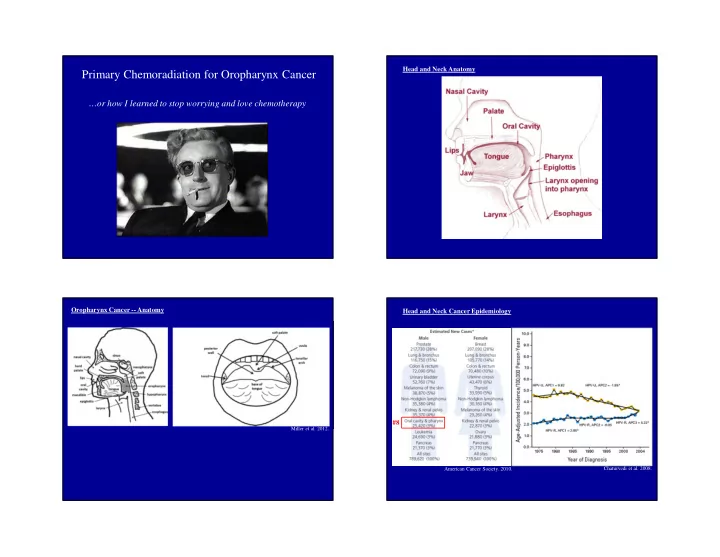
Head and Neck Anatomy Primary Chemoradiation for Oropharynx Cancer …or how I learned to stop worrying and love chemotherapy Oropharynx Cancer -- Anatomy Head and Neck Cancer Epidemiology #8 Miller et al. 2012. American Cancer Society. 2010. Chaturvedi et al. 2008.
Oropharynx Cancer: HPV and Prognosis “Curing” HNSCC ’’ Curative modalities: Surgery, radiation Chemotherapy not curative, may potentiate radiation Curable stages: Localized Regionally advanced - Resectable - Radiation possible (maximum lifetime dose) Incurable: Recurrent – no further radiation or surgery possible Metastatic Chaturvedi et al. 2011. Oropharynx SCC Staging Oropharynx Simplified Decision Tree T Size Invasion N # Size Side T Size Invasion N # Size Side T1 < 2 cm N0 0 T1 < 2 cm N0 0 T2 2-4 cm N1 1 < 3 cm Ipsilateral T2 2-4 cm N1 1 < 3 cm Ipsilateral T3 > 4 cm +Lingual surface N2a 1 3-6 cm Ipsilateral T3 > 4 cm +Lingual surface N2a 1 3-6 cm Ipsilateral +Epiglottis +Epiglottis N2b >1 < 6 cm Ipsilateral N2b >1 < 6 cm Ipsilateral T4a +Larynx T4a +Larynx N2c < 6 cm Contralateral N2c < 6 cm Contralateral +Tongue muscles +Tongue muscles Bilateral Bilateral +Medial pterygoid +Medial pterygoid +Hard palate N3 > 6 cm +Hard palate N3 > 6 cm +Mandible +Mandible T4b +Lateral pterygoid T4b +Lateral pterygoid M Distant metastases M Distant metastases +Pterygoid plates +Pterygoid plates +Lateral nasopharynx +Lateral nasopharynx M0 M0 +Skull base +Skull base M1 Present M1 Present +Encases carotid +Encases carotid Surgery and/or XRT Definitive chemoradiation ≥ Stage I ≥ Stage III ≥ Stage IVb Chemoradiation Palliative therapy ≥ Stage II ≥ Stage IVa Stage IVc Surgery + XRT +/- Chemo
Glottic Larynx Decision Tree Rationale for concurrent chemoradiation in OPC Metaanalysis of chemotherapy in head and neck cancer (MACH-NC) 87 trials, 16,665 patients, median 5.5 years f/up Blanchard et al. 2011. Glottic Larynx Decision Tree Rationale for concurrent chemoradiation in oropharyngeal carcinoma Risk of Death @ 5 years Absolute HR p risk Sequence Adjuvant +0.4% 1.15 p < 0.0001 Neoadjuvant - 1.4% 1.00 Concurrent - 8.1% 0.78 Chemo Platinum + 5FU 0.83 p < 0.004 Platinum 0.70 Single agent non-platinum 1.01 Take Home: 1. Concurrent 2. Platinum Blanchard et al. 2011.
Single agent regimens with XRT Combination chemotherapy + XRT Oropharynx/Mixed: RT vs chemoRT GORTEC 1 Intergroup 2 Pts 113 109 95 87 89 70 Gy 70 Gy 70 Gy 70 Gy 30 Gy, break, RT 35 fx 35 fx 35 fx 35 fx surgery vs boost Chemo carbo/5FU cisplatin cisplatin/5FU OS 5 yr 16% 5 yr 22% 3 yr 23% 3 yr 37% 3 yr 27% 56% late 77% acute Toxicity 30% late 52% acute 89% acute Dry mouth, cervical N, V, mucositis fibrosis MACH-NC 3 year OS = 41.1% 5 year OS = 32.7% Seiwert TY et al . (2007) Nat Clin Pract Oncol 4 : 156–171 1. Calais G, JNCI 91:2081-6, 1999 � T3+ and N3 tumors? 2. Adelstein, JCO, 21(1):92, 2003 Wait a minute… Cetuximab Median LRC 24.4 vs 14.9 months OS 49.0 vs 29.3 months Does it have to be chemo therapy? Bonner et al. 2006. Chemo 2. Robert Arneson. 1992.
A few burning questions XRT +/- Novel EGFR inhibitor (Nimotuzumab) HPV+ 1. Deintensify? 1. Cetuximab = cisplatin? All OPC 1. Better induction? 2. New therapies a. Targeted b. Immune Trials: HPV+ deintensify radiation Trials: HPV+ cetuximab vs cisplatin E1308: HPV-specific Trial RTOG 1016 Chemotherapy-Cetuximab to Select HPV+ Oropharynx Patients for Lower Dose Radiation cisplatin vs cetuximab head to head INDUCTION (3 cycles) ELIGIBILITY CONCURRENT Stage IMRT 54Gy/27 fxs Weekly III,IVA,B CR Paclitaxel Cetuximab 250mg/m2 Resectable qwk + HPV + Cetuximab Oropharynx CONCURRENT IMRT 69.3Gy/33fxs <CR N=83 Cetuximab 250mg/m2 qwk Cetuximab loading dose = 400mg/m2 on Day1 of Cycle1 with Induction
Induction therapy: regimen Induction therapy: regimen TAX 324: Docetaxel/Cisplatin/5-FU vs Cisplatin/5-FU Sequential TAX 324: TPF vs PF Sequential Therapy in Advanced SCCHN Therapy in Advanced SCCHN Survival PFS ICT CRT 100 100 Docetaxel (75 mg/m 2 ) 90 Log-rank P =0.0058 90 Log-rank P =0.004 Survival Probability (%) Cisplatin (100 mg/m 2 ) 80 80 HR=0.70 PFS Probability (%) R HR=0.701 5-FU (1000 mg/m 2 /day, 70 70 A 96-hr C-I) Chemotherapy- and RT-naïve 60 60 N every 3 weeks, 3 cycles Carboplatin stage III/IV SCCHN 50 D 50 TPF 67% (AUC 1.5 weekly) • Oral cavity, oropharynx, O 40 40 TPF 53% PF 54% Daily RT hypopharynx, larynx M TPF 62% 30 30 PF 42% (5 days/week) Cisplatin (100 mg/m 2 ) TPF 49% I PF 48% 20 20 N=501 TPF (N=255) 5-FU (1000 mg/m 2 /day, TPF (N=255) PF 37% Z 10 10 PF (N=246) PF (N=246) days 1-5) E 0 0 every 3 weeks, C-I 3 cycles 0 6 12 18 24 30 36 42 48 54 60 66 72 0 6 12 18 24 30 36 42 48 54 60 66 72 Months Months • TPF improves survival and PFS compared with PF Posner, N Engl J Med. 2007;357:1705. Posner, N Engl J Med, 2007;357:1705. Induction therapy: additional thoughts But the questions still is: do we need induction? Induction+CRT vs CRT • May need larger number in subgroups DeCIDE and PARADIGM Regimen Trial Population N Induction CRT 3y OS PARADIGM 1 Stage II-IV 145 Docetaxel + Weekly 73%* Cisplatin + carboplatin or 5-Fluorouracil docetaxel Cisplatin 78%* (q3w x2) DeCIDE 2 N2/N3 280 Docetaxel + Docetaxel + 75%* Cisplatin + Hydroxyurea + SCC head 5-Fluorouracil 5-Fluorouracil and neck Docetaxel + 73%* Hydroxyurea + 5-Fluorouracil *Not significant 1. Haddad et al., ASCO 2012. 2. Cohen et al. ASCO 2012.
Induction therapy: additional thoughts Conclusions Clinical judgment / scenario • � HPV+ oropharyngeal carcinoma • HPV+ prognosis better, but treated like HPV- for now – Radiation field too big • Chemoradiation for advanced stage – Patient too sick • Concurrent, platinum Weekly carboplatin and paclitaxel • Research may identify relative efficacy of less toxic agents Moosmann et al. 2003.
Recommend
More recommend