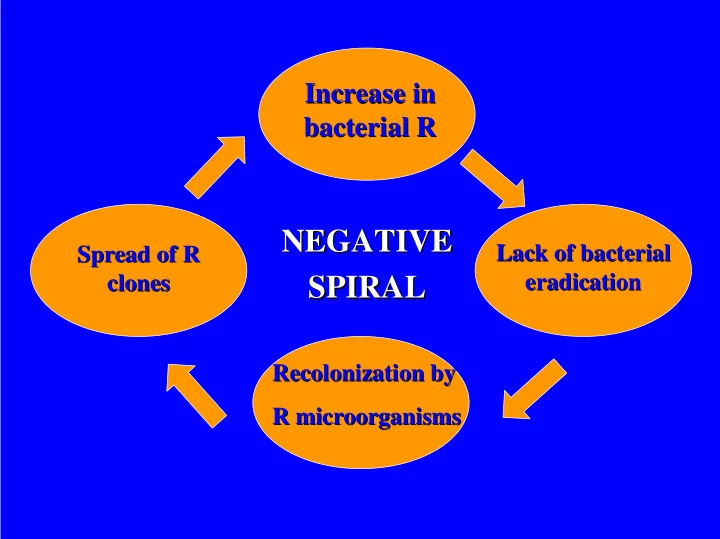
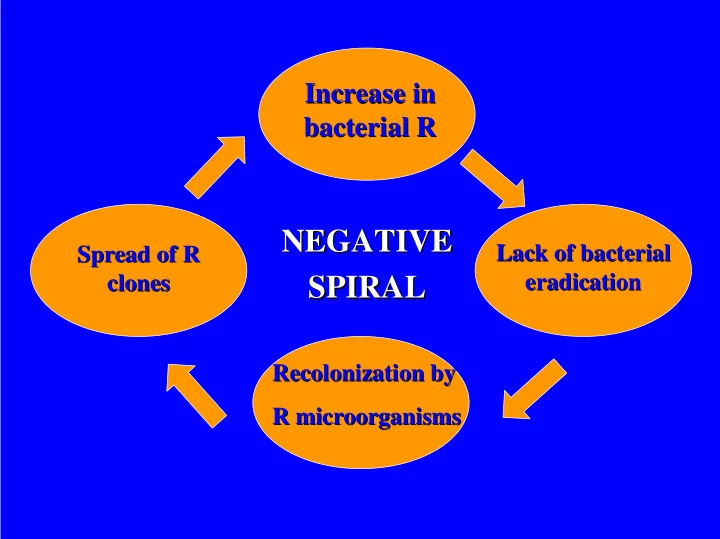
Increase in in Increase bacterial R R bacterial NEGATIVE NEGATIVE Lack of bacterial Spread of R R Lack of bacterial Spread of eradication clones eradication clones SPIRAL SPIRAL Recolonization by Recolonization by R microorganisms microorganisms R
Clinical relevance of in in vitro vitro data data Clinical relevance of Macrolides Macrolides • Which are the breakpoints in Europe? • Effect of methodology used • Effect of incubation atmosphere • Lack of reproducibility among labs. • Data for antimicrobial without published interpretative criteria • Differences in resistance mechanisms
Macrolides breakpoints proposed by Macrolides breakpoints proposed by different organizations for Streptococcus spp Streptococcus spp different organizations for Mensura NCCLS SFM BSAC S R S R S R S R ≤ ≤ ≤ ≤ 0.5 >2 ≤ 0.25 >1 ≤ ≤ ≤ ≤ ≤ ≤ 1 >8 ≤ ≤ ≤ ≤ ≤ 0.5 >1 Erythromycin ≤ ≤ ≤ ≤ 0.5 >2 ≤ ≤ 0.25 >1 ≤ ≤ ≤ ≤ ≤ 1 >8 ≤ ≤ ≤ ≤ ≤ 0.5 >1 Clarithromycin ≤ ≤ ≤ ≤ 0.5 >2 ≤ ≤ 0.25 >2 ≤ ≤ ≤ ≤ ≤ ≤ 1 >8 ≤ ≤ ≤ ≤ 1 >2 Azithromycin Modified from Perea E. Int J Antimicrob Agents. 2001
% of agreement ( ± ± ± 1 dilution) among ± different susceptibility methods CO 2 /Ambient E/BD E/AD AD/BD S. pneumoniae Erythromycin 58% 75% 65% Azithromycin 0% 0% 9% H. influenzae Erythromycin 65% 75% 70% Azithromycin 33% 42% 42% E: e-test; AD: agar dilution; BD: broth dilution Bolstrom et al. ICAAC. 1996
How should resistance limit the use of macrolides (evidence-based?) • Streptococcus pneumoniae • Streptococcus pyogenes • Haemophilus influenzae • Campylobacter spp • Others?
Antibiotic resistance in Streptococcus pneumoniae Isolates non susc. to erythromycin (%) 70 60 50 40 30 20 10 0 0 20 40 60 80 Isolates non susceptible to penicillin (%) Cornaglia et al. ESGARS
Outpatient antibiotic sales in 1997 in the in 1997 in the Outpatient antibiotic sales E.U. E.U. 7 / δαψ / δαψ / δαψ ινηαβιταντσ / δαψ 6 ινηαβιταντσ ∆∆∆ / 1,000 ινηαβιταντσ ινηαβιταντσ 5 4 Macrolides - lincos. ∆∆∆ / 1,000 ∆∆∆ / 1,000 ∆∆∆ / 1,000 3 2 1 0 France Portugal Luxembourg Greece Ireland Austria Sweden Netherlands (Cars et al., 2001)
Macrolide resistance in in S. S. pneumoniae pneumoniae Macrolide resistance Phenotype distribution distribution Phenotype Country MLS B ( ermAM ) M ( mef E ) Spain 1 98.4% 1-3% USA 2 <25% >75% 1 Baquero F et al. Antimicrob Agents Chemother. 1999 2 Sutcliffe J et al. Antimicrob Agents Chemother 1996. Whitney et al. NEJM 2000
Macrolides and S. pneumoniae Lack of correlation in vitro/in vivo • Different mechanism of resistance • Relation between mechanism of R and bacterial eradication • Redefinition of susceptibility and resistance: – Moving breakpoints to reflect 2 mechanisms – Use of a surrogate such as clindamycin
Characterization of 302 erythromycin-R S. pneumoniae isolates Clindamycin MICs Erythromycin MIC Strains 0.25 0.5 1 2 8 1 15 15 0 0 0 0 2 52 51 0 0 0 1 4 53 53 0 0 0 0 8 68 68 0 0 0 0 16 23 22 1 0 0 0 32 6 5 0 0 0 1 64 85 0 0 1 1 83 Doern et al. Emerging Infect Dis. 1999
Pneumococcal macrolide resistance: myth or reality? • Provide the clinicians MIC data • Compare MICs with in vivo pharmacokinetics and pharmocodinamics • Provide MICs of different macrolides (erythromycin and azalides) • Review MIC breakpoints according to site of infection • New clinical breakpoints for intravenous formulations. Amsdem GW. J Antimicrob Chemother. 1999
no data available < 5% 5 - 15% 16-25% ESGARS > 25% Incidence of macrolide resistance in S.pyogenes (G.Cornaglia and P.Huovinen, 12th ECCMID, Berlin, 1999)
Macrolide resistance in in S. S. pyogenes pyogenes . . Macrolide resistance Clinical significance significance?: No ?: No Clinical • Macrolide treatment of pharyngitis accounts for a low proportion of the overall use • Pharyngitis by S. pyogenes is a mild, self limiting disease • The prevalent phenotypes are endowed with low resistance level (M) versus high tissue concentration • C16 macrolides and ketolides may still be effective.
Macrolide resistance in in S. S. pyogenes pyogenes . . Macrolide resistance Clinical significance significance?: ?: Yes Yes Clinical • Increase in severe infections: necrotising fasciitis, STSS • Role of low level resistance • Role of C16 macrolides and ketolides. • In vitro susceptibility and outcome of infection • Spread of macrolide resistance to other species ( S. pneumoniae, S. viridans )
Otitis media caused by caused by H. H. Otitis media influenzae influenzae • Bacterial failure with azithromycin: 71% (similar to placebo). Dagan et al. K102. ICAAC 1997 • New infections by H. influenzae : 15%. Dagan et al. Antimicrob Agents Chemother. 2000 . • Bacterial eradication: 33% azithromycin vs 87% amox/Clav. Craig et al. Ped Infect Dis J. 1996
Macrolide R in Campylobacter spp from human origin Country C. jejuni C. coli Both Austria 0.7 5.5 <1-1.4 Mutation at 23S Denmark 0 14.0 0-4 rRNA Finland - - <1-3 France 1.1 12.2 3.5 Almost 100% Hungary - - 0 MLSB Italy 1.2-6 16-68.4 7.8-11.6 phenotype Spain 0-11 0-35 3.2-7.3 Sweden 6.4 11.1 7.3 U.K. 1 13 1.8 Engberg et al. Emerging Infect Dis. 2001
Recommend
More recommend