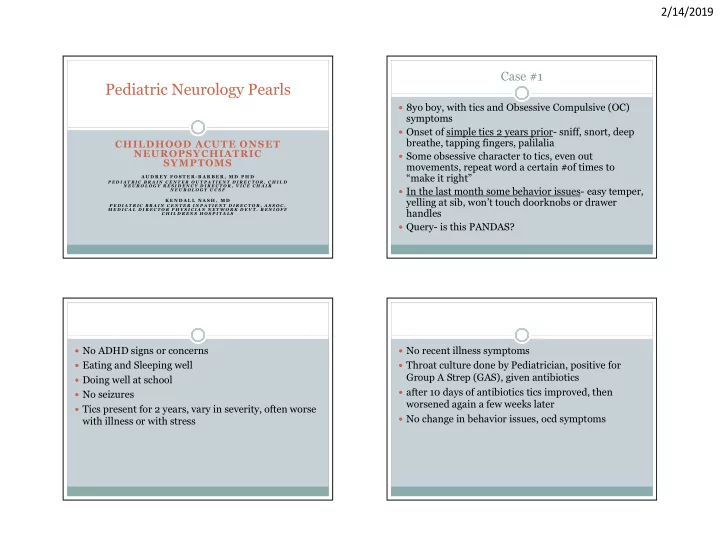
2/14/2019 Case #1 Pediatric Neurology Pearls 8yo boy, with tics and Obsessive Compulsive (OC) symptoms Onset of simple tics 2 years prior- sniff, snort, deep breathe, tapping fingers, palilalia CHILDHOOD ACUTE ONSET NEUROPSYCHIATRIC Some obsessive character to tics, even out SYMPTOMS movements, repeat word a certain #of times to “make it right” A U D R E Y F O S T E R - B A R B E R , M D P H D P E D I A T R I C B R A I N C E N T E R O U T P A T I E N T D I R E C T O R , C H I L D N E U R O L O G Y R E S I D E N C Y D I R E C T O R , V I C E C H A I R In the last month some behavior issues- easy temper, N E U R O L O G Y U C S F yelling at sib, won’t touch doorknobs or drawer K E N D A L L N A S H , M D P E D I A T R I C B R A I N C E N T E R I N P A T I E N T D I R E C T O R , A S S O C . M E D I C A L D I R E C T O R P H Y S I C I A N N E T W O R K D E V T . B E N I O F F handles C H I L D R E N S H O S P I T A L S Query- is this PANDAS? No ADHD signs or concerns No recent illness symptoms Eating and Sleeping well Throat culture done by Pediatrician, positive for Group A Strep (GAS), given antibiotics Doing well at school after 10 days of antibiotics tics improved, then No seizures worsened again a few weeks later Tics present for 2 years, vary in severity, often worse No change in behavior issues, ocd symptoms with illness or with stress 1
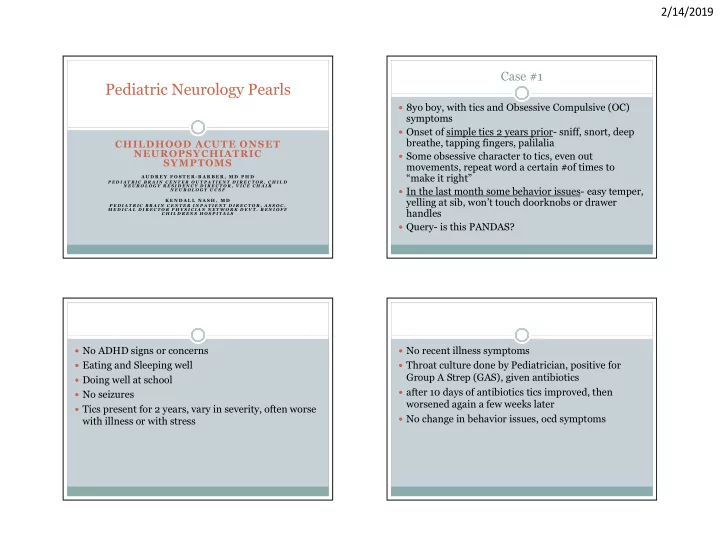
2/14/2019 PMH- born at term with duodenal atresia, largyngeal Return to clinic 6 months later with concern for cleft s/p repair “Explosive worsening” of behavior, moody, more OCD symptoms Development- normal milestones, bright child, aa bit anxious but social and active in sports Tics not worse, though a few new tics added to his repertoire FH- Mother with Hashimoto’s thyroiditis, history of anxiety, Father with history of a mood disorder No associated illness, primary doctor tested for Strep by throat culture and mycoplasma by antibodies, SH- lives with mother and sibling, parents divorcing both negative Dx-Tourette Syndrome or chronic tic disorder, OCD Did receive a Flu vaccine a few weeks to a month tendency prior 6 months later, ongoing CBT with some benefit for New stressors- mother with new partner moving in, behavior and OCD symptoms with partner’s child Tics still present, wax and wane Mother would prefer a PANDAS diagnosis, rather Seen by Integrative Medicine doctor- than a diagnosis of tic disorder with mood disorder Extensive Testing-zinc, heavy metal, strep culture, MTHFR “PANDAS seems to have a clear treatment, whereas polymorphism, autoimmune screen (ANA, DS-DNA) all the others would be a chronic disorder” negative -myocoplasma IgG+, Lyme Ab equivocal Recommend- cognitive behavioral therapy (CBT), no -Cunningham panel interpreted as abnormal antibiotics -treated with 3 months of Azithromycin, patient self d/c’d at 2 months due to GI distress 2
2/14/2019 Why did PANDAS come up here? Classic for Childhood Tic disorder - During the 2 months on antibiotics no tic worsening, -tics onset prepubertal, vary in type, wax and wane over time OCD was better already with therapy -associated OCD (up to 50 % of patients) Mother now “not so sure” about a PANDAS -bilineal inheritance (tics, adhd, anxiety, or ocd in both parents) diagnosis, but feels “antibiotics are benign” so will Family Concerns consider them if symptoms worsen (child refused -FH autoimmune disease antibiotic prophylaxis) -hope for something treatable Plans to avoid escalation to immune therapy that -difficulty of proving associated infection, of attributing was recommended- IVIg and or pheresis cause/effect of antibiotic therapy -common idea in the lay community, with integrative health Declined other neurologic work up (MRI and LP) providers because “doing too well” History behind PANDAS PANDAS- defined 1998 1980s- psychiatrists noted subset of patients with PANDAS- pediatric autoimmune neurologic disorder OCD who had a severe, abrupt onset of symptoms associated with Strep Temporal association with infectious triggers- strep, Presence of OCD and or tics- severe, interfere with varicella, mycoplasma, influenza, EBV, Lyme patient’s ability to function Initially called PITANDS - Pediatric infection Age of onset 3yo to puberty triggered autoimmune neurologic and psychiatric Acute onset, episodic (relapsing remitting) disorder Temporally related to GAS infection Researchers chose to focus on GAS infection due to Other associated neurologic (choreiform ease of documentation of infection and connection to movements) and behavioral abnormalities (sleep known molecular mimicry in Sydenham’s Chorea- disturbance, enuresis, anxiety, lability, insomnia) labeled PANDAS Swedo, SE. J Child and Adol Psychpharm, Feb 25(1)’ 2015 11 12 3
2/14/2019 Pediatric Acute onset Neuropsychiatric Defining a GAS infection is tricky Syndrome 25% of the pediatric population has + strep culture 2013 Consensus meeting without immune reaction ( carrier ) Back to the idea that multiple infections can trigger a ASO and DNAse B titers can remain elevated for months CNS response- PANS ( up to 12 mo in >50 % of kids s/p symptomatic infection ) Mechanism may be molecular mimicry as with Strep By age 12 years >98% of the population have positive titers (pseudo-autoimmune response- Ab to strep also reacts to neuronal antigens) PANDAS research dx requires flare associated with + culture and antibody evidence of appropriate rise in titer Assume also other inflammatory mechanisms over time, at least twice Primary focus on OCD symptoms, with other ( very rarely used clinically- diagnosis most often given with associated symptoms secondary- behaviors and single positive culture ) movements Blackburn, J. Seminars in Ped Neuro. 12: 2017 13 14 PANS PANS clinic experience 15 Research clinic, must fulfill research definition exactly 84% documented prior illness, only 17% Strep Abrupt, dramatic onset Behavioral regression of OCD or severe food Primary symptom OCD or eating d/o Deterioration in school restriction behavior Tics 26%, chorea 15% performance Concurrent neuropsychiatric Many with severe compulsions and mood issues, Sensory and motor symptoms : 2/7 1/3 with psychosis abnormalities-tics, Anxiety chorea Higher rate of maternal autoimmune disease, Emotional lability Somatic symptoms- strong FH of mood disorder Irritability, aggression, insomnia, enuresis oppositional Chang, K., Frankovich, J. 2015 Journal of Child and Adol Psychopharmacology, 25(1): 2015. 4
2/14/2019 Diagnostic Assessment for PANS Is the Cunningham panel helpful? Recommend full medical and family history, detailed Serum studies of autoantibodies neuro exam Sensitivity individual biomarkers for PANS dx Note mild hypotonia and chorea sometimes seen, no criteria 15-60% other specific serious neurologic signs or symptoms (no seizures, no delirium, no focal findings) Specificity 28-92% Strep test, other infectious titers, autoimmune labs PPV 17-40% Commercial antibody panel- Cunningham Panel , NPV 44-74% Moleculara Labs Majority of healthy controls had pathologic results -serum testing, Elisa -anti-dopamine receptor D1 and D2L Test-retest reliability poor -anti-lysoganglioside GM1 Does not document neuro-inflammation -anti-tubulin Hesselmark, E. J Neuroimmunol, Nov 15 (312): 2017. Treatments offered for PANS Do the Treatments for PANS work? Cognitive behavioral therapy Many published papers SSRI Systematic review of the literature on PANDAS, Antibiotics- for acute flare or daily for prevention PANS treatment over 17 years Steroids 3 large consensus papers- based on expert clinical NSAIDs experience, no research Plasma exchange One large survey of parents Intravenous Immune globulin 12 treatment studies- only 4 RCTs Rituximab 65 case series or case reports Cytoxan Total 1300 patients (90 in RCTs) Tonsillectomy, adenoidectomy -Sigra, S. Neurosci and Biobehav Rev. 86:2018. 5
Recommend
More recommend