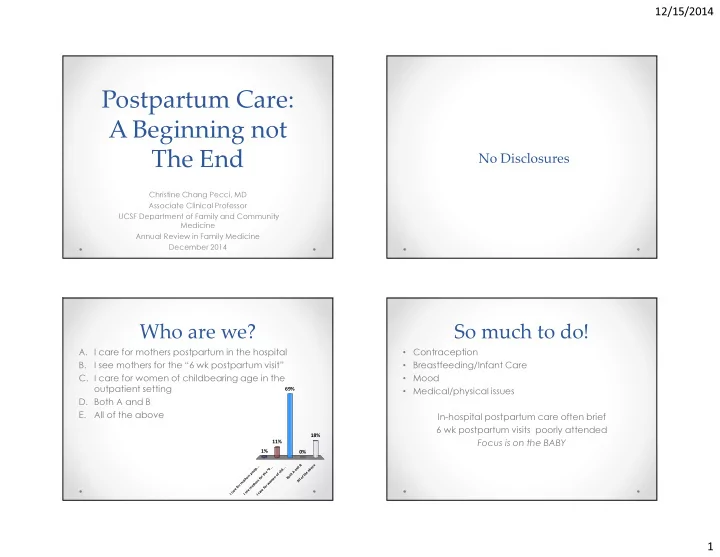
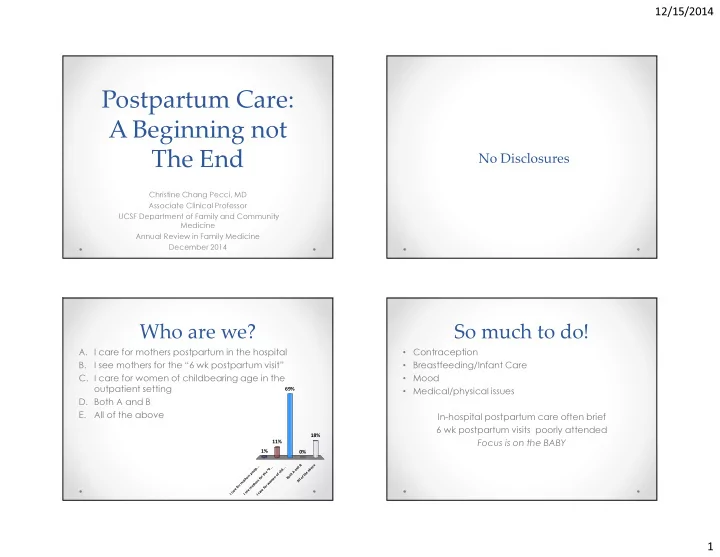
12/15/2014 Postpartum Care: A Beginning not No Disclosures The End Christine Chang Pecci, MD Associate Clinical Professor UCSF Department of Family and Community Medicine Annual Review in Family Medicine December 2014 Who are we? So much to do! • Contraception A. I care for mothers postpartum in the hospital • Breastfeeding/Infant Care B. I see mothers for the “6 wk postpartum visit” • Mood C. I care for women of childbearing age in the • Medical/physical issues outpatient setting 69% D. Both A and B E. All of the above In-hospital postpartum care often brief 6 wk postpartum visits poorly attended 18% 11% Focus is on the BABY 1% 0% Both A and B All of the above I care for mothers postp... I see mothers for the “6 .. I care for women of chil... 1
12/15/2014 Maximizing the Post-partum Visit What more could we be doing? • Interconception Care Project for California • Focus on longer term maternal health issues in • March of Dimes and ACOG addition to short term issues District IX Project with • Realize that postpartum care has larger implications Preconception Health Council for women and their families of California (PHCC) • Redefine postpartum period as the beginning of • Goal: Produce post-partum care guidelines for obstetric interconception care providers that incorporate risk assessment based on the previous pregnancy and develop recommendations for future care Preconception Health and the Life ICPC Guidelines Content Areas Course Perspective • Alcohol Use • Postpartum Depression Excellent Health • Anemia • Preeclampsia Exercise Optimal • Domestic Violence • Preterm Birth Education Healthy Birth Outcome Health Care Relationships • Gestational Diabetes • Cesarean Section Family Planning Financial Security Safe Neighborhood Planned Pregnancy • Gonorrhea and Chlamydia • Seizure Nutrition Healthy Relationships • Hepatitis • Substance Abuse Protective Factors Risk Factors Social Support Disparity at Birth • HIV • Syphilis Poor Nutrition • Hypertension • Thrombocytopenia Obesity Unsafe Neighborhood Poor Education • Migraine • Thyroid Disorder Adverse Lack of Health Care Poverty Childhood Events No Family Planning No Social Support • Obesity • Tobacco Use Exposure to Toxins Tobacco/Alcohol/Drugs Mistimed Pregnancy • Vaccinations Poor Birth Health Poor Outcome Conception Birth Age 5 Puberty Pregnancy Delivery Pregnancy 2
12/15/2014 Rubella • Do not give during pregnancy and avoid pregnancy x 28 days • Not an indication for termination • If lab evidence of immunity, no need to repeat • If neg or equivocal titer after 1-2 doses, give third dose and stop checking titers • Ok for children of pregnant women to get • May give with Rhogam, check titer in 3 months MMWR June 2013 9 Varicella • Lab evidence of immunity or • Mary is 36 yo G2P2 delivered 2 days ago via disease cesarean delivery. She had declined the Tdap and • Birth in US before 1980 is not flu shot pregnancy because she was afraid of it hurting the baby. Now she is willing to accept these sufficient for pregnant two immunizations if you still recommend them. She women got the flu shot last season and got a Tdap after her • Diagnosis or verification of last pregnancy in 2011. history of varicella or zoster by health care provider o Should have link to a typical case or lab confirmation if testing done during acute infection 3
12/15/2014 What immunizations Tdap should she get? • If not given prenatally between 27-36 weeks, no A. Tdap only need to give postpartum if up to date • Immunize other family members B. Influenza only 66% C. Both D. Neither 33% Answer B 1% 0% y y h r l l t e n n o h o o B t i p a e N a z d n e T u l f n I Short Interpregnancy Interval • Preterm birth, SGA, LBW and perinatal death o IPI <3 months 60% LBW c/w 13-14 months o IPI <6 months 30% LBW c/w 18-23 months o IPI < 5 mo 15% SGA c/w 12-23 months • PPROM, cardiovascular defect, autism • Anemia, placental abruption, endometritis, placenta previa, uterine rupture Shachar BZ, Lyell DJ. I Obstet Gynecol Surv 2012;67:584-96 Zhu BP et al NEJM1999 Grisaru-Granovsky S Contraception.2009 4
12/15/2014 What is the causal factor? Is there an ideal IPI? • Maternal depletion • WHO and US Agency for International Development o o protein, macro and micronutrients Recommend IPI > 2 years after a live term birth o o evidence not clear IPI >5 years increased risk for adverse outcomes o • Folate depletion Aligns with WHO breastfeeding recommendation • Studies support IPI 18-24 months o Low 3-4 months PP; improve w supplementation o o Strong evidence birth to conception o • Cervical insufficiency 12 months for moms >35 yo o collagen concentration in cervix not normalized until 12 months PP • Inflammation Conde-Agudelo A, Rosas-Bermudez A, Castano F, Norton MH. Stud Fam Plann 2012;43:93-114 Wendt A, Gibbs CM, Peters S, Hogue CJ. Paediatr Perinat Epidemiol 2012 California Unintended Pregnancies Almost half of live births in California result from unintended pregnancies 70 64.8 60 49.4 50 State Total 44.6 Percent (%) 40 37.1 33.0 30 Black 20 Hispanic White 10 Asian/Pacific Islander 0 Black Hispanic White Asian/Pacific Islander Percent of mothers in California with a recent live birth by race/ethnicity, 2007 Data Source: Maternal and Infant Health Assessment Survey 19 5
12/15/2014 Lactation Amenorrheic Method Nonbreastfeeding • Fully breastfeeding or nearly full • Mean day 1 st ovulation 45-94 day breastfeeding and amenorrhea o 98% effective x first 6 months • Mean 1 st menstruation 45-64 • 20-71% first menses preceded by ovulation but • Exclusively breastfeeding more than half abnormal (30-100%)(compromised o Total contraception x 10 weeks fertility) • Earliest day of ovulation day 25 Bellagio Consensus Statement: Breastfeeding as a Family Planning Method, The Lancet, 19 November 1988 Not fully breastfeeding Rule of 3s • Ovulation returns 6 wk after • Fully Breastfeeding o Initiate contraception at 3 months postpartum supplementation • Not breastfeeding • Half of women not fully breastfeeding o Initiate contraception at 3 weeks postpartum resume menses by 6 weeks 6
12/15/2014 What would you offer her? • Mary (36 yo G2P2 s/p CS; BMI 35) was discharged A. Progestin only pill (POP) because you on POD #4. She was certain she was not going to hope she will go back to breastfeeding have intercourse but promised that she would use B. POP because her risk of DVT right now is 45% condoms if it happened. She left the hospital too high postpartum to start on COC breastfeeding and was breastfeeding well when 37% you saw her a week later for her baby’s first visit. C. COC because she has stopped • She comes in for a 3 week postpartum visit. She breastfeeding and it is more effective found it too difficult to breastfeed with all her other than POP 12% responsibilities. She is interested in taking “the pill”. D. Talk her into using a LARC (implant, IUD) 7% She wants to wait at last 2 years before getting pregnant again. She suspects that she may be having intercourse in the next week. . . . . . . . R . ) . . . P . o A f t O o s L P k s a a ( s g l i h l r n p i r e i h s e u y h s l o n e e o t s s n u u n a a i i r t c c e s e e e h b b g k o P C l O a r O T P C P Kind of a trick question… Progestins • Considered safe even immediately postpartum • Progestins are transferred via breastmilk • Theorectical concerns but no harms seen Answer : NOT C WHO 3 <6 weeks US Med Eligibility Criteria 2 <1 month breast 1 No breast UK Medical Eligibility Criteria 1 7
12/15/2014 OCPs and breastfeeding Initiating COC postpartum • COCs decreases quality and quantity of breastmilk • VTE risk increases by 2-5x postpartum but no difference in infant growth or • Risk declines by more than half second week supplementation in well nourished moms postpartum • Returns to baseline at 4-6 weeks • COC associated with decreased rate of breastfeeding after 6 months • Exogenous estrogens increase hepatic synthesis of several clotting factors 3x-7x • POP modest increase in milk production; breastfeed longer and later time to supplementation Jackson,Emily Obstet Gynec 2011 WHO classification for COC • No one should get COC < 21 days pp (4) • If risk factors, don’t start prior to 42 days (3) o Age >35, prev VTE, thrombophilia, immobility, transfusion at delivery, BMI >30, PPH , post CS, preeclampsia, smoking • If no risk factors, can start 21-42 days (2) MMWR July 8, 2011 60(26);878-883 8
Recommend
More recommend