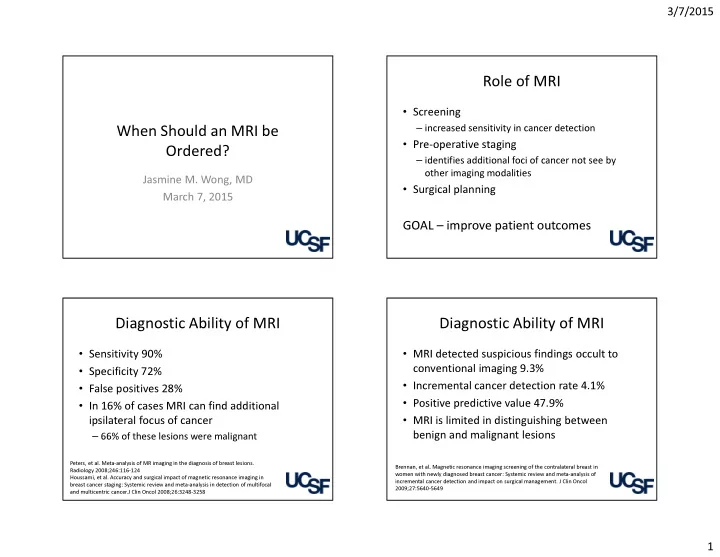
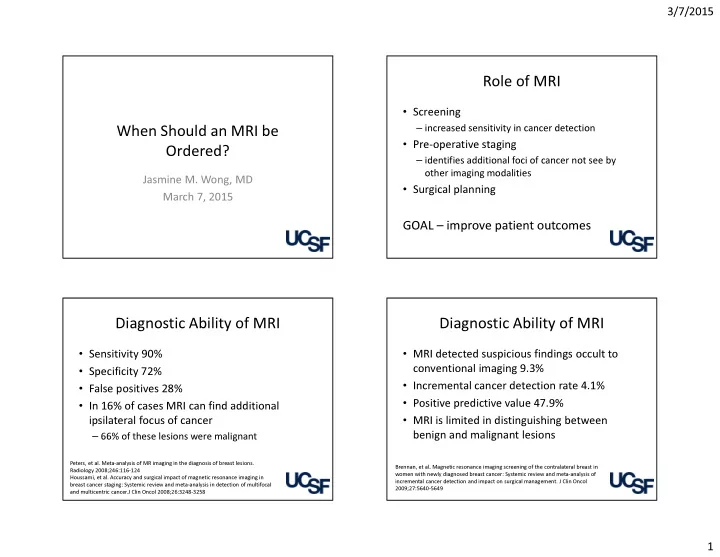
3/7/2015 Role of MRI • Screening – increased sensitivity in cancer detection When Should an MRI be • Pre-operative staging Ordered? – identifies additional foci of cancer not see by other imaging modalities Jasmine M. Wong, MD • Surgical planning March 7, 2015 GOAL – improve patient outcomes Diagnostic Ability of MRI Diagnostic Ability of MRI • Sensitivity 90% • MRI detected suspicious findings occult to • Specificity 72% conventional imaging 9.3% • Incremental cancer detection rate 4.1% • False positives 28% • Positive predictive value 47.9% • In 16% of cases MRI can find additional • MRI is limited in distinguishing between ipsilateral focus of cancer – 66% of these lesions were malignant benign and malignant lesions Peters, et al. Meta-analysis of MR imaging in the diagnosis of breast lesions. Brennan, et al . Magnetic resonance imaging screening of the contralateral breast in Radiology 2008;246:116-124 women with newly diagnosed breast cancer: Systemic review and meta-analysis of Houssami, et al. Accuracy and surgical impact of magnetic resonance imaging in incremental cancer detection and impact on surgical management. J Clin Oncol breast cancer staging: Systemic review and meta-analysis in detection of multifocal 2009;27:5640-5649 and multicentric cancer.J Clin Oncol 2008;26:3248-3258 1
3/7/2015 MRI and Surgical Outcomes MRI and Surgical Outcomes • Monet trial - randomized control trial in patients • COMICE trial - addition of MRI to triple with non-palpable suspicious breast lesions assessment (clinical exam, mammography, detected on mammogram or ultrasound • Primary breast conserving surgery was similar in ultrasound) was not significantly associated with a reduced re-operation rate both groups • Number of conversions to mastectomy did not – Both groups had 19% of their patients needing differ significantly reoperation • Number of re-excisions for positive margins higher in the MRI group Peters, et al. Preoperative MRI and surgical management in patients with Turnbull, et al . Comparative effectiveness of MRI in breast cancer (COMICE) trial: nonpalpable breast cancer: The MONET – Randomised controlled trial Eur J Cancer randomised controlled trial. Lancet 2010;375:563-571 2011;47:879-886 Take Away Points Current Clinical Indications • MRI has high sensitivity, but low specificity • High risk patients • MRI only incrementally increases cancer • Invasive lobular carcinoma • Neoadjuvant chemotherapy detection rates both in the ipsilateral and contralateral breast • Occult primary • MRI in the pre-operative setting does not affect short term surgical outcomes • MRI should not be used for routine screening or routine pre-operative staging 2
3/7/2015 High Risk Patients High Risk Patients • Women who are BRCA 1 or BRCA 2 gene • MRI has higher sensitivity than mammography mutation carriers for detecting breast cancer – MRI not affected by breast density • Untested first degree relatives of BRCA gene • MRI has the ability to detect smaller tumors mutation carriers • Women with greater than 20-25% lifetime risk than mammography • No data on outcome or survival of developing breast cancer based on family history Saslow, et al. American Cancer Society guidelines for breast screening with Kriege, et al. Efficacy of MRI and mammography for breast cancer screening in MRI as an adjunct to Mammography. CA Cancer J Clin 2007;57:75-89 women with familial or genetic predisposition. N Engl J Med2004;351:427-437 American Cancer Society Guidelines High Risk Patients • Women with a history of chest radiation before age 30 • Women with TP53 and PTEN gene mutations Sensitivity of MRI in high risk patients ranges from 77- 100% compared with mammography which ranges Saslow, et al. American Cancer Society guidelines for bresat screening with MRI from 16 to 40% as an adjunct to Mammography. CA Cancer J Clin 2007;57:75-89 3
3/7/2015 High Risk Patients American Cancer Society Guidelines • Insufficient evidence to recommend or • No consensus on when to start screening in discourage MRI screening of women with 15- high risk patients 20% lifetime risk of breast cancer or women – 5 years younger than the first relative who with LCIS, ALH, ADH, dense breasts, or a presented with breast cancer personal history of cancer – Starting at age 30 • No consensus on when to stop MRI screening High Risk Patients Current Clinical Indications • Mutation carriers (>50%) • High risk patients – Cancer detection rate of 26.5 per 1000 patients • Invasive lobular carcinoma • High risk (30-49%) • Neoadjuvant chemotherapy – Cancer detection rate of 5.4 per 1000 patients • Occult primary • Moderate risk (15-29%) – Cancer detection rate of 7.8 per 1000 patients Kriege, et al. Efficacy of MRI and mammography for breast cancer screening in women with familial or genetic predisposition. N Engl J Med 2004;351:427-437 4
3/7/2015 Invasive Lobular Carcinoma Invasive lobular carcinoma • MRI found to more accurately determine • 2 nd most common breast cancer, but only 5- tumor size compared to mammography 15% of all breast cancers • Mammography underestimated the tumor • More likely to be multi-centric, multi-focal size significantly more frequently than MRI and/or bilateral compared to other types • Overestimation of the tumor size happened • Often more difficult to detect with equal frequency • Can be difficult to determine extent of disease – Usually due to extensive LCIS around the tumor Mann, et al. The value of MRI compared to mammography in the assessment of tumor extent in invasive lobular carcinoma of the breast. Eur J Surg Oncol 2008; 34:135-142 Scatter plots of tumor size Invasive Lobular Carcinoma • Significantly fewer patients in the MRI group had a re-excision – Odds ratio for re-excision – 3.29 • No significant difference in initial mastectomy rates Mann, et al. The value of MRI compared to mammography in the assessment of Mann, et al. The impact of preoperative breast MRI on the re-excision rate in tumor extent in invasive lobular carcinoma of the breast. Eur J Surg Oncol 2008; invasive lobular carcinoma of the breast. Breast Cancer Res Treat 2010; 119:415- 34:135-142 422 5
3/7/2015 Current Clinical Indications Neoadjuvant chemotherapy • Invasive lobular carcinoma • Increased use of neoadjuvant chemotherapy • High risk patients has led to the need for a tool to assess tumor response to treatment • Neoadjuvant chemotherapy • MRI offers a non invasive way to assess • Occult primary tumors before, during, and after neoadjuvant treatment to help determine the appropriate surgical therapy for patients MRI Phenotypes 1—well defined, uni-centric mass 2—well defined, multi-lobulated mass 3—area enhancement with nodularity 4—area enhancement without nodularity 5—septal spreading. 6
3/7/2015 Neoadjuvant Chemotherapy Neoadjuvant Chemotherapy • Assessment of tumor volume with MRI has • MRI is more accurate than clinical exam, mammography, and ultrasound for determining been shown to be a strong predictor of residual tumor size pathologic response to neoadjuvant • MRI can predict clinically meaningful tumor reduction chemotherapy – Well defined MRI phenotypes have higher rates of tumor • Multiple studies have shown that the ability of reduction than diffuse MRI phenotypes – Her2 positive and triple negative tumor have higher rates MRI to predict pathologic complete response of tumor reduction than hormone receptor positive and Her2 negative tumors is related to tumor subtypes Lobbes, et al. The role of magnetic resonance imaging in assessing residual disease and pathologic complete response in breast cancer patients receiving neoadjuvant chemotherapy: a systemic review. Insights Imaging 2013;4:163-175 Hylton, et al. Locally Advanced Breast Cancer: MR Imaging for Prediction of Response Mukhtar, et al. Clinically Meaningful Tumor Reduction Rates Vary by Prechemotherapy MRI in Neoadjuvant Chemotherapy – Results from ACRIN 6657/I-SPY TRIAL Radiology phenotype and Tumor Subtype in the I-SPY 1 TRIAL (CALGB 150007/150012; ACRIN 6657) 2012;263:663-672 Ann Surg Oncol 2013;20:3823-3830 Current Clinical Indications Study N Findings • High risk patients Hayashi et al. 2013 260 • Sensitivity/Specificity highest in TN tumors • PPV decreased in order TN, ER-/Her2+, ER+/Her2+,ER+/Her2- • Invasive lobular carcinoma Ko et al. 2013 166 • Size prediction less accurate in ER+ tumors • Neoadjuvant chemotherapy Cruz et al. 2013 205 • Better correlation between MRI measured response and pathologic response in TN and Her2+ tumors • Occult primary Loo et al. 2011 188 • MRI size change associated with path residual disease for TN and Her2+ tumors; not for ER+/Her2- Kuzucan et al. 2012 54 • Among Her2- tumors, MRI accuracy higher in high-proliferation (high Ki-67) tumors McGuire et al. 2011 203 • MRI accuracy for predicting pCR lowest in luminal tumors; highest in TN and ER-/Her2+ tumors Greater MRI-pathology agreement and more accurate prediction of pathologic complete response in triple negative and Her2+ hormone receptor negative breast cancers 7
Recommend
More recommend