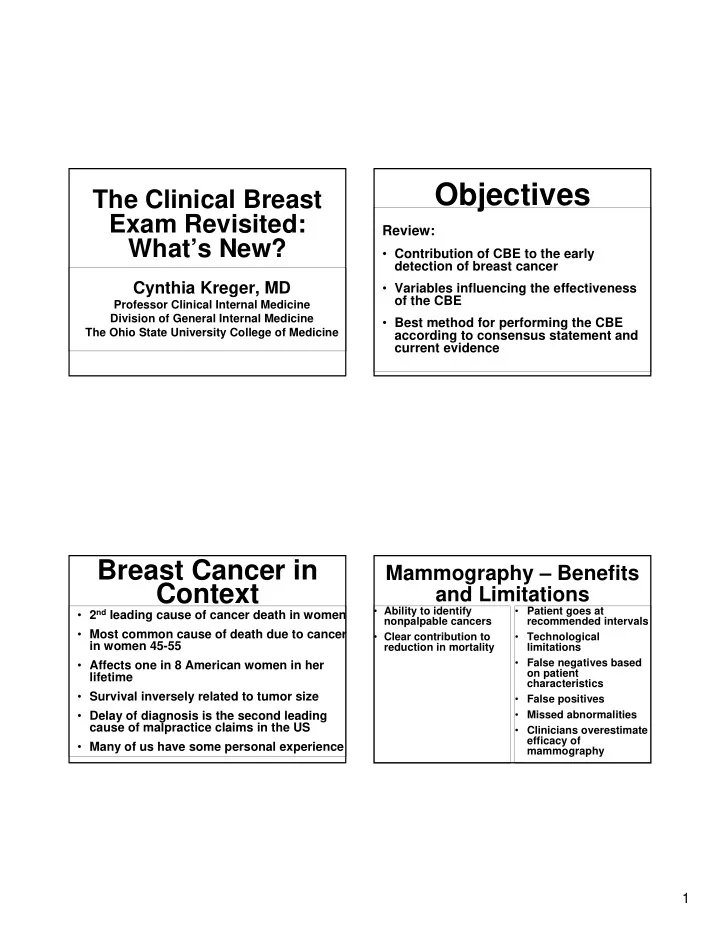
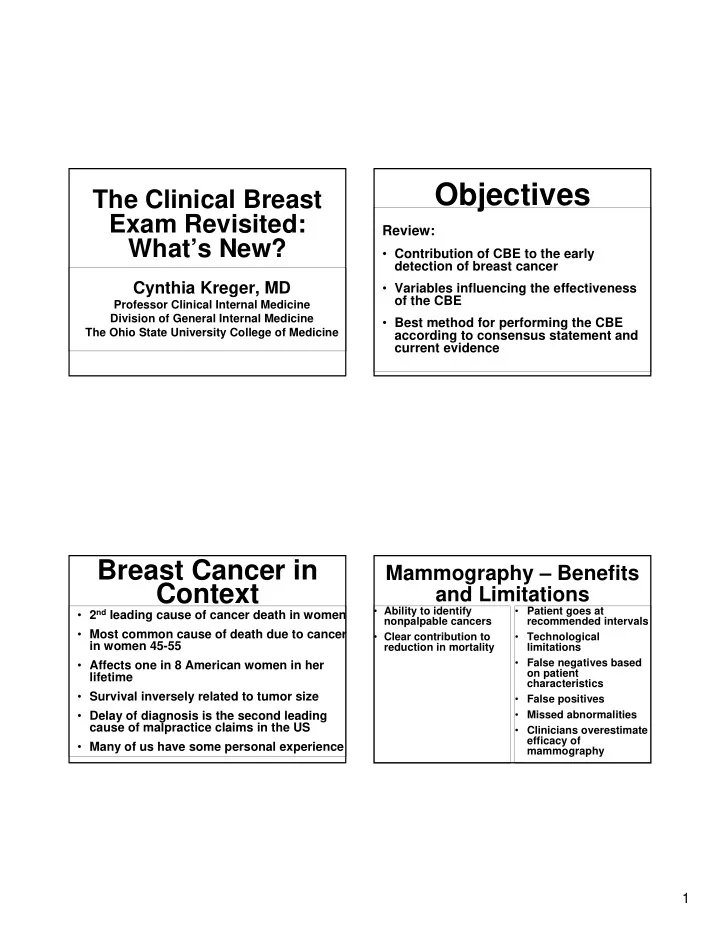
Objectives The Clinical Breast Exam Revisited: Review: What’s New? • Contribution of CBE to the early detection of breast cancer Cynthia Kreger, MD • Variables influencing the effectiveness of the CBE Professor Clinical Internal Medicine Division of General Internal Medicine • Best method for performing the CBE The Ohio State University College of Medicine according to consensus statement and current evidence Breast Cancer in Mammography – Benefits Context and Limitations • 2 nd leading cause of cancer death in women • Ability to identify • Patient goes at nonpalpable cancers recommended intervals • Most common cause of death due to cancer • Clear contribution to • Technological in women 45-55 reduction in mortality limitations • False negatives based • Affects one in 8 American women in her on patient lifetime characteristics • Survival inversely related to tumor size • False positives • Delay of diagnosis is the second leading • Missed abnormalities cause of malpractice claims in the US • Clinicians overestimate efficacy of • Many of us have some personal experience mammography 1
What is the Contribution of the What is the Goal of the CBE? CBE to Early Detection? Goal: • Lack of RCT demonstrating CBE • To detect palpable abnormalities in reduces mortality asymptomatic women at an earlier stage of • Population-based study: disease when treatment options are greater and more effective � 71.2% of cancers identified by BSE • To evaluate patient symptoms � 19.6% of cancers identified by mammogram • To provide screening in women for whom � 9.3% of cancers identified by CBE mammography is not recommended • Relied on recall, was in younger • To provide screening in limited resource women settings What is the Contribution of the What Are The Barriers To And Variables Influencing CBE? CBE to Early Detection? Physician Variables • More recent studies suggest that: � 5.1% of malignancies detected by CBE in women • Unconvinced about the value of the exam with negative, benign or probably benign • Discomfort with the exam mammograms • Confidence, skill • This is over 10,000 otherwise undetected cancers per year • Considerable variability in way the exam is taught � 10.7% of cancers identified by CBE alone and performed � CBE plays a role in detection of interval cancers, • Reliance on technology to provide the answer in screening for women under 40, and in women who do not receive high quality mammograms or • Limited time who do not follow recommendations for screening mammography • Experience in detecting abnormal breast lesions 2
What Are The Barriers To And CBE Skills Among Graduating Variables Influencing CBE? Primary Care Physicians • Only 50% examined the patient in a supine position with arm over head Patient characteristics • Only 55% performed systematic palpation � Tissue density, nodularity, menopausal status • Only 37% examined the supraclavicular Tumor characteristics region � Size, depth, mobility, firmness • Only 25% examined the axilla • Some evidence that CBE skills diminish during training The Components of the What’s Different Regarding Inspection? CBE Have Not Changed • Inspection • Inspection � No studies document the independent • Nodal Evaluation benefit of inspection � Taking into account limited time, inspect • Breast Palpation while palpating � Increase inspection if abnormality found on palpation 3
What’s Different What’s Different Regarding Regarding Inspection? Lymphatic Examination? • Inspection • Palpation of lymph nodes should: � Look for subtle changes such as • Include the supra and flattening of breast contour, area of infra clavicular areas fullness, asymmetry, difference in venous pattern, scaliness of skin • Include the apical, central, pectoral, and � Findings such as erythema, retraction or subscapular areas dimpling, or changes in the nipple such as inversion, tend to be late signs • Be performed with the patient seated What’s Different What’s Different Regarding Palpation? Regarding Palpation? • Emphasizes the following core competencies • MammaCare method � Positioning � Most widely studied � Perimeter � Palpation � Recommended by CDC and the ACS � Pressure � Pattern � Time 4
What’s Different Include the Full Perimeter During Palpation Regarding Positioning? The Cahan Position • Perimeter as pentagon Note two characteristics: • Sternum to the lateral chest wall at the • Position of patient’s mid-axillary line ipsilateral arm, the hand resting on forehead, • Clavicle to below the which softens pectoralis muscle infra-mammary ridge • Position of hips/knees to contralateral side, • Junction of the shoulder with the which helps to distribute breast tissue anterior chest, at anterior axillary line centrally over chest wall Performing the Performing the Examination Examination Palpation/Pressure Palpation/Pressure • Three fingers • Pay particular attention to upper outer quadrant, and under nipple • Dime-sized circles • No need to assess for nipple • Overlapping by one finger breath discharge � with fingers sliding over breast tissue • In women with breast implants - perform the CBE in the same way � helps to ensure no areas are missed • In women post mastectomy - palpate � palpate directly over nipple all of chest wall and along incision 5
What’s Different Performing the Examination Regarding Pattern? Time - A Critical Variable • Vertical strip pattern in contrast to concentric • Duration of exam (and consistency of search circles pattern) are the factors most consistently shown to correlate directly with sensitivity and • Palpate from distal to specificity proximal toward you � 1 minute increase in exam duration resulted in 1.8 more lumps being noted, but also increased false • Efficacy in detecting lumps positive rates • Vertical strip (67.9%) vs. spoke pattern (44.7%) � Optimal duration is influenced by a variety of factors: proficiency of examiner, breast size, lumpiness, body • Vertical strip (64.4%) vs. concentric circles weight, tenderness (38.9%) � A thorough exam may take up to 3-4 minutes per side What Can I Take Home? Video Demonstration Don’t overestimate the efficacy of mammography, don’t • underestimate the importance of CBE • Use the preferred method for CBE � Include infra and supraclavicular in lyamphatic At this point I would like to share evaluation a video clip that highlights � Consider the use of Cahan’s position selected portions of the exam. � Three level palpation, vertical strip pattern, cover full perimeter of breast tissue • Remember that time and consistency of search pattern are the most critical variables • Any abnormality found on CBE, even in the face of a normal mammogram, needs evaluation to appropriate resolution 6
Breast Cancer Palpable mass Screening usually ½” and Diagnosis Mammograms Adele Lipari, DO Assistant Professor of Radiology detect ¼” Ohio State University Medical Center Craniocaudad Lateral 7
Mammogram Paddles Adequate Mammograms Compression • Screening • Lowers x-ray dose • Diagnostic • Reduces thickness • Immobilizes breast • Spreads out tissue 8
ACR Recommendations for Screening Versus Sreening Mammogams Diagnostic Mammogram • Baseline between ages 35-40 • Screening • Annual screening mammograms after � No breast problems age 40 � No self history of breast cancer � Over age 40 Diagnostic Mammogram • Mass • Persistent, pin-point pain • Personal history of breast Ca • Increase in size/firmness • New nipple retraction • Itching/flackiness of nipple • Spontaneous nipple discharge- serous/bloody 9
Duty of Referring Doctor • Results of Clinical Exam • 10% of breast cancers are • Location of Palpable Lesion not seen by mammograms or ultrasounds • Recent Needle Biopsy Bi-Rads Code • Bi-Rads 1- Negative Ultrasound of • Bi-Rads 2- Benign findings • Bi-Rads 3- Short follow up the Breast • Bi-Rads 4- Suggestive of Ca • Bi-Rads 5- Strongly suggestive • Bi-Rads 6- Known Ca 10
Value of Breast US DMIST • Cysts • Margins/blood flow – solid mass • Digital mammographic screening trials • Lymph nodes • Study to determine value of MRI and • Duct evaluation digital mammography • Silicone implant leak • F/U known Ca • Perform aspiration/biopsy 11
Acrin Guidelines for Digital Mammograms Screening MRI • > 20% risk of Breast Ca • Detect 15-28% more Ca in premenopausal women or those • BRCA 1 and BRCA 2 gene mutation over 50 with dense breasts • 1 st degree relative with mutation • Strong family history • Chest radiation between 10-30 MRI in Contralateral Breast • 10% of breast ca patients develop contralateral Ca • DMIST showed a 3% increase in detection in ca patients 12
Image Guided Biopsy • Stereotactic biopsy Stereotactic • Ultrasound guided biopsy Breast Biopsy Stereotactic Table 13
Biopsy Clip Biopsy Needle Not Stereo Candidate • > 300 Pounds Ultrasound • Breast too small • Superficial lesion Guided • Deep lesion • Bleeding problems • Unable to lie prone 14
Complications of Ultrasound Biopsy Biopsy • Hematoma and Infection • Rate = 0.1% • Miss Rate = 3% 15
Recommend
More recommend