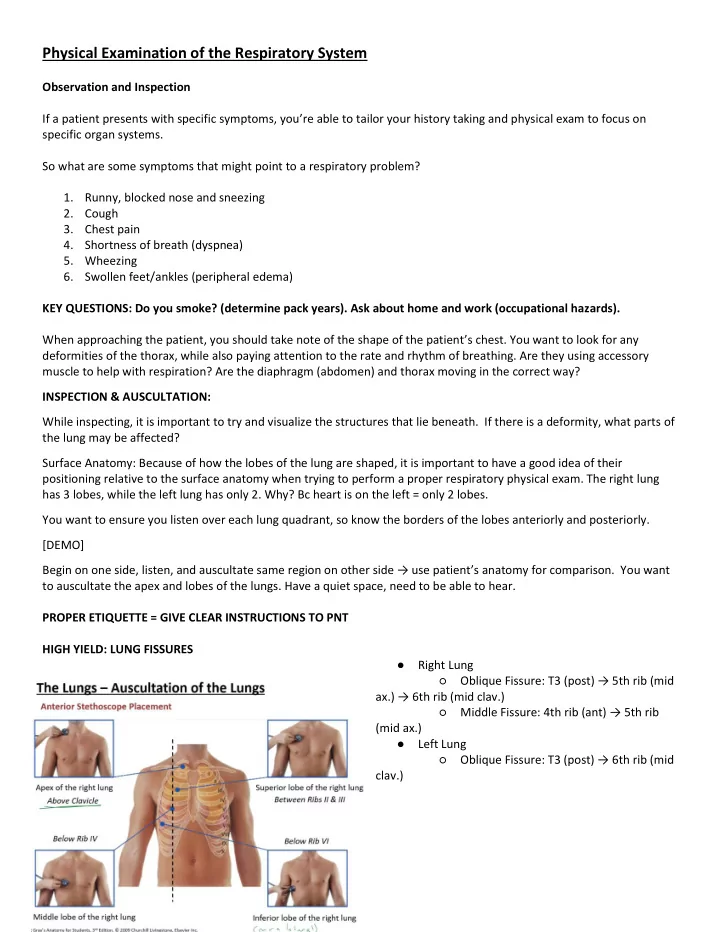
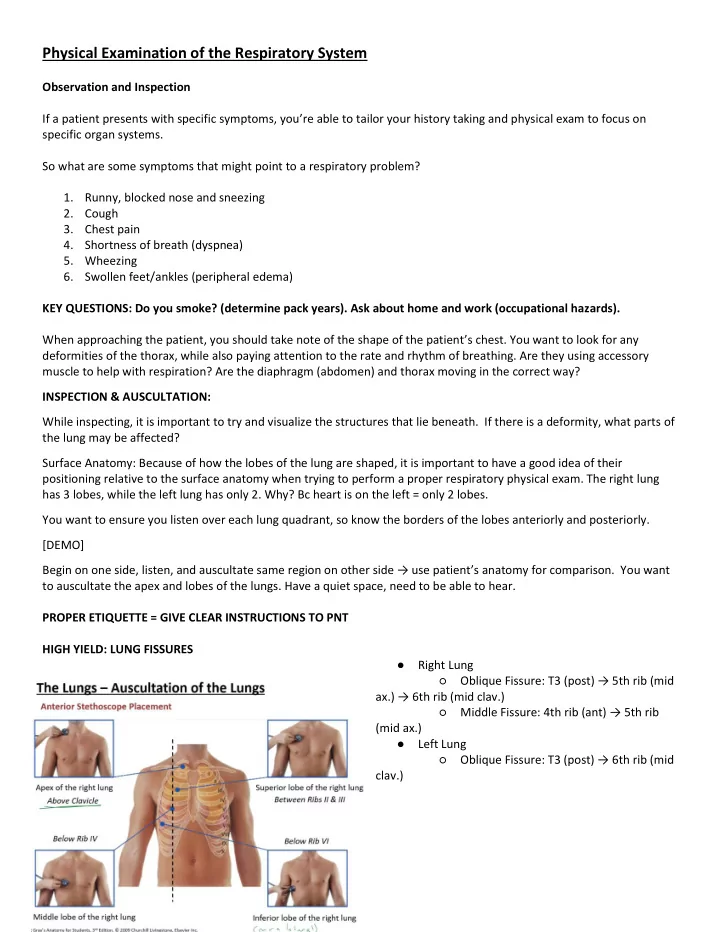
Physical Examination of the Respiratory System Observation and Inspection If a patient presents with specific symptoms, you ’ re able to tailor your history taking and physical exam to focus on specific organ systems. So what are some symptoms that might point to a respiratory problem? 1. Runny, blocked nose and sneezing 2. Cough 3. Chest pain 4. Shortness of breath (dyspnea) 5. Wheezing 6. Swollen feet/ankles (peripheral edema) KEY QUESTIONS: Do you smoke? (determine pack years). Ask about home and work (occupational hazards). When approaching the patient, you should take note of the shape of the patient ’ s chest. You want to look for any deformities of the thorax, while also paying attention to the rate and rhythm of breathing. Are they using accessory muscle to help with respiration? Are the diaphragm (abdomen) and thorax moving in the correct way? INSPECTION & AUSCULTATION: While inspecting, it is important to try and visualize the structures that lie beneath. If there is a deformity, what parts of the lung may be affected? Surface Anatomy: Because of how the lobes of the lung are shaped, it is important to have a good idea of their positioning relative to the surface anatomy when trying to perform a proper respiratory physical exam. The right lung has 3 lobes, while the left lung has only 2. Why? Bc heart is on the left = only 2 lobes. You want to ensure you listen over each lung quadrant, so know the borders of the lobes anteriorly and posteriorly. [DEMO] Begin on one side, listen, and auscultate same region on oth e� side → use patie�t’ s anatomy for comparison. You want to auscultate the apex and lobes of the lungs. Have a quiet space, need to be able to hear. PROPER ETIQUETTE = GIVE CLEAR INSTRUCTIONS TO PNT HIGH YIELD: LUNG FISSURES ● Right Lung ○ Oblique Fissure: T� �post� → �th �i� ��id a�.� → �th �i� ��id �lav.� ○ Middle Fissu�e: �th �i� �a�t� → �th �i� (mid ax.) ● Left Lung ○ O�li�ue Fissu�e: T� �post� → �th �i� ��id clav.)
Starting ANTERIORLY: ● Apex: above the clavicle, ask patient to breath normally and listen for 1-2 breaths. Listen to the same spot on other side. ● Superior lobe: Right + Left: 2nd IC space at the midclavicular line . Use the angle of louis to find this spot. ● Middle lobe: right side, 4th IC space ● Inferior lobe: R + L: for the lower lobes, listen in the mid axillary lines in the 6th IC space . ● Posteriorly: You can only auscultate the superior and inferior lobes. Good trick is to have pnt raise arms and place hand on head. Scapula can delineate the upper and lower lobes. ( T3 to 5th IC ) [NOTE: CLinically, you ’ ll start posteriorly, then anteriorly listen to middle lob and proceed to heart PE. If you hear something, then do a full anterior exam] What do you WANT to hear? BREATH SOUNDS: 1. Inspiratory and expiratory sounds are equal. Some abnormal sounds: Narrow or obstructed airway s: ● Rhonchi: continuous low pitched, rattling lung sounds , often resembles snoring. Often OBSTRUCTIVE cause, seen in COPD, pneumo , cystic Fibrosis. ● Wheezes: continuous noise, constriction of bronchioles, see in asthma and bronchitis. ( musical quality, high pitched ) Others ● Crackles/Rales: discontinuous, smaller airways, fluid in lungs . Seen in CHF, pneumo. ● Rubs (sounds like rubbing hair): usually discontinuous, Pleural friction rubs are low-pitched, grating, or creaking sounds that occur when inflamed pleural surfaces rub together during respiration . More often heard on inspiration than expiration, the pleural friction rub is easy to confuse with a pericardial friction rub. To determine whether the sound is a pleural friction rub or a pericardial friction rub, ask the patient to hold his breath briefly. If the rubbing sound continues, it is a pericardial friction rub because the inflamed pericardial layers continue rubbing together with each heartbeat - a pleural rub stops when breathing stops. [DEMO] PERCUSSION: A controlled blow that sets up a vibration in tissue. The vibration is transmitted differently if underlying tissue is air or fluid filled or solid. Air filled = resonant or tympanic sounds. Leave on finger on the chest wall (called the pleximeter, surface being struck) Strike finger with one or two fingers. Is the sound dull or resonant? → Test skills: t�� o� �i�, a�d the� i� IC spa�e. The �i b will make a duller sound, good to hear difference.
RATE & RHYTHM: As you listen and discuss symptoms with Pnt, you can assess the rate and rhythm of breathing. ● How long should you try and watch for? 30 secs ● What ’ s a normal RR? About 12, +/= 4 breaths per minute in an adult. (count for 30 secs, x2) ○ Infants 30-60 ○ Kids: 20-30 ● Tachypnea (abnorm. Rapid breathing) = >20 ○ Tachypnea can be caused by a number of conditions. Chronic conditions like asthma, lung disease, anxiety, or obesity can lead to tachypnea. It may also be caused by acute conditions like pulmonary embolism (blood clots in lungs), choking, heart failure, shock, or heatstroke. Lung infections can also cause tachypnea. ● Bradypnea = < 8 ○ One of most common: Narcotics (ex. Benzos, opioids), hypothyroidism (cushing ’ s). Also pulmonary obstructions, increased intracranial pressure, obesity, alcohol consumption, and cardiogenic shock. RESP PATTERN: ● Usually it ’ s rhythmic and regular, with insp to exp ratio being 1:2 ● Prolonged expiration can suggest underlying OBSTRUCTIVE impairment ● Rapid shallow breathing (1:1) suggest restrictive impairment. ● Abnormal Sounds: ○ Cheyne-Stokes breathing (gradual increase in resp. rate, decrease, increase, rhythmic), ■ Sign of Heart Failure. (Also sign of central s leep ap�ea, da�age to �esp �e�te�s i� the ��ai� → T� IPAP) ○ Kussmaul breathing (sounds like you just ran): It is a form of hyperventilation, which is any breathing pattern that reduces carbon dioxide in the blood due to increased rate or depth of respiratio � → e�. I� metabolic acidosis. ○ Abdominal paradox: diaphragm goes down and thorax expands in normal breathing. If thorax goes out and abdomen in, sign of diaphragmatic dysfunction (possibly paralysis) OTHER SIGNS ON PE: Signs of resp distress can include tachypnea. Is there accessory muscle use when breathing? T�ipod positio�: sig� of �esp dist�ess → the t�ipod positio� opti�izes the �e�ha�i�s of �espi�atio� �� taki�g adva�tage of the accessory muscles of the neck and upper chest to get more air into the lungs. Nasal fla�i�g? → Ca� i�di�ate �esp dist�ess, diffi�ult� ��eathi�g. Unable to complete a full sentence on a single breath? Cyanosis? Bluish discoloration of the skin, bc of low oxygen lvls in blood. Peripheral remains in hands and feet, whereas central cyanosis you see discoloration in the core, around lips and tongue. Can indicate a ventilatory prob leading to [poo� �lood o��ge�atio� i� the lu�gs → e� p�eu�o, PE, COPD. Clubbing? Lose normal angle of nail bed-to-finger. Clubbing can be seen with lung cancer, bronchiectasis as well as some indolent pulmonary infections. It can also be seen in a few extra-throracic conditions. Interstitial lung disease (restrictive). It is NOT seen in COPD*
Recommend
More recommend