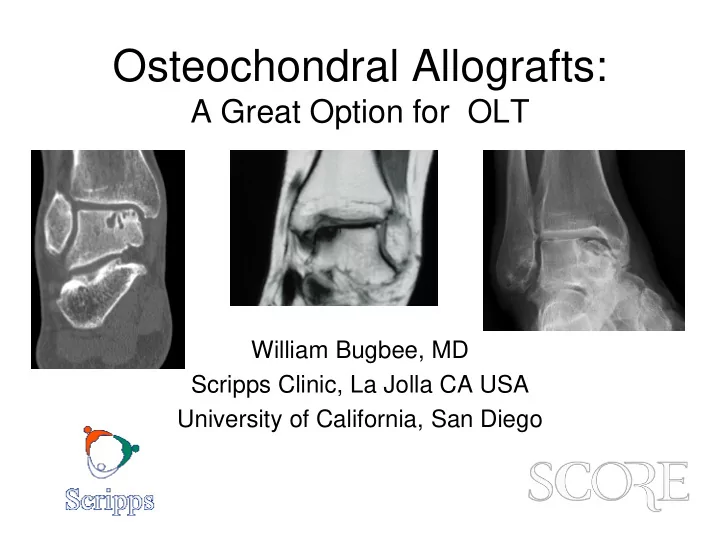
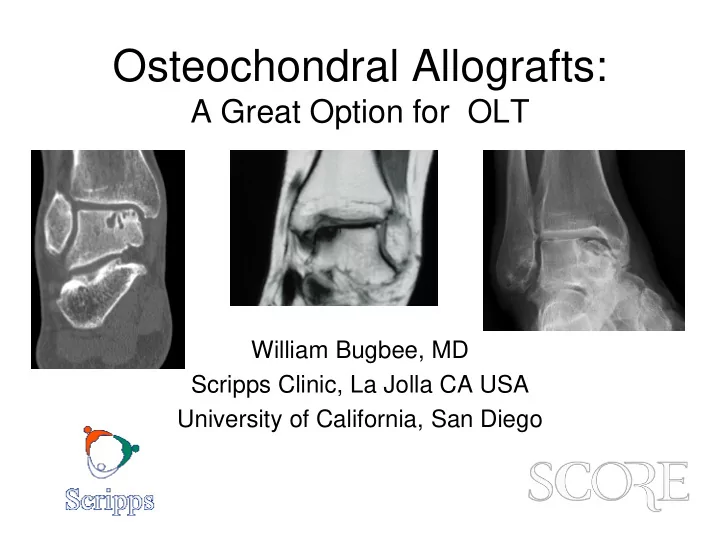
Osteochondral Allografts: A Great Option for OLT William Bugbee, MD Scripps Clinic, La Jolla CA USA University of California, San Diego
Disclosure • Joint Restoration Foundation – Consultant, research support • Arthrex – consultant • FDA – Medical advisory committee: Cellular, tissue and gene therapy
A shell allograft is not “bulky”
Subchondral Bone and the Osteochondral Unit • Integrated organ system • Very interdependent structure-function relationship
Osteochondral Replacement Has Many Advantages • Mature hyaline cartilage • No cell or tissue differentiation required • Bone healing paradigm • Replace diseased subchondral bone • Quick and simple rehabilitation
The Osteochondral Allograft Paradigm • Cartilage is an ideal tissue for transplantation • Transplantation of mature hyaline cartilage • Viable chondrocytes • Intact osteochondral unit • Bone healing vs. chondral tissue regeneration
When Do I Use Allografts in the Talus? • Osteochondral lesions (OLT) – Large volume cystic lesions (primary Rx) • Salvage of smaller lesions • Osteonecrosis • Traumatic defects • Selected cases of PTOA • Fresh talus allografts are relatively easy to obtain (in US)
Surgical Techniques • Approaches – Medial malleolar osteotomy – Lateral malleolar osteotomy – Anterior approach – External fixation joint distraction • The type of approach does not appear to affect clinical outcome • Consider morbidity of osteotomy
My Preference Görtz S, Bugbee WD. Oper Tech Orthop 2006, 16(4):244-249 . • Anterior approach • External fixation (optional) • Joint distraction • Modest plafondplasty • Onlay partial talus graft • Fixation with absorbable pins or darts or small metallic screws • 6-12 weeks non wt bearing
But Why Should You Consider Allografts in the Talus? Everyone that has used them and published results has a good experience! • 9 studies, 155 patients • Patient age 30-44 years • 2/3 medial lesions • Graft size 1.5-6.0 cm 2 6 yrs • Mean follow up 2-11 years Gross 2001, Raikin 2009, Hahn 2010, Gortz 2010, Janis 2010, Adams 2011, Berlet 2011, Daniels 2011, El-Rashidy 2011
Clinical Outcome Summary OCA for OLT • Patient satisfaction 75-100% • Improvement in ankle score (AOFAS) 27- 46 points – mean post op 79-83 • Complications and reoperations – 0-50% • 12 graft failures (8%) requiring revision, arthrodesis or arthroplasty
Recent Systematic Review • 5 studies, 91 patients • 39 years, 45 month mean f/u • AOFAS 40 80 • VAS 7.1 2.7 • 25% had reoperations • 13.2% failure • 8.8% converted to arthrodesis or TAA
My Long Term f/u • 20 patients • 34 years, 53% male • 11 medial, 9 lateral 81% 10 year Mean graft size 3.75 cm 2 (1.7-6.4) • survivorship • 9.7 year f/u (2-18) • 93% less pain and better function • 87% satisfied • 100% would have procedure again • 5/20 reoperation • 3 failures 8 years post-op
OCA for OLT is a Great Option
Thank You
Recommend
More recommend