22 Copy # x2 Copy Number State Copy # x1 30 Genes 12 OMIM loci Di George syndrome locus 9
Conclusions Conclusions • Array should be considered in cases • Primary benefit of array is the greater of karyotype failure or major likelihood obtaining a result anomalies – Ability to analyze non-viable tissue • Array may prove useful as a first line • Higher resolution allowing for screen for genetic abnormalities in detection of copy number changes stillbirth given higher yield of not visible on karyotype abnormalities as cost decreases Reddy et al, NEJM 2012;367:2185-2193 Reddy et al, NEJM 2012;367:2185-2193 Optimal Evaluation of stillbirth Optimal Evaluation of stillbirth • Multicenter prospective cohort • CONTROVERSIAL • Netherlands: 2002 – 2008 • Cost versus yield • 1025 stillbirths ≥ 20 weeks • Focus on common causes • Comprehensive evaluation • Focus on recurrent conditions • Cause of death (COD) determined • Panel determined if test in “ “ work- “ “ • Pay attention to clues • TULIP up ” ” helped to determine COD ” ” • Emotionally challanging: • Varied levels of comfort with autopsy or genetic testing Korteweg et al. Am J Obstet Gynecol 2012;206:e1-12 10
Clinical narrative Optimal Evaluation of stillbirth • Placental examination: Clinical suspicion for potential cause of death • Abnormal 89.2% (87.2 – 91.1) • Valuable 95.7% (94.2 – 96.8) Fetal autopsy • Autopsy: Placental pathology Maternal lab results • Abnormal 51.5% (47.4 – 55.2) Probable or Possible INCODE • Valuable 72.6% (69.2 – 75.9) classification Confirm or identify a Refute a suspected cause • Karyotype: cause • Abnormal 11.9% (8.7 – 15.7) Pertinent positive Pertinent negative • Valuable 29.0% (24.4 – 34.0) Korteweg et al. Am J Obstet Gynecol 2012;206:e1-12 Study Design Results � Pertinent positive � leads to a probable • 512 stillbirth cases or possible INCODE cause of death • 390 (76.2%) - probable or possible � Pertinent negative � rules out cause of death suspected causes based on clinical • 122 (23.8%) - without cause of death history – 105 present conditions only – 17 no INCODE conditions “Useful”: result that identifies a cause or identified confirms/refutes a clinical suspicion 11
Test Utility for Stillbirth Cause of Death Clinical Presentations 70% 60% • Growth Restriction 50% % Useful – 53 cases 40% • Hypertensive Disorders 30% 20% – 50 cases 10% • PTL/Chorio/PPROM 0% – 77 cases • Suspected Fetal Anomalies – 31 cases • No Clinical Clues – 115 cases Fetal Growth Restriction: Helpful Tests Hypertensive Disorders: Helpful Tests (n = 53) (n = 50) 100% 100% 90% 90% 80% 80% 70% 70% % Useful 60% 60% % Useful 50% 50% 40% 40% 30% 30% 20% 20% 10% 10% 0% 0% 12
Preterm Labor, Chorioamnionitis, Suspected Fetal Anomalies: Helpful PPROM: Helpful Tests (n = 77) Tests (n = 31) 90% 100% 80% 90% 80% 70% 70% 60% % Useful 60% % Useful 50% 50% 40% 40% 30% 30% 20% 20% 10% 10% 0% 0% No Clinical Clues: Helpful Tests (n = Autopsy 115) 90% 80% • Second most useful step in evaluation 70% 60% • Autopsy cause of death differed from % Useful 50% 40% the fetal death record in 55% of cases 30% • New information in 26-51% of cases 20% 10% • Birth defects and morphologic 0% abnormalities-genetic or developmental abnormalities • Confirm infection, anemia, hypoxia, and metabolic abnormalities 13
Recommend
More recommend