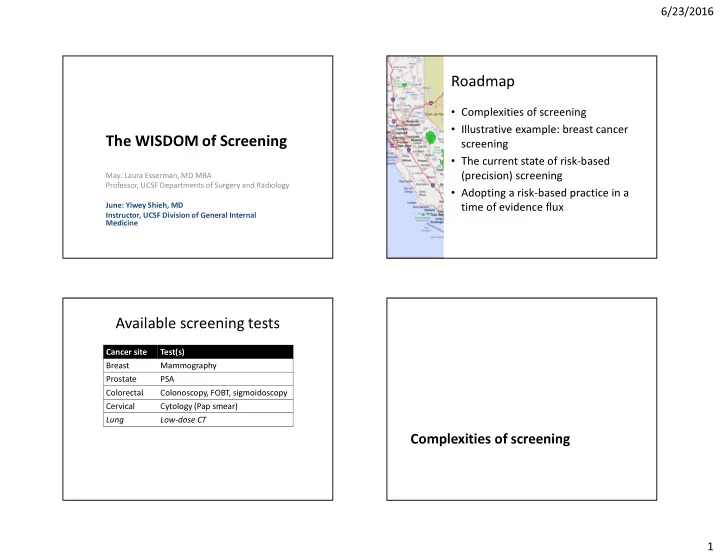
6/23/2016 Roadmap • Complexities of screening • Illustrative example: breast cancer The WISDOM of Screening screening • The current state of risk-based May: Laura Esserman, MD MBA (precision) screening Professor, UCSF Departments of Surgery and Radiology • Adopting a risk-based practice in a June: Yiwey Shieh, MD time of evidence flux Instructor, UCSF Division of General Internal Medicine Available screening tests Cancer site Test(s) Breast Mammography Prostate PSA Colorectal Colonoscopy, FOBT, sigmoidoscopy Cervical Cytology (Pap smear) Lung Low-dose CT Complexities of screening 1
6/23/2016 New Paradigm: variable progression Old Paradigm: inexorable progression INDOLENT SLOW RAPID Normal LESIONS PROGRESSION PROGRESSION “cancer” is one disease . . . Cell Normal Normal Normal Cell Cell Cell Atypical Cell Atypical Atypical Stage 1-3 Cell/CIS Cell/CIS Cancer Carcinoma In Situ Stage 1 Stage 1 Detectable Cancer Cancer Metastasis Stage 1 Cancer Stage 2-3 Cancer death Cancer IDLE condition : Stage 2-3 Detectable Indolent lesions Cancer of epithelial origin Metastasis Indolent Tumors: Detectable Cancer Rare metastases, Metastases death course Indolent Cancer Early Detection Will Early Detection Will Early Detection Systemic Therapy Key death Reduce Mortality Esserman Lancet Onc 2014 Not Impact Mortality Reduce Mortality to Reducing Mortality The good: incidence has declined The good: mortality has declined (for some cancer sites) U.S. Women, 1975-2013 U.S. Men, 1975-2013 U.S. Men, 1975-2013 U.S. Women, 1975-2013 Colorectal cancer Colorectal cancer Colorectal cancer Colorectal cancer Cervical cancer Cervical cancer Prostate cancer Breast cancer seer.cancer.gov seer.cancer.gov 2
6/23/2016 New Paradigm: variable progression Evidence for benefit in cervical and INDOLENT SLOW RAPID colorectal cancer screening LESIONS PROGRESSION PROGRESSION Normal Normal Normal • Cervical cancer Cell Cell Cell – Incidence rate decline in multiple cohort studies Atypical Atypical Stage 1-3 – RCTs in India showing mortality benefit of both HPV Cell/CIS Cell/CIS Cancer testing and visual acetic acid exam Stage 1 Stage 1 Detectable – Most new cases occur in unscreened women Cancer Cancer Metastasis • Colorectal cancer Cancer Stage 2-3 – RCTs and cohort studies on sigmoidoscopy death Cancer • Drop in incidence rate 18-23% IDLE condition : • Drop in mortality 22-31% Detectable Indolent lesions – Modeling: 50% of decline in incidence/mortality of epithelial origin Metastasis Indolent Tumors: Cancer attributable to screening Rare metastases, death course Indolent Early Detection Will Early Detection Systemic Therapy Key Not Impact Mortality Reduce Mortality to Reducing Mortality The bad: incidence has increased Early stage cancers driving increase in incidence rates (for certain cancers) U.S. Men, 1975-2013 U.S. Women, 1975-2013 Breast Prostate Colorectal cancer Colorectal cancer Cervical cancer Prostate cancer Breast cancer seer.cancer.gov Esserman JAMA 2009 3
6/23/2016 Overdiagnosis occurs when screening An example of overdiagnosis: picks up IDLE or indolent disease Thyroid cancer screening in Korea INDOLENT IDLE Ahn NEJM 2014 Screening does not always prevent metastatic A thought experiment… disease at time of first presentation Breast 50 % of overall cancers detected 40 30 20 10 0 Fast Slow Very Slow IDLE Prostate Colorectal & Cervical 50 50 % of overall cancers detected % of overall cancers detected 40 40 30 30 20 20 10 10 0 0 Fast Slow Very Slow IDLE Fast Slow Very Slow IDLE Welch NEJM 2015 4
6/23/2016 What makes screening so complex? • Benefits of screening are proportionate to distribution of biologic tumor types • Distribution of tumor types is changed by screening • Perceptions of screening benefit are also proportionate to distribution of biologic The case for “IDLE” or indolent tumor types • Impact of screening changes with advances in tumors in breast cancer treatment Defining indolent breast cancers using Ultra Low risk: Threshold determination and locking gene expression profiling Ultra Low Threshold determined using NEJM publication with 25 years FU 70 significant prognosis genes data (van de Vijver et al, NEJM 2002; Drukker et al, BCRT 2014) • Node negative at time of diagnosis • 100% overall survival at 25 years Ultralow • Ultra low risk threshold locked at MP-score 0.7 Threshold Ultra low group (yellow curve): Ultra low group (yellow curve): • • Threshold at 0.7 Threshold at 0.7 • • 100% overall survival @ 25 years (n=8) 100% overall survival @ 25 years (n=8) Vant Veer Nature 2002 Threshold different and refined from Esserman et al BCRT: Nature paper 5 yrs FU 5
6/23/2016 Indolence = excellent survival Evidence for indolent prostate cancers regardless of treatment Prostate cancer mortality in low risk (Gleason ≤ 6, PSA ≤ 10) lesions followed with active surveillance 94% Survival NO Systemic Tx 20 years 97% Survival 20 years Klotz JCO 2014 30% of Screen Detected Are Categorized as 70-gene prognosis signature index score distribution “Ultralow Risk” Cancers Women aged 49-60 Women aged 49-60 High Unscreened, symptomatic Screened, asymptomatic Esserman, Shieh, vant Veer BCRT 2011 Esserman, Shieh, vant Veer BCRT 2011 6
6/23/2016 DCIS Increased 500% after the Advent of Consequences: Treatment of DCIS Mammographic Screening . . . Figure 2. SEER9 Age-adjusted incidence rate of breast cancer by stage (1973-2005) 100 90 80 Incidence rate (per 100,000) 70 Localized 60 In situ Rate Localized Rate 50 Regional Rate Distant Rate 40 Regional 30 20 In Situ 10 0 Metastatic 1975 1980 1985 1990 1995 2000 2005 Year of diagnosis Wells J Am Coll Radiol 2013 Li CEBP 2005 Questionable benefit of radiation or For low-grade DCIS, no benefit to mastectomy in DCIS surgery • Observation of >100,000 women with DCIS • 20-year breast cancer • 57,222 women (SEER) mortality = 3.3% • 2% (1169) of women • Mortality rates equivalent had observation only among women treated with lumpectomy, • Survival in low grade lumpectomy + radiation, DCIS IDENTICAL (98.6 vs and mastectomy • >50% of women who died 98.8%) for surgery vs. of breast cancer did not not have in-breast recurrence Narod JAMA Oncology 2015 7
6/23/2016 Precursor of Indolent tumor fits Recap definition of IDLE DCIS Dx • Screening will uncover indolent tumors, or precursors to indolent tumors. • We must be prepared to deal with them. IDLE Condition Unintended Consequences of the Screening Controversy Some women screened too much, others too little Women are caught in the middle... and some are choosing not to screen at all PATIENTS ASSUME THAT CANCER, LEFT UNTREATED , WILL KILL YOU Physicians too 31 8
6/23/2016 Mammography guidelines, 2016 Mammography guidelines, 2016 USA Rest of world Start screening at Terminate Frequency of Start screening at Terminate Frequency of Country Organization age screening at age assessment age screening at age assessment Every 2 years (for Canada 50 74 Every 2-3 years United States Preventive women at average- Services Task Force 50 74 risk of breast (USPSTF) 50 70 cancer) United Kingdom Every 3 years (47) (73) Annually then As appropriate American Cancer Society biennially at 55 The Netherlands 50 75 Every 2 years 45 based on life (ACS) years of age and expectancy older Australia 50 74 Every 2 years American College of As appropriate Obstetricians and 40 based on life Annually Gynecologists (ACOG) expectancy Switzerland recently considering ending mammography screening altogether because of lack of evidence that the benefits outweighs the harms. American College of As appropriate Biller-Andorno and Jüni, NEJM, 2014. Radiology (ACR)/Society 40 based on life Annually of Breast Imaging (SBI) expectancy A proposed approach RISK-BASED SCREENING Shieh Nature Rev Clin Onc 2016 9
6/23/2016 Screening cascade, part 1 Screening cascade, part 2 Shieh Nature Rev Clin Onc 2016 Shieh Nature Rev Clin Onc 2016 Choosing whom to screen Deciding how often to test • Lung cancer screening • HPV-negative after age – Age > 55 years 30 � retest in 5 years – 30+ pack-year history of • Colonic polyps smoking – Few small, hyperplastic – If former smoker, quit polyps � 10 years within 15 years – Tubular adenomas � 5- • BRCA mutation carriers 10 years (depending on in breast cancer size, number) – Mammogram + MRI – Sessile serrated polyps every 6 months (ACS � 3-5 years guidelines) 10
Recommend
More recommend