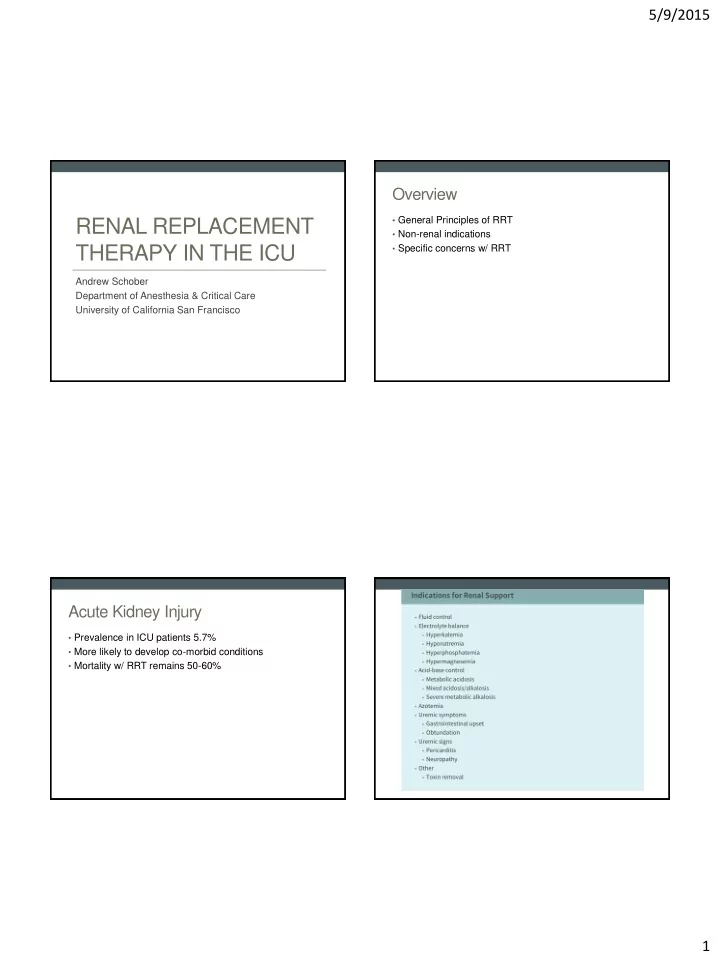
5/9/2015 Overview • General Principles of RRT RENAL REPLACEMENT • Non-renal indications THERAPY IN THE ICU • Specific concerns w/ RRT Andrew Schober Department of Anesthesia & Critical Care University of California San Francisco Acute Kidney Injury • Prevalence in ICU patients 5.7% • More likely to develop co-morbid conditions • Mortality w/ RRT remains 50-60% 1
5/9/2015 Ideal Renal Replacement Therapy • Controls volume • Corrects acid-base / metabolic abnormalities • Improves uremia / toxin clearance • Promotes renal recovery • Improves survival • Hemodynamic stability • Minimal bleeding / clotting complications Ronco. Critical Care Nephrology. 2008 Types of Therapy Modalities of RRT • Intermittent renal replacement Hemodialysis Hemofiltration • Intermittent hemodialysis (iHD) • PUF • Based on diffusion • Based on convection via hydrostatic pressure gradient • Dialysate flows countercurrent • Continuous renal replacement (CRRT) to blood • Plasma water removes solutes • CVVH / CVVHD / CVVHDF as ultrafiltrate • Urea, creatinine, K + diffuse • SCUF from blood to dialysate • Replacement fluid given pre- or • Peritoneal dialysis post-filter • Ca 2+ & Bicarb from dialysate to • Rarely utilized in ICU setting blood • Better for fluid removal • Hybrid therapies • Effective for clearing small • Effectively clears medium-sized molecules molecules / less efficient for • SLEDD small molecules • Extended daily dialysis 2
5/9/2015 CRRT Advantages Disadvantages • Lower flow rates greater • Slow removal of hemodynamic stability electrolytes/toxins • Continuous control of volume, • Cannot be performed via AV pH, electrolytes, uremia fistula • Theoretical benefit in certain • Continuous anticoagulation populations • Filter clotting (blood loss, gap • Unstable hemodynamics in therapy) • Less risk of cerebral edema • Hypothermia in hepatic failure / TBI • Electrolyte depletion • Removal of sepsis mediators • Not available in certain settings Ronco. Critical Care Nephrology. 2008 IHD CRRT vs. iHD : The Data CRRT vs. IRRT Meta-analysis (Rabindranath et al. Advantages Disadvantages Cochrane Database. 2008) • Less expensive • Osmotic shifts / Dialysis disequilibrium syndrome (CRF) • Does not require continuous anticoagulation • Higher rate of intra-dialytic hypotension • Fewer bleeding / clotting complications • Faster clearance of toxins 3
5/9/2015 CRRT vs. iHD : The Data When to choose iHD vs. CRRT CONVINT trial (2014) : • Single center, 252 pt , RCT iHD CRRT • No difference in mortality (14, • Severe hemodynamic • Severe, life-threatening 30d, in-hospital) instability electrolyte derangements • No difference in : All subjects • High catabolic states w/ • Rapid clearance of toxins • Days on RTT ongoing production of / overdose • Ventilator days toxins • Flash pulmonary edema • Vasopressor use • Removal of toxins w/ high • ICU/hosp LOS • Liberation from CRRT intracellular concentrations (e.g. Li + ) • Severe metabolic acidosis w/ inability to compensate Schefold et. al, Crit Care Med. 2014 High Vasopressors Hybrid Therapy : Is SLEDD the answer? • Essentially IHD at lower blood / dialysate flows for extended period of time ( > 5h ) Non-renal indications for RRT • 11h SLEDD equivalent to 23h CVVH* • Uses conventional dialysis machine • Similar hemodynamic stability to CRRT • Reduced anticoagulation requirement • Cheaper than CRRT • Difficulty / complicated drug dosing • Risk of underdosing antibiotics during 2 nd half of session * Fliser. Nature Clinical Practice – Nephrology. 2006 4
5/9/2015 Toxin Clearance : Volume Overload SCUF / PUF What makes a substance dialyzable? • Indicated for volume overload in pre-renal states (e.g. CHF) • Low molecular weight • Goal to remove plasma water not solute • Small volume of distribution (primarily blood > peripheral tissues) • UF not replaced, corresponds to negative fluid balance • High aqueous solubility • Can be performed w/ either continuous (SCUF) or intermittent (PUF) forms of therapy • Low protein binding • Renal > non-renal contribution to plasma clearance Commonly Dialyzable Drugs Sepsis : a special case for CRRT? • Salicylates • Clearance of inflammatory cytokines (endotoxin, IL-1, IL-6, IL- 10, TNF α) w/ CVVHDF* • Theophylline • High-volume hemofiltration (35L UF) appeared favorable in • Methanol / ethylene glycol / isopropanol non-controlled trials • Barbiturates • No affect on outcomes regardless of dose in multiple RCTs** • Lithium • Further studies w/ high cutoff membranes (greater cytokine • Depakote removal) & CPFA (coupled plasma filtration and adsorption) are ongoing • Carbamazepine • Dabigatran * Peng. Burns. 2005 ** Lehner. Minerva Anestesiol. 2014 5
5/9/2015 Catheter Site • Right IJ or femoral sites preferred ; Left IJ associated w/ higher rates of catheter failure* • Better performance & longer filter life w/ catheter tip in right atrium (vs. SVC)** Specific concerns with the patient on renal • Mobilization w/ femoral dialysis catheter safe (controversial) replacement therapy • no adverse events ; may increase filter life*** • ’d r isk of proximal vein stenosis w/ subclavian location * Parienti. Crit Care Med. 2010. ** Morgan. Am J Kidney Disease. 2012. ***Wang et al. Crit Care. 2014. Nutritional Supplementation Summary • Renal replacement therapy is complicated – work w/ your • RRT results in additional protein losses nephrologist to determine appropriate therapy based on • Protein supplementation local capabilities • Normal : 1-1.2 g/kg/day • Data equivocal btw modalities – may be specific situations • Renal Failure (w/o RRT) : 0.8-1.2 g/kg/day • iHD : 1.2 – 1.4 g/kg/day where one technique is preferred • CVVH : 1.6 – 2 g/kg/day • CRRT increasingly being used for non-renal applications – understand limitations and pitfalls as well as how to manage them 6
Recommend
More recommend