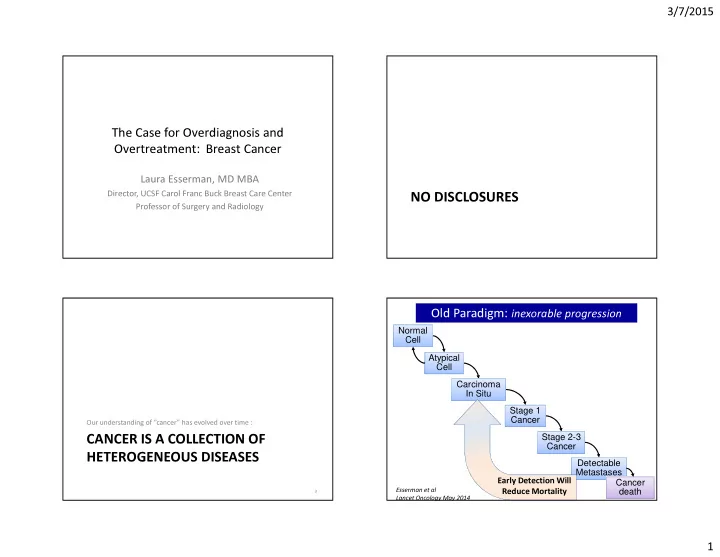
3/7/2015 The Case for Overdiagnosis and Overtreatment: Breast Cancer Laura Esserman, MD MBA Director, UCSF Carol Franc Buck Breast Care Center NO DISCLOSURES Professor of Surgery and Radiology Old Paradigm: inexorable progression Normal Cell Atypical Cell Carcinoma In Situ Stage 1 Cancer Our understanding of “cancer” has evolved over time : Stage 2-3 CANCER IS A COLLECTION OF Cancer HETEROGENEOUS DISEASES Detectable Metastases Cancer Early Detection Will death Esserman et al 3 Reduce Mortality Lancet Oncology May 2014 1
3/7/2015 New Paradigm: variable progression “Cancer” INDOLENT SLOW RAPID or REGRESS PROGRESSION PROGRESSION Dictionary.com Definition Normal Normal Normal Cell Cell Cell can·cer Atypical Atypical Stage 1-3 noun Cell/CIS Cell/CIS Cancer 1. Pathology Stage 1 Stage 1 Detectable a. a malignant and invasive growth or tumor, especially one Cancer Cancer Metastasis originating in epithelium, tending to recur after excision Cancer and to metastasize to other sites. Stage 2-3 death Cancer b. any disease characterized by such growths. IDLE tumors: Detectable Indolent lesions Metastasis of epithelial origin 2. any evil condition or thing that spreads destructively; blight. Cancer death Early Detection Will Early Detection Can Systemic Therapy Key 6 Not Impact Mortality Reduce Mortality to Reducing Mortality March 2012 • Workshop convened around overdiagnosis • Subgroup to compile recommendations to NCI – Signal the physician community – Signal the patient community – Generate shift in philosophy, enable improvement – Explain previous approach and motivate change • contentious debate � exploration of new concepts • Findings summarized PATIENTS ASSUME THAT CANCER, – JAMA 2013 LEFT UNTREATED, WILL KILL YOU – Lancet Oncology May 2014 Physicians too 7 8 2
3/7/2015 Recommendations to the NCI Recommendations Working Group 1. Recognize that over-diagnosis occurs and is common • Laura J. Esserman UCSF • 2. Embrace the development of new terminology to replace the Ian M Thompson UTHSC, San Antonio • Brian Reid, M.D., Ph.D. Fred Hutchinson CRC word “cancer” where appropriate; use companion diagnostics to • Peter Nelson, M.D. Fred Hutchinson CRC support this process • David F. Ransohoff, M.D. UNC, Chapel Hill • H. Gilbert Welch, M.D., M.P.H. Dartmouth • 3. Create observational registries for IDLE conditions with low or Shelley Hwang, M.D. Duke University • Donald A. Berry, Ph.D. UT MD Anderson Ca Ctr uncertain risk of progression to cancer • Kenneth W. Kinzler, Ph.D. Johns Hopkins University • William C BlackM.D. Dartmouth 4. Mitigate over-diagnosis by testing strategies that lower the • Howard Parnes NCI chance of detecting unimportant lesions • Mina Bissell LBL Berkeley • Sudhir Srivastava NCI, EDRN 5. Embrace new concepts for how to approach cancer progression and prevention 10 Esserman et al Lancet Oncology May 2014 Recommendation #1 Recommendation #1 RECOGNIZE THAT OVERDIAGNOSIS OVERDIAGNOSIS IS MORE OCCURS AND IS COMMON COMMON WITH SCREENING 11 12 3
3/7/2015 For Both Breast and Prostate Incidence Rates Have Risen and Remain Higher BREAST OVERDIAGNOSIS REPRESENTS OUR ABILITY TO DETECT THE ENTIRE PROSTATE SPECTRUM OF CANCERS THAT ARISE 14 Esserman et al JAMA 2009 Chance Increases with Screening Non-invasive Cancer • Lung: • Barrett’s Esophagus – Screening of general population increases incidence – Common with gastric reflux without changing mortality: Focus on HIGHEST RISK pts • 20% decrease in lung ca death – Considered high risk for esophageal cancer • Incidence of stage 1 CA >>reduction in stage 2-4 cancers • Nodules <1cm on CT: 1.5% chance of cancer – Barrett’s patients are screened with biopsy – Autopsy and screening: overdiagnosis 20-25% • Longitudinal studies • Thyroid – The vast majority will never develop Ca – In office screening of thyroid nodules has become routine – Barrett’s is an adaptation to reflux – SEER data : incidence has tripled, death rate constant 1975 2009 And yet, endoscopic screening continues . . . Incidence 4.9 14.3 Death rate 0.56 0.52 15 16 4
3/7/2015 an IDLE condition? IDLE CONDITIONS are part of the spectrum of breast cancer biology A TUMOR WITH LITTLE POTENTIAL FOR WHAT IS THE MAGNITUDE? METASTASIS AND NONE FOR DEATH Canadian RCT: 25 years of followup IDLE tumors Women 40-69, conducted during the Tamoxifen Era • Evidence suggests ultralow cancers exist With With Without Without – Pre-screening: 10-20% of all cancers Mammograms Mammograms Mammograms Mammograms – Post Screening Era: 25-50% of all cancers • Possibly up to 50% of non-palpable cancers (BMJ 2014) 44,925 women 44,910 women received • Based on trials, cohort studies received breast mammograms exams – A problem if not recognized and treated accordingly and breast exams 1 in 424 women • Opportunity to improve our approach to prevention were diagnosed with and treated for 3,250 women had 3133 women had and treatment cancers that would a diagnosis of a diagnosis of never come to breast cancer breast cancer • Opportunity to improve screening clinical attention – Learn who is at risk for what type of cancer 500 women died 505 women died – What should be a target for call back/biopsy? from breast from breast cancer cancer Miller et al BMJ Feb 2014 5
3/7/2015 IDLE tumors What Can Be Done? • Excess of 106 cancers/ • Invest in better biomarkers of extremely low • Estimate: 1/424 women screened metastatic potential • Recognize that non-palpable mammographically • 22% of all cancers detected breast cancers have a high chance of • 50% of non-palpable cancers being IDLE – AVOID OVERTREATMENT • Don’t overscreen Finding cancer at the earliest possible point- may not be optimal under all conditions – Minimize detection of IDLE conditions . . . – Don’t make low grade DCIS a target of early detection IF WE CANNOT RECOGNIZE AND TREAT ACCORDINGLY Defining “IDLE” Tumors 70 gene Prognosis Signature: “Ultra-low Threshold” 70 significant prognosis genes Ultralow Threshold Effect of screening on the detection of good and poor prognosis breast cancers Laura Esserman, Yiwey Shieh, Laura Van’t Veer Dan Moore, Emiel JT Rutgers, Michael Knauer,Valesca Retel, Stella van´t Veer et al., Nature ,2002 Mook, Sabine Linn, Flora E van Leeuwen, Annuska Glas Early Detection Research Network, 50% of screen detected tumors in MINDACT are Ultralow risk Drukker et al BCRT 2014 23 UCSF Dean’s Summer Research Fellowship 6
3/7/2015 Study Design Findings • Large database of 862 patients with known 70-gene • As age increases, the proportion of prognosis signature outcomes from previous European trials. – grade 1 tumors increases Selected node-negative cases only. – MammaPrint low (good risk) tumors increase • Cohort 1: Prior to screening era : pts diagnosed 1980- – Hormone receptor positive tumors increase 1991. No population-wide screening in countries of origin thus low uptake of mammography. • Distribution of good/poor risk tumors with screening – Does not shift in women under the age of 40 • Cohort 2: Screening era : pts diagnosed 2004-6 in 17 community-based hosptials (RASTER) in the Netherlands, • 25-30% good risk where screening uptake is approx 80%. – Substantially shifts in women aged 49-60 • subset of screen-detected cancers • Cohort 1: 40% good risk (no screening) • Cohort 2: 58% good risk (“screening”) •Analyzed 2 age groups separately: – 67% good risk in screen detected cancers • Age 49-60 : screened in cohort 2 but not cohort 1 (TEST) • <40 years : not screened in either cohort (CONTROL) Shieh Esserman, van’t Veer ASCO 2010 26 Esserman, Shieh, van’t Veer Br Ca Research and Treatment 2011 HR+HER2- ultra-low risk patients: Proportion of Node-Negative Patients Classified as Low Risk by RS and RSPC: Tamoxifen (TAM) vs. Untreated At least 50% Preliminary Results: Stockholm 1 Randomized Trial Low Risk Intermediate Risk High Risk STO trial long-term survival in Mammaprint Ultra-low risk by treatment arm 1 RS RSPC 0.9 Survival proportion 18.4% 19.1% 0.8 TAM 0.7 No TAM 54.2% 63.8% 17.8% Only 106 patients in total. Not significantly 26.7% 0.6 differential survival by treatment. P-log rank= 0.15 N=1444 0.5 0 5 10 15 20 25 Pathology-Clinical; RS, Recurrence Score Years since primary tumor diagnosis RSPC classifies fewer patients as having intermediate risk. X axis starts at 50% Ca Cancer Registry/ SEER: Lindstrom et al SABCS 2014 Women >50 with stage 1 N0 grade 1 comprise 50% of all breast cancer ore Tang G, et al. JCO. Oct 2011; 1-8. 7
Recommend
More recommend