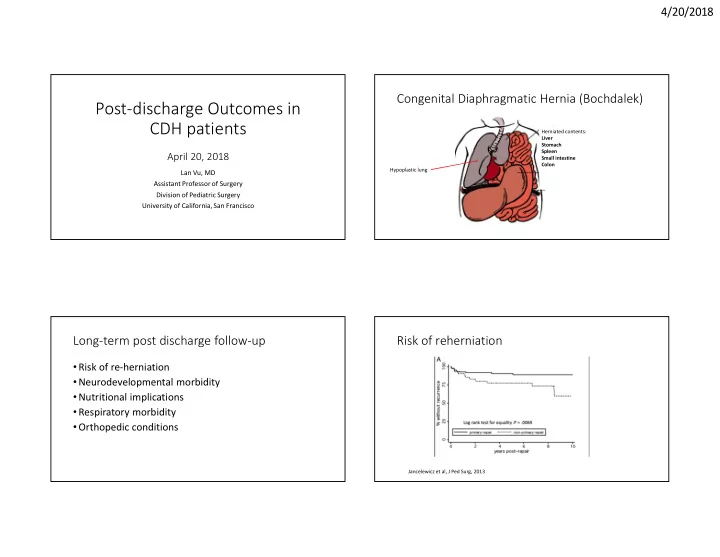
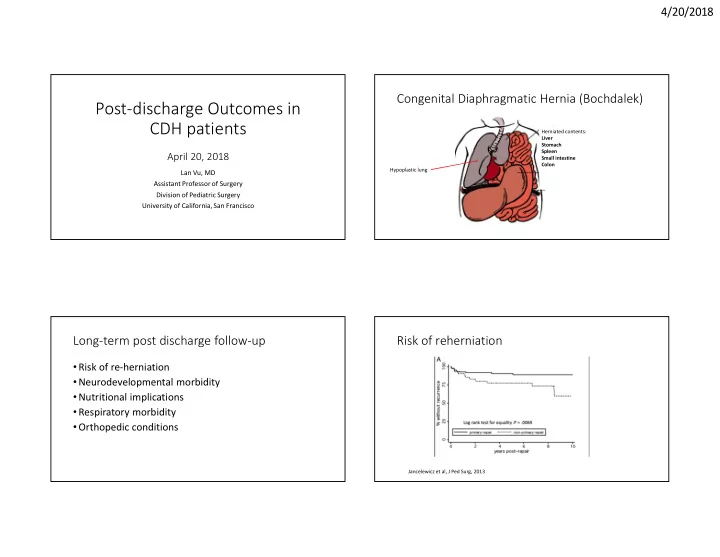
4/20/2018 Congenital Diaphragmatic Hernia (Bochdalek) Post-discharge Outcomes in CDH patients Herniated contents: Liver Stomach Spleen April 20, 2018 Small intestine Colon Hypoplastic lung Lan Vu, MD Assistant Professor of Surgery Division of Pediatric Surgery University of California, San Francisco Long-term post discharge follow-up Risk of reherniation • Risk of re-herniation • Neurodevelopmental morbidity • Nutritional implications • Respiratory morbidity • Orthopedic conditions Jancelewicz et al, J Ped Surg, 2013 1
4/20/2018 Diaphragm Diaphragm Reherniation 2
4/20/2018 Neurodevelopment impairment • Hearing loss • Motor dysfunction • Cognitive delays • Sensory processing disorders/autism spectrum • Behavioral disorders (ADHD) High-Risk Infant Follow-up Program at UCSF What has been published? • Structured medical, social, developmental history and exam • Cortes, Keller et al (2005): no difference in NDI at 1 and 2 years between tracheal occlusion and conventionally treated CDH, but • 6, 12-18, 30 months, and 4.5 years (8-12 years of age for subset of overall high rates of morbidity research subjects) • >50% with cognitive delays • Prior to 2009, children with CDH were standardly followed to 30 • 40% with neuromotor delays months of age • 7/16 with hearing loss requiring amplification between 2.5-5 years of • All patients in TO trial were evaluated between 2.5-5 years age • Extended to visits at 4.5 years since 2009 3
4/20/2018 NDI and CDH NDI and CDH • Danzer et al (2010): moderate to severe delays in psychomotor, • Predictors of poor outcome: cognitive, or language scores on Bayley-3 testing in 41 CDH patients - ECMO born between 2004-2007 < 3 year olds - supplemental oxygen at 28 days - tube feedings at discharge • > 50% had moderate to severe delays in at least one domain - lower socioeconomic status • 51% abnormal muscle tonicity • 7% rate of autism - rehospitalization in the first 2 years of life Wynn J, et al. J Pediatr Surg. 2013 Oct Older patients with CDH Nutritional implications • Older assessments more favorable than those < 3 years • Poor growth • At preschool age, 22% had borderline scores • Gastrostomy tube dependence • 11% showed significant delays in at least one domain • Oral feeding difficulties/aversion • Danzer et al. , Preschool neurological assessment in congenital diaphragmatic hernia survivors: outcome and perinatal factors associated with • Gastroesophageal reflux disease neurodevelopmental impairment. Early Hum Dev. 2013 Jun. • At 9 years of age in survivors, outcomes in 33 patients were not statistically different than norms, except in motor dysfunction • Tureczek I, Long-term motor and cognitive outcome in children with congenital diaphragmatic hernia. Acta Paediatr. 2012 May 4
4/20/2018 First few years of life • Childhood and adolescence • Leeween et al, J Ped Surg, 2014 (single center, cohort of 24 pts) Haliburton et al, J Ped Surg, 2015 (single center, ages 5-17 years, N=116) - FTT (z scores > -2.0 in weight for age and/or weight for length): 63% in the first 6 months • 25% feeding tubes (FT) placed - Catch up growth occurs between 6-12 months: FFT only in 21% of cohort at 12 during infancy - 60% remained at 7 years of age month visit • Those with FT were shorter and lighter (similar BMI) • Increased REE in 58% of patients (based on indirect calorimetry) Natural history of pulmonary hypertension • Lusk et al, J Pediatr, 2015 (single center, 140 patients) Respiratory Issues - 98 had resolution of pulm HTN at discharge/death - mean time to resolution 18 days • Pulmonary hypertension • Chronic lung disease 5
4/20/2018 • Wong et al, J Ped Surg, 2018 (single center) - PH generally resolves by age 5 years Risk of pneumonia - Lung perfusion scans do not change over time (unclear reason for PH resolution) • Reported as 7% within the first year of life • Both aspiration and infectious • Preventive measures: - treatment of chronic lung disease and other associated conditions (oromotor dysfunction, GERD) - appropriate vaccination (RSV vaccination for the first two years: recommended in the AAP policy statement, 2003). Long term pulmonary sequelae in adult survivors of CDH Orthopedic Conditions • Vanamo et al, J Ped Surg, 1996 (Finland) • Type of repair (primary, patch, muscle flap) - 60 patients (age 11-41 years) • Surgical approach (thoracotomy, laparotomy) - self report: 12% asthma, 7% increased susceptibility to infxn - PFTs: 51% had ventilatory impairment • Differential growth of the lung 15% obstructive 12% restrictive 25% mixed obstructive and restrictive 35% had bronchial hyperreactivity 6
4/20/2018 Conclusions • Multiple factors contribute to chronic conditions • Improvement seen with time • Multidisciplinary follow-up is needed in patients with CDH - pediatric surgeon - nutritionist - neurodevelopmental team - cardiologist - pulmonologist - social worker - feeding therapist 7
Recommend
More recommend