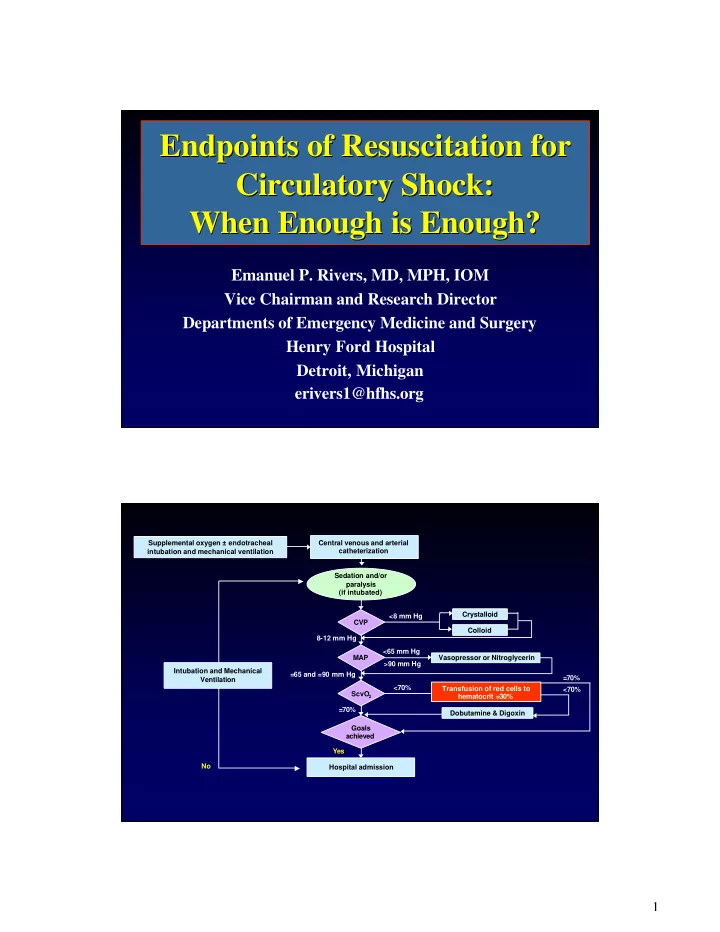
Endpoints of Resuscitation for Endpoints of Resuscitation for Circulatory Shock: Circulatory Shock: When Enough is Enough? When Enough is Enough? Emanuel P. Rivers, MD, MPH, IOM Vice Chairman and Research Director Departments of Emergency Medicine and Surgery Henry Ford Hospital Detroit, Michigan erivers1@hfhs.org Supplemental oxygen ± endotracheal Central venous and arterial catheterization intubation and mechanical ventilation Sedation and/or paralysis (if intubated) Crystalloid <8 mm Hg CVP Colloid 8-12 mm Hg <65 mm Hg MAP Vasopressor or Nitroglycerin >90 mm Hg Intubation and Mechanical =65 and =90 mm Hg =70% Ventilation <70% Transfusion of red cells to <70% ScvO hematocrit =30% 2 =70% Dobutamine & Digoxin Goals achieved Yes No Hospital admission 1
Communication Avoids Misunderstanding and Prevents Problems Inflammatory Mediators Produce Cardiovascular Insufficiency Increased Metabolic Demands: Hypovolemia,Vasodilation & Fever, Tachypnea Myocardial Depression Microvascular Alterations: Impaired Tissue Oxygen Utilization Cytopathic Tissue Hypoxia Fink, Crit Care Clin, 2002 2
The Purpose of Resuscitation “Perhaps Forgotten” Delivery Dependent Delivery Independent The Problem VO 2 • Uniformity of terminology Endpoints and Tools • Uniformity of goals Optimum region • Under-resuscitation e VO2 u s • Over-resuscitation s a i t i x l a o b p o y l • Multiple outcome G h measures in clinical trials • How do we solve the DO 2 Critical DO 2 problem? Substrates Goal Directed Optimization of Cardiac Function O 2 ATP DO 2 VO 2 - PaO 2 - Stress Glucose - Hemoglobin - Pain - Cardiac Output - Hyperthermia - Shivering Hemodynamic - Work of breathing - Preload (CVP, PCWP) - Afterload (MAP, SVR) Endpoints of Resuscitation - Contractility (SV) - Heart Rate (BPM) - Shock Index (HR/SBP) - Coronary Perfusion Pressure SvO Lactate 2 Microcirculation (a-v)CO 2 Happy Base Deficit Cell pHi Mediators DO 2 3
Macro Endpoints Delivery Dependent Delivery Independent Physical Exam VO 2 Heart Rate Blood Pressure Shock Index Urine Output Optimum region CVP/PCWP VO2 a i x o p y h e u s s i t l a b o l G Critical DO 2 DO 2 Substrates Goal Directed O 2 ATP Glucose Hemodynamic - Preload (CVP, PCWP) - Afterload (MAP, SVR) - Contractility (SV) - Heart Rate (BPM) - Shock Index (HR/SBP) - Coronary Perfusion Pressure 4
Effects of perfusion pressure on tissue perfusion in septic shock • OBJECTIVE: To measure the effects of increasing MAP on systemic O2 metabolism and regional tissue perfusion in septic shock. • DESIGN: Prospective study. • SETTING: MICU and SICU patients in a tertiary care teaching hospital. • PATIENTS: 10 patients with septic shock requiring pressor agents to maintain a MAP > 60 mm Hg after fluid resuscitation to a PAOP > 12 mm Hg. LeDoux, Crit Care Med, 2000 Effects of perfusion pressure on tissue perfusion in septic shock • INTERVENTIONS: Norepinephrine was titrated to MAPs of 65, 75, and 85 mm Hg in 10 patients with septic shock. 65 mmHg 85 mmHg Cardiac Index 4.7+/- 0.5 L/min/m2 5.5+/- 0.6 L/min/m2 (p < 0.03) Lactate 3.1+/-0.9 mEq/L 3.0+/- 0.9 mEq/L (NS) A-Gastric 13+/-3 mm Hg 16+/-3 at 85 mm Hg pCO2 (1.7+/-0.4 kPa) (2.1+/-0.4 kPa) (NS) Urine Output 49+/-18 mL/hr 43+/-13 mL/h (NS) LeDoux, Crit Care Med, 2000 5
Effects of perfusion pressure on tissue perfusion in septic shock CONCLUSIONS: – Increasing the MAP from 65 mm Hg to 85 mm Hg with norepinephrine does not significantly affect • systemic oxygen metabolism • skin microcirculatory blood flow • urine output • splanchnic perfusion. LeDoux, Crit Care Med, 2000 Radial artery pressure monitoring underestimates central arterial pressure during vasopressor therapy in critically ill surgical patients Critical Care Medicine 1998;26:1646-1649 Todd Dorman, MD, FCCM; Michael J. Breslow, MD, FCCM; Pamela A. Lipsett, MD; Jeffrey M. Rosenberg, MD, PhD; Jeffrey R. Balser, MD, PhD; Yaniv Almog, MD; Brian A. Rosenfeld, MD, FCCM • Radial artery pressure underestimates central pressure in hypotensive septic patients receiving high-dose vasopressor therapy. • The higher mean femoral arterial pressures: – immediate reduction in norepinephrine infusions in 11 of the 14 patients. • Clinical management, based on radial pressures, may lead to excessive vasopressor administration. 6
7
58% 60 54% Mortality (%) 37 % 40 20% 20 0 No No Vasopressor No Vasopressor Low Dose Vasopressor to Low Dose to High Dose to High Dose Vasopressor Vasopressor Vasopressor 15% % Receiving Vasopressors 60 50 40 30 20 10 0 0-6 hours 6-72 hours 0-72 hours No Corticosteroids 8
Substrates Goal Directed O 2 ATP DO 2 - PaO 2 Glucose - Hemoglobin - Cardiac Output Hemodynamic - Preload (CVP, PCWP) - Afterload (MAP, SVR) - Contractility (SV) - Heart Rate (BPM) - Shock Index (HR/SBP) - Coronary Perfusion Pressure An ICU Therapy Forever Changed • A restrictive strategy of red-cell transfusion is at least as effective as and possibly superior to a liberal transfusion strategy 9
Stop An International Crisis • Transfusions do make a difference in shock or global tissue hypoxia states. • Conservative management during the convalescent Abuse to the clinician phase. after giving blood Hemodilution After Volume 40 14 12 35 * * 10 * 30 Control 8 Control Treatment 25 6 Treatment 4 20 2 15 0 0-6 hours 6-72 hours 0-72 hours Baseline 3 hours 6 hours 7-72 hours 60 ml 3.6 Liters 447.13 More Fluid 500 450 339.49 400 350 No difference in blood 300 250 transfused over 72 hours 108 ml 200 150 between groups 100 50 0 0-72 hours 10
Hemodynamic Phases of Sepsis Transfusion Decisions Depend on the Clinical Sate Delivery Dependent Delivery Independent VO 2 VO 2 VO 2 SVO 2 VO 2 SVO 2 SVO 2 OER OER Lactate Lactate OER Lactate DO 2crit DO 2 • Even SvO 2 is a combination of various tissue beds. • The coronary circulation is at the highest risks. 11
Hemodynamic Phases of Sepsis Transfusion Decisions Depend on the Clinical Sate Delivery Dependent Delivery Independent VO 2 VO 2 VO 2 SVO 2 VO 2 SVO 2 SVO 2 OER OER Lactate Lactate OER Lactate DO 2crit DO 2 Transfusion Decisions Depend on the Clinical Sate Delivery Dependent Delivery Independent VO 2 VO 2 Dietrich, Critical Care, Med, 2000 VO 2 VO 2 Marik, JAMA, 2000 SVO 2 SVO 2 OER Herbert, NEJM, 2001 Lactate OER Vincent, JAMA, 2002 Lactate DO 2crit DO 2 12
Transfusion Studies EGDT, NEJM, Vincent, Hebert, NEJM, 1999 Marik, JAMA, 1993 2002 JAMA, 2002 Setting ED ICU ICU ICU Time (hours) <1 24 hours Over 2 weeks Up to 48 hours Age 62-67 57-58 53-59 49.6 Hemoglobin 11.3 – 11.4 8.2-8.2 10.1-12.2* 9.9 Lactate 6.9 - 7.7 1.8±1.8 -1.8±2.1 ---- 2.6 (mM/L) SvO 2 (%) 48.6 - 49.2 ---- ---- 69.5 CVP (mmHg) 5.3 - 6.1 ---- ---- Resuscitated Cardiac Index 1.7 – 1.9 ---- ---- 3.4 Transfusion Studies EGDT, NEJM, Vincent, Hebert, NEJM, 1999 Marik, JAMA, 1993 2002 JAMA, 2002 20.4±7.4 - 16.5-13.5 ---- APACHE 20.9±7.3- 21.3±8.1 21.4±6.9 18.5-10% ICU Mortality 56-30.5% 22.2 vs. 28.1% (0.05) 22 -17% 28 day Decreased pHi And Endpoints Excluding dialysis patients, patients likely to die in 24 In shock or hours and patients in 100% 16-13% global tissue 20-23% established septic shock hypoxia? (systolic blood pressure <90 mmHg). 13
Substrates Goal Directed O 2 ATP DO 2 VO 2 - PaO 2 - Stress Glucose - Hemoglobin - Pain - Cardiac Output - Hyperthermia - Shivering Hemodynamic - Work of breathing - Preload (CVP, PCWP) - Afterload (MAP, SVR) - Contractility (SV) - Heart Rate (BPM) - Shock Index (HR/SBP) - Coronary Perfusion Pressure SvO2 = 65 - 75% 20 volume % 5 liters/min. 25% 1000 ml/min 250 ml/min 14
ScvO 2 SvO 2 70-75% - + VO 2 DO 2 Stress PaO2 • • • Pain • Hgb • Hyperthermia • Cardiac Output Shivering • • Work of breathing Using Metabolic Endpoints SvO 2 15
Lactate and Outcome (Mizock, Dis Mon, 1989) (Weil, Circulation, 1970) Survivors Non-survivors 6 5 Lactate (mM/L) 4 3 2 N = 76 1 0 0 8 16 24 36 48 Time (hrs) Clearance Survivors Nonsurvivors % Survival < 24 hrs 27 0 100 24-48 hrs 21 6 77.8 > 48 hrs 3 19 13.6 (Abramson and Scalea, J Trauma, 1993) 16
Crit Care Med 2004 Vol. 32, No. 8 ∆ Lactate (ED Admission - ED Discharge) N = 114 14 ED Length of Stay (hrs) 16 12 No clearance 10 • 14 8 84 < 0 mM/L/hr Lactate • (mM/ L) 6 Intermediate clearance • 4 0-1 mM/L/hr • 2 High clearance 0 • No Clearance High > 1 mM/L/hr • Clearance ED Admission ED Discharge Crit Care Med 2004 Vol. 32, No. 8 ∆ Lactate (ED Admission - ED Discharge) ED Length of Stay (hrs) 80 70 60 50 N = 243 40 Lactate 30 Clearance 20 % 10 0 -10 -20 -30 1 2 3 4 Quartiles of Lactate Clearance 17
50 50 45 40 Mortality (%) Early Lactate Clearance 35 30 23 25 20 12 15 10 5 11 No Clearance 0 Intermediate Clearance 10 No Clearance Intermediate High High Clearance Clearance Clearance 9 MODS 8 7 6 5 4 3 0 6 12 24 36 48 60 72 Time (hr) p<0.05 % Lactate Clearance Quartiles and mean Biomarker Levels over 72 Hours 10 9 8 Caspase-3 (ng/mL) 7 6 5 4 3 2 1 0 1 2 3 4 Lactate Clearance Quartiles 18
Recommend
More recommend