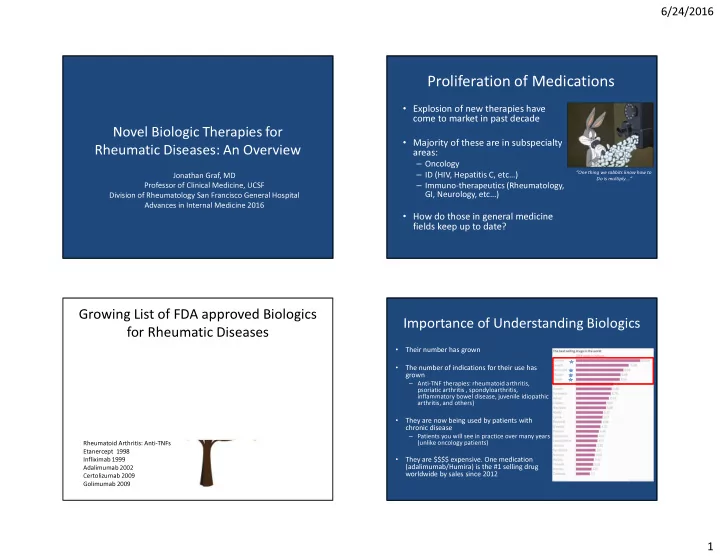
6/24/2016 Proliferation of Medications • Explosion of new therapies have come to market in past decade Novel Biologic Therapies for • Majority of these are in subspecialty Rheumatic Diseases: An Overview areas: – Oncology – ID (HIV, Hepatitis C, etc…) “One thing we rabbits know how to Jonathan Graf, MD Do is multiply….” – Immuno-therapeutics (Rheumatology, Professor of Clinical Medicine, UCSF GI, Neurology, etc…) Division of Rheumatology San Francisco General Hospital Advances in Internal Medicine 2016 • How do those in general medicine fields keep up to date? Growing List of FDA approved Biologics Importance of Understanding Biologics for Rheumatic Diseases • RA: Tocilizumab (anti-IL6R) Ank Spondylitis/Psoriasis/Psoriatic Arthritis: Their number has grown 2010 Secukinumab 2016 (anti IL17a) • The number of indications for their use has RA: Abatacept (CTLA4 Ig) Psoriatic arthritis: Ustekinumab (anti IL-12/23) grown 2005 2013 – Anti-TNF therapies: rheumatoid arthritis, RA: Rituximab: depleting B cell psoriatic arthritis , spondyloarthritis, ANCA vasculitis: inflammatory bowel disease, juvenile idiopathic Antibody 2006 Rituximab 2012 arthritis, and others) RA: Anakinra: IL1-RA • They are now being used by patients with 2001 SLE: Belimumab chronic disease (anti-BLyS) 2011 – Patients you will see in practice over many years (unlike oncology patients) Rheumatoid Arthritis: Anti-TNFs Periodic fever syndromes : Etanercept 1998 CAPS, muckle wells, NOMID • They are $$$$ expensive. One medication Infliximab 1999 Canakinumab (anti-IL1) 2009 (adalimumab/Humira) is the #1 selling drug Adalimumab 2002 Rilonacept (IL-1 TRAP) 2008 worldwide by sales since 2012 Certolizumab 2009 Golimumab 2009 1
6/24/2016 Overview of Today’s Talk Biologic Therapies • Anti-TNF therapy in detail – Most commonly used in practice • What is meant by the term “Biologic Therapy”? • When anti-TNF therapy for RA fails • Double meaning: – Anti-IL6 directed therapy (although there are other options) – Large complex organic products (mostly but not – Use this as example to show how indications are likely to necessarily proteins) synthesized by living cells increase beyond RA for biologics like this – Segue into discussion below: – Target a gene or protein and modify biologic responses • New small molecule “biological response modifiers” • Antibody-antigen interactions • Cytokine-receptor interactions (both ends) • Cell signaling proteins, inhibitors, or ligands • A lot of long-worded medications that sound alike: “imabs, umabs.” Don’t fret – discuss general principles Families of biological medications for Conventional vs. biological medication comparison rheumatic diseases • Anti-cytokine therapies – Block pro-inflammatory cytokines from binding Conventional medications Biological medications their receptors • • Larger complex molecules Small molecules – Anti-TNF, anti-IL6, anti-IL1, anti-IL 12/23, anti-IL 17 • Often organic: usually • Usually inorganic peptides/proteins • Cell-oriented therapies • • Encoded genetically, transcribed, Synthesized and purified translated, and then post – Removal of or prevent activation and/or chemically from inorganic translationally modified by living reactions cells proliferation of cells implicated in disease – Rituximab (B-cells), abatacept (T-cells) • Often can be difficult to identify full structure of complex • Structures can be identified = molecules that biologically easily manufacture generic constructed modified by cells 2
6/24/2016 Biological therapy for rheumatoid Anti-cytokine therapies arthritis • • Approaching two decades of Pro-inflammatory cytokines bind to receptors on cells and mediate experience with first class of inflammatory responses from biological medications (anti-TNF those cells medications) • Blockade of following cytokines significantly ameliorates these • Data have shown significant diseases – TNFa: RA, Psoriatic arthritis benefits not only in treating (PsA), psoriasis, ankylosing disease-associated symptoms spondylitis, juv. arthritis, IBD – IL 17: Psoriasis and PsA • Significant prevention of joint – IL 12/23: Psoriasis and PsA – IL 6: RA, ?giant cell arteritis erosion, narrowing, and McInnes et al. JCI 2008 – IL 1: periodic fevers (?gout) ultimately disability Benefits of adding an anti-TNF medication to Biologic therapies for rheumatoid arthritis conventional therapy with methotrexate Klareskog et al. Lancet 2004. Tempo Trial • Anti-Tnf medications (5 total) – Etanercept (TNF decoy receptor fusion protein) – Infliximab, Adalimumab, certolizumab, golimumab (variations of anti-TNF antibodies or fragments) • B-cell depleting agents – Rituximab • T-cell costimulation inhibitors (receptor-ligand ) – Abatacept • Inhibitors of IL-6 signaling – Tocilizumab (anti Il-6 receptor antibody) • Il-1 Inhibitors (IL-1 cytokine receptor decoy) – Anakinra 3
6/24/2016 Tumor Necrosis Factor-a Biologic therapies for rheumatoid arthritis • Anti-Tnf medications (5 total) – Etanercept (TNF decoy receptor fusion protein) – Infliximab, Adalimumab, certolizumab, golimumab (variations of anti-TNF antibodies or fragments) • B-cell depleting agents – Rituximab • T-cell costimulation inhibitors (receptor-ligand ) – Abatacept • Where does it come from? • Inhibitors of IL-6 signaling – TNF genes located on chromosome 6 (MHC) – Tocilizumab (anti Il-6 receptor antibody) – Primarily Macrophage and Monocyte derived • Il-1 Inhibitors (IL-1 cytokine receptor decoy) – Anakinra – Some also produced in T Cells and Synoviocytes TNF Effects: Good and the Bad Natural Biological Effects of TNF GOOD BAD • • TNF-alpha regulates biological TNF-a binds membrane- functions necessary for normal bound TNF receptors and inflammatory, immune, and mediates pro-inflammatory tumor surveillance responses. processes implicated in – TNF-alpha absolutely essential inflammatory arthritis. for granulomatous host defenses against intracellular bacteria (MTb, fungal infections, listeria) McInnes et al. JCI 2008 – Explains infection-related toxicity profile of these medications 4
6/24/2016 Anti-TNF Family Anti-TNF medications Anti-Tnf medications – Etanercept (TNF receptor fusion protein) – Infliximab (anti-TNF antibody) – Adalimumab (anti-TNF antibody) – Certolizumab pegol (anti-TNF Fab-PEG) – Golimumab (anti-TNF antibody) Etanercept Most of other anti-TNF monoclonal Abs Practical issues to consider in patients on long Contraindications term anti-TNFs: Pharmacokinetics... • History of latent tuberculosis unless/until they have • Anti-TNF medications have long half lives completed an adequate courses of prophylactic therapy (Duration up for debate) • This is important for duration of the biologic effect • Active acute or chronic infections (HCV exception) • Also important in case someone develops a side effect or infection while on one of these medicines • Active or suspected malignancies. – Etanercept 4.25 days – Infliximab 8-12 days • Anti-TNFs are generally contraindicated in patients with – Adalimumab 14 days moderate or severe congestive heart failure (some have black box warning) • Many patients, especially those on IV therapy, (infliximab, rituxan, etc…) may not mention to their MD • History of demyelinating disease that they are on therapy 5
6/24/2016 Initiating and monitoring therapy Initiating Anti-TNF Therapy • Screening for active infections by history in all • Asses Latent TB status at baseline patients on active therapy – PPD or interferon release assay – Follow up CXR if necessary (I recommend CXRs on all – Hepatitis B (will be discussed shortly) high risk patients) • Initiate treatment for LTBI if necessary (I recommend holding therapy in high risk patients until they have • If patients are being treated in our office, screen completed a significant amount of their regimen) for illness (history, temperature and blood • Other intracellular organisms with latent infection: pressure) before infusions or injections – Consider coccidiomycosis and histoplasmosis in endemic regions before prescribing (should weigh into decision of risks/benefits) – Counsel patients to do the same if being treated at home and hold doses if ill. If truly sick – seek MD attention • Age appropriate cancer screening - good idea Infliximab and TB Anti-TNFs: Adverse Events Keane et al. N Engl J Med. 2001 Oct 11;345(15):1098-104 • Most common: Injection site reactions – Tend to wane over time and with use • Most serious: Increased risk of infections! (OR of 2.0 for serious infection in large meta analysis published in JAMA 2006) – Most common URIs – Problematic: mTB and other intracellular organisms for which TNF is necessary for immune containment • Increased malignancy risk: Controversial 56% Extra Pulmonary TB • May worsen symptoms of congestive heart 24% Disseminated disease failure. Patients don’t make granulomas (atypical appearance) Average onset 12 weeks after initiation (3-4 th dose) 6
Recommend
More recommend