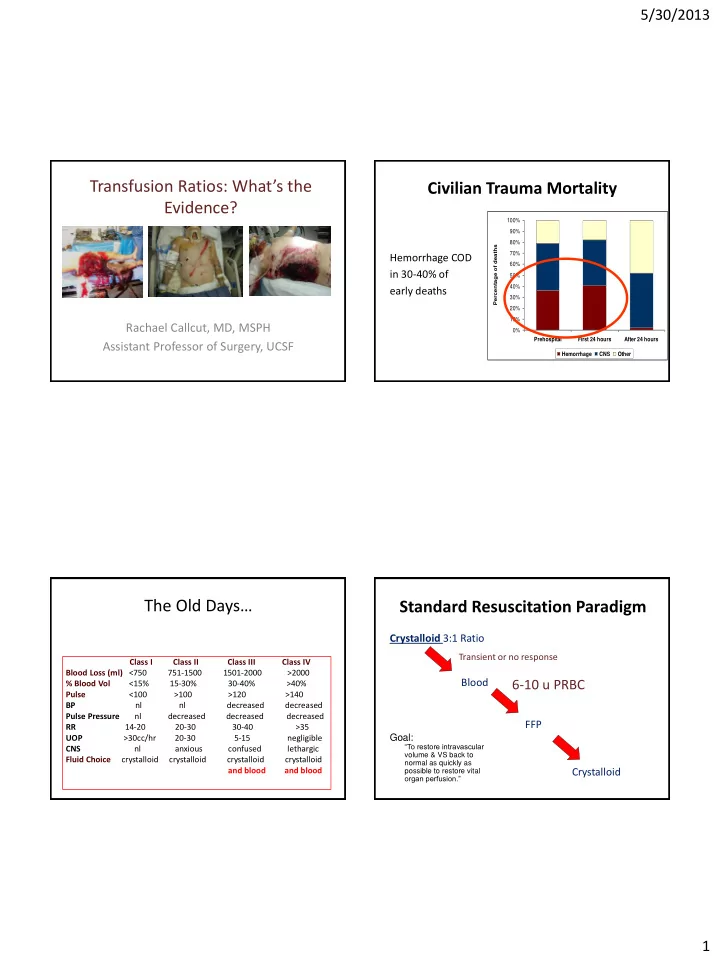
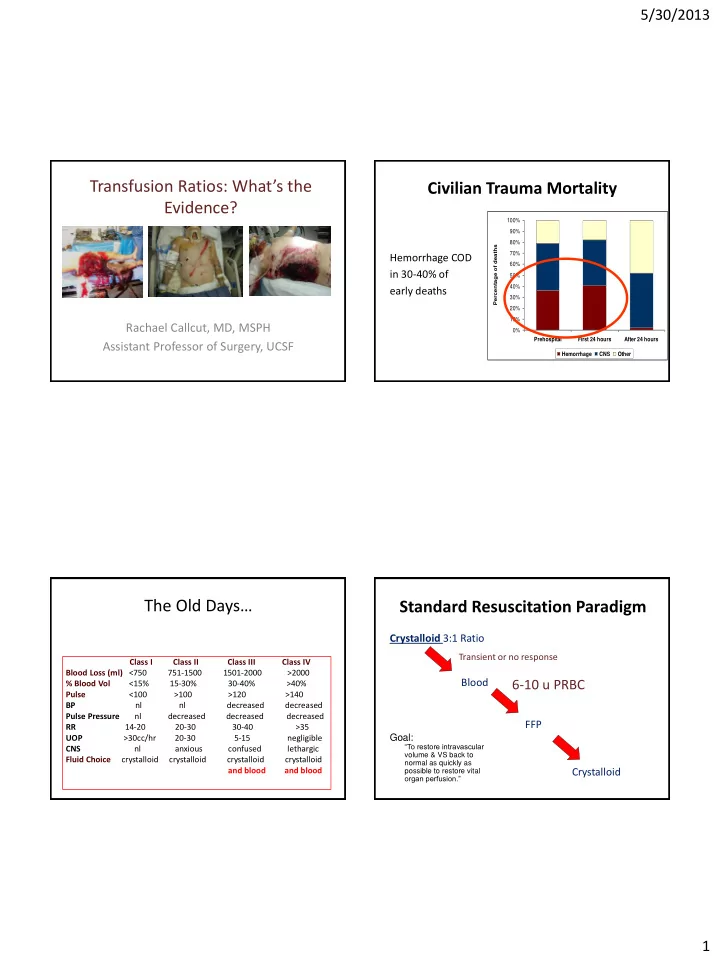
5/30/2013 Transfusion Ratios: What’s the Civilian Trauma Mortality Evidence? 100% 90% 80% Percentage of deaths 70% Hemorrhage COD 60% in 30-40% of 50% 40% early deaths 30% 20% 10% Rachael Callcut, MD, MSPH 0% Prehospital First 24 hours After 24 hours Assistant Professor of Surgery, UCSF Hemorrhage CNS Other Data adapted from: Acosta, et al. J Am Coll Surg 1998 & Sauaia, et al. J Trauma 1995 The Old Days… Standard Resuscitation Paradigm Crystalloid 3:1 Ratio Transient or no response Class I Class II Class III Class IV Blood Loss (ml) <750 751-1500 1501-2000 >2000 Blood 6-10 u PRBC % Blood Vol <15% 15-30% 30-40% >40% Pulse <100 >100 >120 >140 BP nl nl decreased decreased Pulse Pressure nl decreased decreased decreased FFP RR 14-20 20-30 30-40 >35 UOP >30cc/hr 20-30 5-15 negligible Goal: “To restore intravascular CNS nl anxious confused lethargic volume & VS back to Fluid Choice crystalloid crystalloid crystalloid crystalloid normal as quickly as and blood and blood possible to restore vital Crystalloid organ perfusion.” 1
5/30/2013 Military Resuscitation Standard Resuscitation • Cochrane Review (2003) • No evidence to support large-volume I.V. fluid resuscitation But is it harmful? The consequence… • Harmful effects: – Increased BP accelerates rate of bleeding which can dislodge a soft early clot – Dilutes RBCs therefore reduces oxygen delivery despite an increased CO – Reduced hct and clotting factors inhibit new clot formation – Resuscitative fluids are harmful themselves • Acidic • Pro-inflammatory • Abdominal Compartment Syndrome 2
5/30/2013 Lung Histology Lethal Triad Hypothermia Acidosis Death Sham WB Coagulopathy LR Brohi, K, et al. J Trauma, 2003. Makley et al, J Trauma 2010 Hypothermia Base Deficit • 18% arrive cold (<36°F) • 100% mortality <34°C 3
5/30/2013 What Resuscitation Strategy for the Severely Injured? What is the solution? What are our goals? Warm Fresh Whole Blood • Restore volume • Correct acidosis • Avoid coagulopathy • Avoid hypothermia • Blunt anemia Restore volume Reverse acidosis Avoid coagulopathy Avoid hypothermia Blunt anemia 4
5/30/2013 Component Therapy vs. Fresh Whole Blood How about reconstituted whole blood? Plt 5.5x10 10 50 mL PRBC FFP Hct 55% 80% 335 mL 275 mL 500 mL Warm Component Therapy Hct: 38-50% 1U PRBC + 1U PLT + 1U FFP + 10 pk Cryo = Plt: 150-400K 660 COLD mL Restore volume • Hct 29% Coags: 100% Reverse acidosis • Plt 87K Avoid coagulopathy 1500 mg • Coag activity 65% Avoid hypothermia • 750 mg fibrinogen Fibrinogen Blunt anemia • Armand & Hess, Transfusion Med. Rev., 2003 Hemostatic (Damage Control) Resuscitation Damage Control Resuscitation • Concept from Damage Control Surgery • Goal is to avoid exsanguination and – “Staying out of trouble rather than getting out of trouble” coagulopathy • Aggressive hemostatic resuscitation techniques should be performed in parallel with equally aggressive • Uses pRBCs and FFP + platelets surgical control of bleeding • Preliminary data from OIF/OEF • Civilian data compelling to make this Standard of Care J Trauma, 2007. 5
5/30/2013 Key Concepts of DCR • Recognize Shock • Resuscitate Immediately – Identify the critical 10 % – Devote attention to Hemostatic resuscitation • Provide volume that also How do we do it? restores the hemostatic cascade • Minimize crystalloid • Stop the bleeding Component Therapy • Stay out of trouble What Transfusion Ratio?? Can we apply this to the Civilian Trauma Patient? Cause of Death • Median ratio of FFP: RBC was 1:1.7 in survivors compared to 1:3 in non-survivors (p<0.001). 6
5/30/2013 Civilian Literature (2008) • Survivors vs. Non-Survivors – FFP:PRBC ratios • Plasma rich (≥1u FFP : 1.5u PRBCs) • Plasma poor (< 1u FFP : 1.5u PRBCs) • OR death (multivariate logistic regression) PRBC (mean +/- sd) 9.8 units +/- 11.7 1-80 units FFP (mean +/- sd) 8 units +/- 7.6 0-37 units FFP:PRBC (mean) 1 : 1.26 57% 1: 1.5 or better Plasma rich (survival) 84% 2746 pts needing operative intervention, Plasma poor (survival) 60% p=0.04 4yr retrospective study OR death (poor vs. rich) 3.57 (95% CI 1.02 – 12.5) p<0.05 Platelets: RBCs Multicenter, retrospective 466 pts. Single center, prospective, 214 MT pts. 7
5/30/2013 16 Trauma centers pooled their one year experience with transfusion of trauma patients 8
5/30/2013 Is all 1:1 the same? pRBC pRBC pRBC FFP pRBC pRBC pRBC pRBC FFP pRBC FFP pRBC FFP FFP FFP FFP FFP pRBC FFP FFP 5 pRBC, 5 FFP 5 pRBC, 5 FFP Prospective Observational Multicenter Major Trauma Transfusion study • 10 Level 1 trauma centers • July 2009-October 2010 • Primary objective: – Investigate in hospital mortality in all patients surviving at least 30 minutes after ED admission • Minute to minute tracking until resuscitation complete • Followed until hospital discharge 9
5/30/2013 Other Patient Population Who MAY Also Benefit? Known Theoretic • Trauma patients requiring • Massive GI bleed <10 units PRBCs (Sub MT) • Cardiac Surgery • Ruptured AAA • Major Orthopedic Cases • Emergency general surgery • Vascular elective surgery patients • OB PRBC 4 – 9 units PRBC 1 – 9 units 10
5/30/2013 Is 1:1 the correct ratio? 1400 MIP-2 800 MIP-1 α 1200 Concentration (pg/mL) Concentration (pg/mL) 600 1000 800 400 600 * 400 200 * 200 0 0 plasma 2:1 1:1 1:2 pRBCs plasma 2:1 1:1 1:2 pRBCs Figure 1:. MIP-2 Levels after resuscitation. P<0.05 vs all other groups Figure 2:. MIP-1 α Levels after resuscitation. P<0.05 vs plasma and pRBCs alone 20 14 Colon Evan’s Blue Lung Evan’s Blue Evans Blue (ug/g tissue) Evans Blue (ug/g tissue) 12 15 10 8 * * 10 6 4 5 2 Makley et al, http://cetir-tmc.org/research/proppr 0 0 manuscript plasma 2:1 1:1 1:2 pRBCs plasma 2:1 1:1 1:2 pRBCs 2011 Figure 4:. Evan’s blue levels in the colon after resuscitation. Figure 5:. Evan’s blue levels after resuscitation in the lung. P<0.05 vs plasma alone P<0.05 vs pRBCs alone Summary • Prospective Observational data supports prior retrospective data that more balance plasma • Phase III clinical trial to PRBC to platelets improves survival in • Investigating 1:1:1 plasma:platelet:pRBC vs. massively hemorrhaging trauma patients. 1:1:2 • RCT is forthcoming for optimum ratio. • 12 US trauma centers • Overall number of units utilized is decreasing. • Enroll 580 MT patients prospectively • Many analogous hemorrhaging ICU patient • Outcome 24 hr & 30 d mortality populations that may also benefit. 11
5/30/2013 Acknowledgements Acknowledgements • PROMMTT Investigators – Univ of Cincinnati Department of Surgery – Univ of Texas – Houston – UCSF • PROPPR Investigators • Cohen Research Staff • 24/7 Staff • Mary Nelson, RN • Military Colleagues 12
Recommend
More recommend