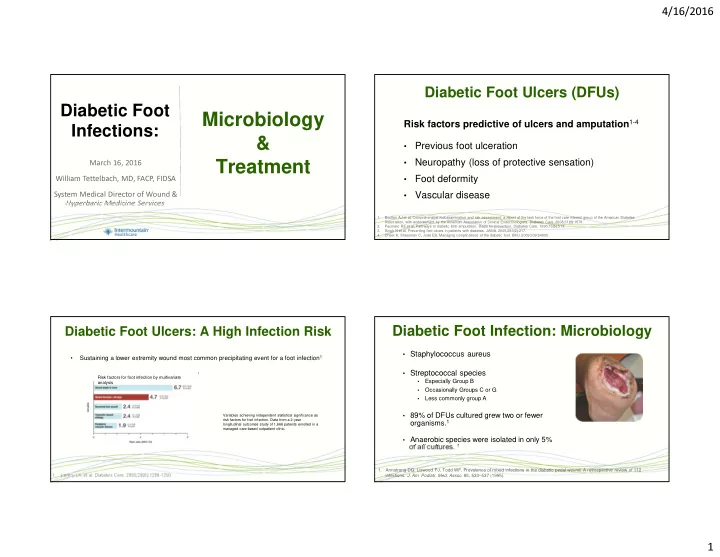
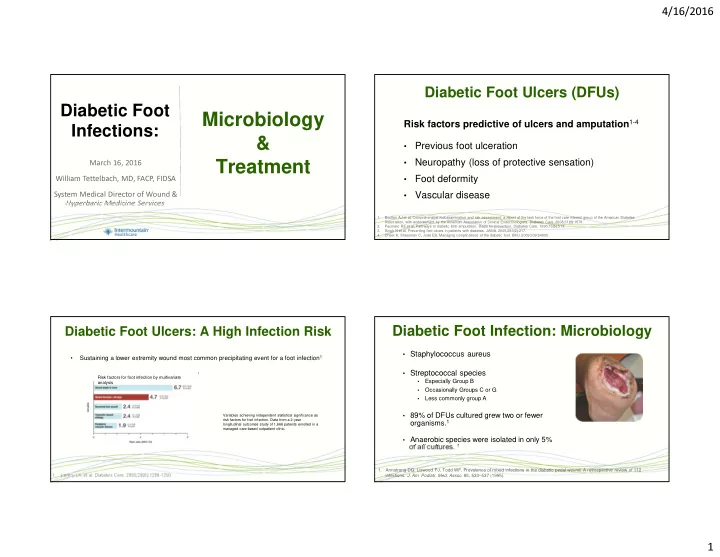
4/16/2016 Diabetic Foot Ulcers (DFUs) Diabetic Foot Microbiology Risk factors predictive of ulcers and amputation 1-4 Infections: & Previous foot ulceration • Treatment Neuropathy (loss of protective sensation) • March 16, 2016 Foot deformity • William Tettelbach, MD, FACP, FIDSA Vascular disease • System Medical Director of Wound & Hyperbaric Medicine Services 1. Boulton AJ et al, Comprehensive foot examination and risk assessment: a report of the task force of the foot care interest group of the American Diabetes Association, with endorsement by the American Association of Clinical Endocrinologists. Diabetes Care. 2008;31(8):1679. 2. Pecoraro RE et al, Pathways to diabetic limb amputation. Basis for prevention. Diabetes Care. 1990;13(5):513. 3. Singh N et al, Preventing foot ulcers in patients with diabetes. JAMA. 2005;293(2):217. 4. Cheer K, Shearman C, Jude EB, Managing complications of the diabetic foot. BMJ. 2009;339:b4905. Diabetic Foot Infection: Microbiology Diabetic Foot Ulcers: A High Infection Risk • Staphylococcus aureus Sustaining a lower extremity wound most common precipitating event for a foot infection 1 • • Streptococcal species 1 Risk factors for foot infection by multivariate Especially Group B • analysis analysis Occasionally Groups C or G • Less commonly group A • • 89% of DFUs cultured grew two or fewer Variables achieving independent statistical significance as risk factors for foot infection. Data from a 2-year organisms. 1 longitudinal outcomes study of 1,666 patients enrolled in a managed care-based outpatient clinic. • Anaerobic species were isolated in only 5% of all cultures. 1 1. Armstrong DG, Liswood PJ, Todd WF. Prevalence of mixed infections in the diabetic pedal wound. A retrospective review of 112 infections. J. Am. Podiatr. Med. Assoc. 85, 533–537 (1995). 1. Lavery LA, et al. Diabetes Care. 2006;29(6):1288-1293. 1
4/16/2016 Diabetic Foot Infection: Microbiology Diabetic Foot Osteomyelitis: Microbiology Gram Positive Aerobes • Chronic or more severely infected DFUs tend to be more polymicrobial • Staphylococcus aureus • most common pathogen cultured from bone 1 • Common Gram Negative Pathogens • Staphylococcus epidermidis E. coli • Klebsiella spp. • Gram Negative Aerobes Anaerobes Proteus spp. • • Escherichia coli • Peptostreptococcus spp. • Pseudomonas aeruginosa • Peptococcus spp. • Klebsiella pneumoniae Associated with water exposure • • Proteus species • Finegoldia magna e.g., Puncture wound thru bottom of a shoe • • Pseudomonas aeruginosa • B. fragilis 1. Senneville E, Melliez H, Beltrand E, et al. Culture of percutaneous bone biopsy specimens for diagnosis of diabetic foot osteomyelitis: concordance with ulcer swab cultures. Clin Infect Dis 2006; 42:57–62. Diabetic Foot Infection: Osteomyelitis Diabetic Foot Infection: Osteomyelitis • Plain film rarely useful (unless late in course) Probing to bone in infected pedal ulcers is a clinical sign of • underlying osteomyelitis in diabetic patients 1 good for foreign bodies • sensitivity of 66% • • Bone scan nonspecific specificity of 85% • positive predictive value of 89% • Especially in patients with neuropathic osteoarthropathy (Charcot joint) • negative predictive value of 56% • Can be useful when MRI is not an option • If you can palpate small bones of the feet in diabetics with a • • MRI (gold standard for radiological diagnosis) chronic ulcer, consider it osteomyelitis until proven otherwise • T1 weighted image (low signal intensity) • T2 fat-saturated image (hyperintense signal) • T1 fat-saturated image post-gadolinium (enhancement) 1. Grayson ML, JAMA 1995;273:721-723 z • 2
4/16/2016 Limb Preservation Treatment Network Diabetic Foot Infections: Treatment Vascular Evaluation • Nutrition Optimization • Address Comorbidities • Debridement • Culture Wounds • Advanced Wound Dressings • Offloading TeleHealth • Appropriate Use of Antimicrobials • Diabetic Foot Infections: Treatment Diabetic Foot Infections: Treatment Oral antibiotic agents for empiric therapy of mild diabetic foot infections. Inpatient vs. Outpatient Drug Renal Dosing Required? Class Unable To Dicloxacillin No Penicillin • Critical Ischemic Limb • Unable To Care For Themselves † Amoxicillin/Clavulanate Yes β -lactam/ β -lactamase inhibitor • Systemic Toxicity † Cephalexin Yes Cephalosporin • Metabolic Instability Cefdinir Yes Cephalosporin † Levofloxacin Yes Fluoroquinolone • Necrotizing Soft Tissue Infection † ‡ Clindamycin No Lincosamide • Substantial Necrosis / Gangrene § TMP/SMX Yes Sulfonamide § • Need for Urgent Diagnostic / Therapeutic Intervention Minocycline Yes Tetracycline § Doxycycline No Tetracycline †Drugs that have been used in published trials of treatment of diabetic foot infections. ‡Suspect inducible clindamycin resistance if staphylococcal isolate is susceptible to clindamycin but resistant to erythromycin. Confirm with D-test. §Active against community-associated methicillin-resistant Staphylococcus aureus . TMP/SMX: Trimethoprim/sulfamethoxazole 3
4/16/2016 Diabetic Foot Infections: Treatment Parenteral or oral antibiotics for empiric therapy of moderate-to-severe DFU infections Drug Class Activity against Activity against Renal Dosing MRSA? B. fragilis? Required? Antibiotic Selection Overview: Questions a Clinician Should Consider. Ampicillin/Sulbactam β -lactam/ β -lactamase inhibitor No Yes Yes Is there clinical evidence of infection or critical colonization? Piperacillin/tazobactam β -lactam/ β -lactamase inhibitor No Yes Yes Do not treat clinically uninfected wounds with antibiotics. Ceftriaxone Cephalosporin No No No Is there high risk of MRSA? Cefepime or Ceftazidime Cephalosporin No No Yes Ceftaroline Cephalosporin Yes No Yes Include anti-MRSA therapy in empiric regimen if the risk is high or the infection is severe. Ertapenem Carbapenem No Yes Yes Has patient received antibiotics in the past month? Imipenem/cilastatin Carbapenem No Yes Yes If so, include agents active against gram-negative bacilli in regimen. Moxifloxacin Quinolone No Yes No If not, agents targeted against just aerobic gram-positive cocci may be sufficient. Clindamycin with Ciprofloxacin Lincosamide / Quinolone Some Yes No Are there risk factors for Pseudomonas infection? a Tigecycline Glycylcycline Yes Yes No Vancomycin Glycopeptide Yes No Yes If so, consider empiric antipseudomonal agent. Linezolid Oxazolidinone Yes No No If not, empiric antipseudomonal treatment is rarely needed. Daptomycin Cyclic lipopeptide Yes No Yes a. Such as high local prevalence of Pseudomonas infection, warm climate, frequent exposure of the foot to water. Diabetic Foot Infections: Treatment Diabetic Foot Infections: Treatment 1 Algorithm for the use of HBO 2 Duration and route of antibiotic therapy for the treatment of diabetic foot osteomyelitis. 2 Clinical situation Route of therapy Duration of therapy Wagner Grading System: A. Grade 1: Superficial Diabetic Ulcer No residual infected tissue Parenteral or oral 2–5 days B. Grade 2: Ulcer with deep structures involved: (e.g., postamputation) • ligament, tendon, joint capsule or fascia no active infection (abscess or osteomyelitis) Residual infected soft tissue Parenteral or oral 2–4 weeks • (but not bone) C. Grade 3: Ulcer with deep structures involved: Residual infected (but viable) Initial parenteral, then consider 4–6 weeks • ligament, tendon, joint capsule or fascia + evidence of infection (abscess or osteomyelitis) • bone oral switch D. Grade 4: Gangrene to portion of forefoot No surgery, or residual dead Initial parenteral, then consider >3 months bone postoperatively oral switch E. Grade 5: Extensive gangrene of foot Lipsky B, Berendt A, Deery H et al. Infectious Disease Society of America. Guidelines for the diagnosis and treatment of diabetic foot 1. 1. Huang ET et al; UHMS CPG Oversight Committee. A clinical practice guideline for the use of hyperbaric oxygen therapy infections. Clin. Infect. Dis. 39, 885–910 (2004). in the treatment of diabetic foot ulcers. Undersea Hyperb Med. 2015 May-Jun;42(3):205-47. 2. Wagner FW, The diabetic foot. Orthopedics. 1987 Jan;10(1):163-72. 4
4/16/2016 Diabetic Foot Infections: Treatment Diabetic Foot Infections: Treatment • “Appropriate therapy” includes: • o HBO 2 as adjunctive therapy • Antibiotics • Offloading • • at least 42 days for osteomyelitis • total contact cast • antibiotics should be culture-directed • walker boot Treat at 2.0 to 2.4 ATA once or twice daily • PICC line for outpatient management • • Aggressive surgical debridement Oxygen administered 90 to 120 minutes per session • • remove infected/dead bone, as well as involved hardware if possible Treatment range: 30 to 40 • Educate & optimize dietary needs • • e.g., malnutrition (protein), vitamin D, Vitamin C, Vitamin A, Zinc may require up to 60 treatments to achieve sustained • • Address comorbidities therapeutic benefit • e.g., diabetes, venous stasis, smoking cessation, renal/liver failure • Vascular evaluation/intervention if indicated • Adjunct HBO 2 therapy (not an approved indication for acute osteomyelitis) Questions? 5
Recommend
More recommend