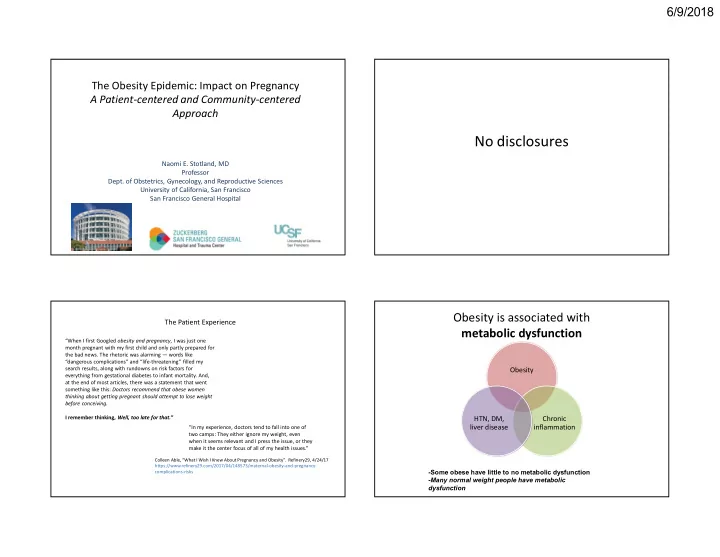
6/9/2018 The Obesity Epidemic: Impact on Pregnancy A Patient-centered and Community-centered Approach No disclosures Naomi E. Stotland, MD Professor Dept. of Obstetrics, Gynecology, and Reproductive Sciences University of California, San Francisco San Francisco General Hospital Obesity is associated with The Patient Experience metabolic dysfunction “When I first Googled obesity and pregnancy , I was just one month pregnant with my first child and only partly prepared for the bad news. The rhetoric was alarming — words like “dangerous complications” and “life-threatening” filled my search results, along with rundowns on risk factors for Obesity everything from gestational diabetes to infant mortality. And, at the end of most articles, there was a statement that went something like this: Doctors recommend that obese women thinking about getting pregnant should attempt to lose weight before conceiving. I remember thinking, Well, too late for that.” HTN, DM, Chronic liver disease inflammation “In my experience, doctors tend to fall into one of two camps: They either ignore my weight, even when it seems relevant and I press the issue, or they make it the center focus of all of my health issues.” Colleen Able, “What I Wish I Knew About Pregnancy and Obesity”. Refinery29, 4/24/17 https://www.refinery29.com/2017/04/148573/maternal-obesity-and-pregnancy- -Some obese have little to no metabolic dysfunction complications-risks -Many normal weight people have metabolic dysfunction 1
6/9/2018 Obesity and Stigma Obesity and Stigma • Weight bias = inequities in education, employment, • 68% of women with BMI > 55 reported delaying & healthcare healthcare because of their weight, and 83% reported that their weight was a barrier to getting • Widespread negative stereotypes: “lazy, care unmotivated, lacking discipline, not competent, non- • Women reported disrespectful treatment and compliant, sloppy” negative attitudes from providers, embarrassment • Implicit bias tests in providers shows strong about being weighed, and too small gowns, exam preference for thin tables, equipment • Obese persons are less likely to undergo recommended cancer screening Obesity and Stigma Stigma – Role of Providers “It’s interesting because we recently had someone who was • Language is important over 400 pounds who got transferred to us because her out-of- the-city hospital was too terrified of delivering her . They • In one study, patients preferred the term “weight” thought if she needed a C-section or whatever it would be impossible to do it and they just didn't want to deal with her . to “obesity” or “fat” • Focus on patients’ chosen behavioral and lifestyle So we induced her and it was just like passing the hot potato. No one wanted to be around. We induced her for days, we goals (rather than emphasizing weight measurement sent her home, we brought her back, we induced her some more. Because there’s a situation – you may not want to pull as only measure of success) the baby out but you do not want to do a C-section either.” • Avoid blaming and judgmental statements - Academic CNM, from focus group study 2
6/9/2018 Stigma – Role of Providers Intersection of Race and Obesity • It’s our duty as providers and hospitals to make birth as safe as possible for ALL patients • If we need different equipment, more providers/staff, we need push to get these resources rather than blame our patients for having particular needs • Because as a society we still blame individuals for having a high body weight, we may be less likely to fight for what is needed to keep our patients safe Monica Mclemore, PhD, MPH, RN Assistant Professor School of Nursing, UCSF “So what is successful in lowering risk and improving pregnancy outcomes? Years of data that show that successful public health interventions such as Black Infant Health, Nurse Family Partnership and Centering Pregnancy improve birth outcomes. … These programs are built on several principles, including culturally relevant care, peer-to-peer learning, and establishing cohorts among the women. “ https://www.centerforhealthjournalism.org/2018/02/18/what-blame-mother-stories-get-wrong-about-birth-outcomes-among- black-moms 3
6/9/2018 Early Pregnancy Concerns Early Pregnancy Concerns • Spontaneous abortion & recurrent • Cell-free fetal DNA screening may result in test failure or inaccurate result as obese women may loss more common have a lower fetal fraction of the cell-free DNA • Fetal anomalies, esp neural tube • First and second trimester serum-based screening tests are adjusted for maternal weight defects • Accurate NT measurement may be more difficult to • 20% decrease in detection of obtain anomalies by ultrasound Antepartum Complications Intrapartum Complications • GDM and DM2 • Prolonged labor (only first stage) • Lower likelihood of VBAC success • Chronic hypertension • Preeclampsia • Postterm pregnancy • Higher rates of cesarean delivery • Anesthetic complications • Macrosomia and shoulder dystocia • Stillbirth 4
6/9/2018 Postpartum Complications At first prenatal visit • Longer hospital stays • Screen for DM2 (repeat at 24 wks if neg) • Measure and record BMI in chart • Review weight gain goals and strategies with patient • Infections • Discuss MODIFIABLE risks especially re: weight gain – Wound infection and endometritis • If concern for CHTN: baseline Cr, 24hour urine, LFTs • Lower rates of breastfeeding The IOM Report and Guidelines IOM Recommendations for Weight Gain in Pregnancy 2009 Weight Gain During Pregnancy for Pre-pregnancy BMI IOM Recommended Obese Women (kg/m 2 ) Gestational Weight Gain (kg / lbs) <18.5 (Underweight) 12.5-18 / 28-40 18.5 – 24.9 (Normal) 11.5-16 / 25-35 25.0 - 29.9 (Overweight) 7-11.5 / 15-25 ≥30.0 (Obese) 5-9 / 11-20 5
6/9/2018 Does Prenatal Advice on Weight Gain Matter? • Receiving correct advice about weight gain was associated with actual weight gain within guidelines; • Receiving no advice about weight gain was associated with gain outside guidelines; • About a third of women report receiving no advice about how much weight to gain. Cogswell et al. Obstet Gynecol 1999. Stotland et al. Obstet Gynecol 2005. Comparison of weight gain by BMI category between PRAMS 2002-2003, and new IOM guidelines What interventions have been tested? Diet and Exercise Interventions • Overall, diet, exercise, and diet + exercise interventions in • Traditional diet, exercise, and diet + exercise pregnancy show a modest but significant effect on reducing GWG • However, many studies (esp in U.S.) show that these interventions • Digital Health are LESS effective among obese women • Meal replacement • The interventions studied are often not well-described and are heterogeneous from study to study, so difficult to interpret as a whole • Centering Pregnancy (secondary analysis) • Not surprisingly, more intensive (and expensive) interventions with more frequent human interaction seem to be more effective • Type of diet (eg low glycemic, low fat) seems to be less important than overall caloric restriction, similar to non-pregnant studies, but little is known about long-term impact on offspring • Digital Tools (apps) show promise and are widely accessible 6
6/9/2018 MEAL REPLACEMENT STUDY – Phelan et al The clinical impact was small but statistically significant, and especially impressive given that this intervention (Centering) was not specifically designed to prevent excessive weight gain. The effect was seen among all BMI groups including obese women. The effect persisted at 12 months postpartum 7
Recommend
More recommend