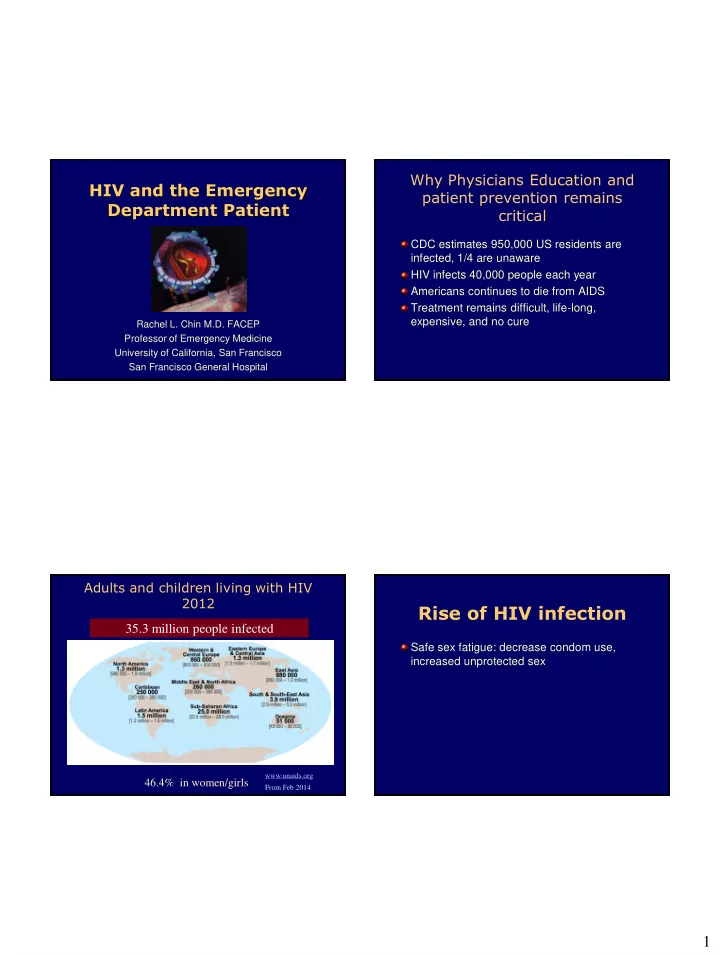
Why Physicians Education and HIV and the Emergency patient prevention remains Department Patient critical CDC estimates 950,000 US residents are infected, 1/4 are unaware HIV infects 40,000 people each year Americans continues to die from AIDS Treatment remains difficult, life-long, expensive, and no cure Rachel L. Chin M.D. FACEP Professor of Emergency Medicine University of California, San Francisco San Francisco General Hospital Adults and children living with HIV 2012 Rise of HIV infection 35.3 million people infected Safe sex fatigue: decrease condom use, increased unprotected sex www.unaids.org 46.4% in women/girls From Feb 2014 1
Rise of HIV infection Safe sex fatigue: decrease condom use, increased unprotected sex Medications (HAART/ART) 2
3
Rise of HIV infection Safe sex fatigue: decrease condom use, increased unprotected sex Medications (HAART/ART) Increased access to sex: internet, circuit parties, public sex venues Increased recreational drug use, esp crystal methamphetamines and ecstasy 4
Rise of HIV infection Safe sex fatigue: decrease condom use, increased unprotected sex Medications (HAART) Increased access to sex:internet, circuit parties, public sex venues Increased recreational drug use, esp crystal methamphetamines and ecstasy Viagra Viagra + Ecstasy = Sextasy 5
Case #1 Objectives Learn how to recognize subtle complaints in the most 28 year old HIV positive man complains of dry common life-threatening AIDS infections. cough for 2-4 weeks and fevers. He has no history of Opportunistic Infection (OI ’ s) and Identify what tests may be helpful in the diagnosis of the most common OI in the US. takes no medicines. Normal Vital signs. O 2 saturation 95%. CXR clear. Summarize the treatment and management of these OI ’ s. Learn about the adverse effects of HIV-Therapy Become aware of drug induced metabolic changes What is the Stage of HIV infection? Returns 10 days later with diffuse pneumonia Defined by CD4 count: and goes to the ICU with the diagnosis of • Early: CD4 > 500/mm 3 PCP. • Intermediate: CD4 200-500/mm 3 What could have changed this management? • Late: CD4 < 200/mm 3 What was the stage of the HIV infection? • ?Very Late: CD4 < 50/mm 3 6
Viral Load Monitors therapy Always need CD4 count in your decision making It is essential in suggesting the medications < 200 and no PCP prophylaxis, all URI ’ s are not working either to • non-adherence need close follow up • drug interactions > 200 or on prophylaxis (and compliant), then • malabsorption bronchitis • mutations Pulmonary disease is one of the most common HIV-related emergencies PCP is the leading AIDS-defining condition in the United States Absolute lymphocyte count (ALC) Pneumocystis jiroveci ( “ yee row vet zee ” - • < 950 x 10 6 cells/μL ~ CD4 < 200 x 10 6 cells/μL formerly carinii) pneumonia Pretest probability CDC. HIV/ AIDS Surveillance Reports Academic Emergency Med 2011;18:385-389 Emerging Infectious Diseases 2002;8(9):891-896 7
P neumo c ystis jiroveci PCP Chest Radiographic P neumonia Presentation Bilateral > Unilateral, Symmetric > Asymmetric Clinical presentation • CD4 cell count ≤ 200 cells/mm 3 Pattern • Interstitial (reticular) or granular • Symptoms: fever, DOE, dry cough , fatigue • Alveolar (consolidation) • Duration: >2-4 weeks • Cyst(s) • Signs: Nonspecific • Normal • Labs: Serum LDH often elevated • Pneumothorax PCP Chest Radiographic Treatment Presentation Trimethoprim-sulfamethoxazole Clindamycin + Primaquine Trimethoprim + Dapsone Atovaquone Pentamidine Treat for 21 days followed by prophylaxis • Steroids 40 mg PO BID if Pa02 < 70 mm Hg 8
Bacterial Pneumonia Case #2 Clinical presentation 28 year old HIV + man complains of • CD4 cell count: any headache. No medications. • Symptoms: Fever, SOB, chest pain, productive What do you need to know? cough w/ purulent sputum Is his HIV infection early, intermediate, or • Duration: 3-5 days late? • Signs: Focal lung findings CD4 < 100, need LP to rule out cryptococcal • Labs: WBC often (relatively) elevated meningitis Cryptococcal meningitis CNS Emergencies Clinical presentation Cryptococcal meningitis • Signs: ± meningeal Cryptococcal signs neoformans is the most • Dx: common fungus • CT/MRI usually responsible for infections negative in patients with AIDS. • CSF CrAg + > 90-95% Clinical presentation Treatment • CD4 < 100 cells/mm 3 • Ampho B +/- Flucytosine • Symptoms: fever, for 2 wks • Oral fluconazole for headaches • Duration: weeks to chronic suppressive therapy months • Manage increased ICP, hydrocephalus, seizures 9
Cerebral Toxoplasmosis CNS Emergencies Diagnosis Cerebral Toxoplasmosis • CT/MRI: multiple ring- enhancing lesions Toxoplasma gondii, a parasite, is the most • Inferred by response common cause of focal brain lesions in to empiric therapy people with AIDS Treatment Clinical presentation • Pyrimethamine, • CD4 < 200 cells/mm 3 sulfadiazine, folinic • Symptoms: headache, fever, AMS, focal signs acid over days to weeks • Expect clinical and • Signs: seizures (25%-50%), focal signs over days radiologic to weeks improvement in 2 • Labs: Toxo titers usually positive weeks Prophylaxis and Treatment of HAART/ART OI ’ s- What ’ s New? Cessation of primary prophylaxis for PCP Highly active antiretroviral therapy/ • Short-term data CD4 > 200 for 3-6 months, no PCP antiretroviral therapy Cessation of prophylaxis for disseminated MAC Combination of at least 3 drugs • CD4 > 100-200 Standard of care Cessation of treatment of CMV retinitis, • CD4 > 200 Prophylaxis for HSV (genital or oral) • Outbreaks up-regulate HIV viral production and can threaten HIV viral suppression, shed both HSV and HIV CDC, MMWR 10
Therapies currently on market Emergencies Related to HIV Nucleoside and Protease inhibitors: NNRTI ’ s: Therapy nucleotide RTIs • Indinavir, IDV • Delavirdine (DLV) • Zidovudine, AZT ( Retrovir ) • Nevirapine, NVP ( Crixivan) • Abacavir, ABC ( Ziagen ) • Saquinavir, SQV ( Viramune) Mitochondrial toxicity • Lamivudine, 3TC ( Epivir ) • Efavirenz, EFV ( Invirase, hgc ) • • Lactic Acidosis Didanosine, ddI ( Videx ) • Nelfinavir, NFV ( Sustiva) • Stavudine, d4T ( Zerit ) • Etravirine* ( Viracept) Pancreatitis • Tenofovir, TFV ( Viread ) • Amprenavir, APV (Intelence) • Emtricitabine, FTC Rash by Non-Nucleoside Reverse ( Agenerase) Fusion ( Emtriva ) • Atazanavir, ATZ • Combivir (AZT/3TC) Transcriptase Inhibitors inhibitors: (Reyataz) • Trizivir (AZT/3TC/ABC) • Enfuvirtide, ENF • Fosamprenavir, FPV Drug interactions • Epzicom (3TC/ABC) or T20 ( Fuzeon) (Lexiva) • Truvada (FTC/TFV) Combination • Kaletra CCR5 receptor • A tripla (lopinavir/ritonavir) antagonist (EFV/FTC/TFV) • Tipranavir ( Aptivus) • Maroviroc (Selzentry)* • Darunavir ( Prezista)* Integrase inhibitor *Approved in past year • Raltegravir (Isentress)* Orange text – combination agents www.aidsmeds.com HIVinsite.com 11
www.epocrates.com Mitochondrial toxicity Nucleoside reverse transcriptase inhibitors (NRTIs) • Pancreatitis ( “ d ” drugs, ie: ddI, d4T, ddC) • Neuropathy ( “ d ” drugs) • Myopathy (AZT) • Hepatic steatosis and lactic acidosis (all) • Peripheral lipoatrophy (predominantly d4T) Fat Redistribution Mitochondrial toxicity ( “ lipodystrophy ” ) Lipodystrophy Syndrome • Thinning of the face, arms, or legs (lipoatrophy) • Fat accumulation in the belly and back. 12
Fat Wasting (NRTI) Truncal Obesity (PI ’ s) Buffalo Hump (PI ’ s) 13
Are HIV patients at increased Metabolic complications- risk of premature cardiovascular PI ’ s disease? Glucose metabolism Case Series/Reports: • Insulin resistance • increased levels of insulin • Early MI ’ s • Impaired glucose tolerance • CVA ’ s resistance and diabetes • higher rates of smoking • hypercholesterolemia • Hyperglycemia • substance use • hypertriglyceridemia • Frank diabetes • decreased HDL • increased visceral Lipid metabolism • increased rates of abdominal fat • Increased triglycerides atherogenic lipids • HTN • Increased total and LDL cholesterol, low HDL All of these are known to increase the risk of CAD. CAD may be the next wave of the epidemic. HIV infection is associated with HIV and MI: VA Study higher rates of CAD • Kaiser Permanente Study: CHD VA Aging Cohort Study from 2003 to 2009, hospitalization rate and MI rate significantly 82,459 patients higher in HIV pts vs. controls Outcome acute MI (871 events) • Partners HealthCare System: AMI rates higher HIV infection associated with a 50% in setting of HIV increased risk of AMI even after adjustment • Meta analysis of literature: 1.61 RR of CVD for for framingham risk factors, substance use, untreated HIV pts vs. controls, RR of 2.00 comorbidities (HR 1.48, 95%CI 1.27-1.72) among treated HIV pts vs. controls) Klein JAIDS 2002, Triant JCEM 2007, Islam FM HIV Medicine Freiberg MS et al JAMA Internal Medicine 2013 2012; DAD Study Group Lancet 2008 14
Recommend
More recommend