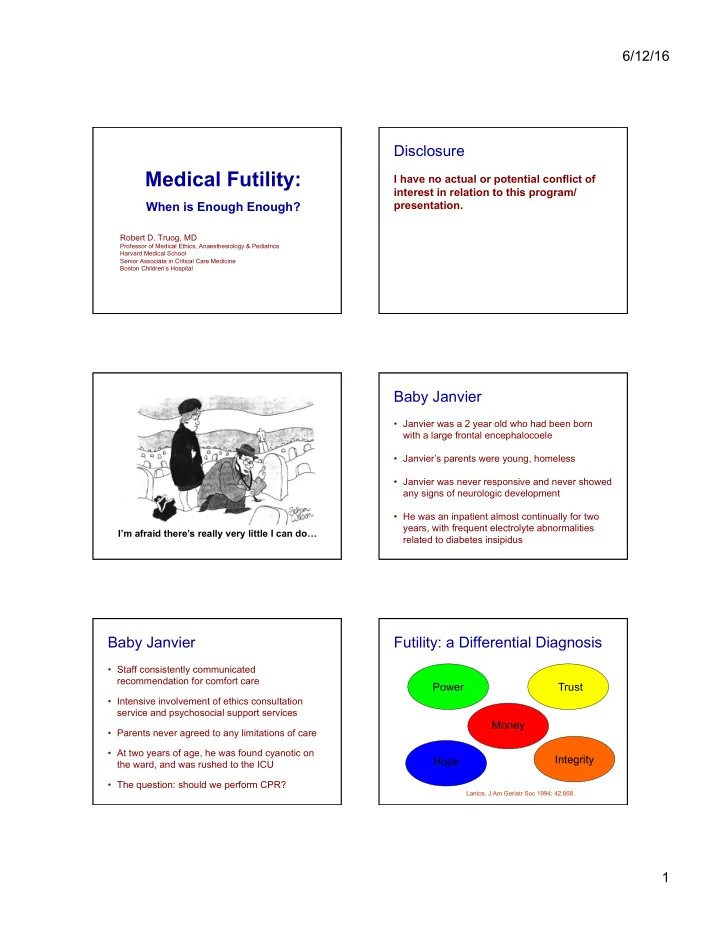
6/12/16 Disclosure Medical Futility: I have no actual or potential conflict of interest in relation to this program/ When is Enough Enough? presentation. Robert D. Truog, MD Professor of Medical Ethics, Anaesthesiology & Pediatrics Harvard Medical School Senior Associate in Critical Care Medicine Boston Children’s Hospital Baby Janvier • Janvier was a 2 year old who had been born with a large frontal encephalocoele I ’ m afraid there ’ s very little I can do • Janvier’s parents were young, homeless • Janvier was never responsive and never showed any signs of neurologic development • He was an inpatient almost continually for two years, with frequent electrolyte abnormalities I’m afraid there’s really very little I can do … related to diabetes insipidus Baby Janvier Futility: a Differential Diagnosis • Staff consistently communicated recommendation for comfort care Power Trust • Intensive involvement of ethics consultation service and psychosocial support services Money • Parents never agreed to any limitations of care • At two years of age, he was found cyanotic on Integrity Hope the ward, and was rushed to the ICU • The question: should we perform CPR? Lantos. J Am Geriatr Soc 1994; 42:868. 1
6/12/16 What’s underneath the futility Who gets to say NO? debate? • Power • The question of the 1970’s & 1980’s: The rights of patients to refuse medical • Trust treatment – Ethically and legally resolved, but still a problem in practice • Money • Hope • The question of the 1990’s and 2000’s: The rights of patients to demand • Integrity medical treatment – Ethically, legally, and politically controversial How should we frame the A debate about “ Odds and Ends ” issues? • Do patients and families have a right to force • Questions about futility doctors to squander scarce time and ask: resources on therapies that have no benefit in order to satisfy their irrational wishes? – What chance or probability of success is “ worth it ” ? • Do doctors have a right to arbitrarily ignore – What quality of the values and preferences of patients and outcome is “ worth it ” ? families, using only their own value systems to make life and death decisions for others? Lantos. J Am Geriatr Soc 1994; 42:868. Caplan. Ann Intern Med 1996; 125:688. What’s underneath the futility A debate about “ Odds and Ends ” debate? • Are these questions within the expertise of • Power the medical profession? • Trust • Money • Hope • Integrity Good Lord, Gilroy, it’s not for us to determine if they’re worth saving! 2
6/12/16 Get better data about the loss of Surrogates vs Physicians trust • 72% of surrogates think that patients have a right to demand care their physicians think will not help. – Only 44% of physicians agreed • 21% of surrogates think that even when doctors think there is “ no hope of recovery, ” all efforts should continue indefinitely. – Only 2.5% of physicians agreed Lenworth et al. Archives Surgery 2008: 143:730 Is it all just a question of What’s underneath the futility debate? money? • Power Futility debates • Trust rarely arise around therapies that are • Money cheap and easy to provide • Hope • Integrity Would futility guidelines save Would futility guidelines save money? money? “ Resource consumption and the extent of “ The low frequency of futility in an adult futile care among patients in a pediatric intensive care unit setting. ” intensive care unit setting. ” Halevy et al. Arch Int Med 1996; 156:100-4. Sachdeva et al. J Pediatr 1996; 128:742-7. “ The frequency of futile interventions appears to be low “ Despite our use of broad definitions of medical futility, unless one is willing to accept a definition that includes relatively small amounts of resources were used in futile patients who could survive for many months... this PICU care... attempts to reduce resource consumption in suggests that concepts of futility will not play a major role the PICU by focusing on medical futility are unlikely to be in cost containment. ” successful. ” 3
6/12/16 What’s underneath the futility Hope debate? • Power • The issue of “ miracles ” • Trust • Money • Insights from “ lotteries ” • Hope • Is hope just a denial of the facts? • Integrity Hope Hope is a state of mind independent of the state of the world. If your heart’s full of hope, you can be persistent when you can’t be optimistic. You can keep the faith, despite the evidence, knowing that only in so doing does the evidence have any Hope has nothing to do with probabilities chance of changing. So, while I’m not optimistic, I’m always very hopeful. Eric Cassell, MD Reverend William Sloane Coffin, as interviewed on NPR radio in 1994 Hope If the talk ended here … • Since futility judgments – • “ High Hopes ” Abigail Zuger, JAMA 1989;262:2988 – Are often a power-play by clinicians to enforce their values on power-less patients and families • “ Which was, in fact, the greater cruelty? Was – Are used as a trump card when trust has broken it the one she avoided, which would have down in the patient-physician relationship condemned Jerry to a protracted death in the intensive care unit, all blood and tubes and – Can squash whatever therapeutic value there may pain? Or was it the one she committed, sitting be in hope, however irrational it may seem on Jerry’s bed, holding his hand, and – Will save very little money under even the most methodically erasing all the hope from his optimistic of circumstances … eager eyes? ” 4
6/12/16 Futility judgments should have no role in Rise and Fall of limiting treatments for Futility patients and families who want them Helft et al. N Engl J Med 2000; 343:293. What’s underneath the futility Integrity debate? • Power • In some cases, clinicians experience moral distress from the belief that their efforts to • Trust keep patients alive are profoundly wrong. • Money • “ Moral distress is psychological disequilibrium that occurs when the ethically right course of • Hope action is known but cannot be acted on. ” • Integrity Meltzer et al. Am.J.Crit.Care 2004; 13:202. Integrity Resolution? – “ I often equate my job with ‘ keeping dead people alive. ’ On these days, I dread coming Is there a way to identify reasonable limits to work. ” to what patients and families can demand, – “ I’m scared that I’m causing while adequately respecting different undue pain and suffering, and values and perspectives? this causes me great distress. ” – “ Some days I feel (physically) sick. ” Elpern et al. Am.J.Crit.Care 2005; 14:523 5
6/12/16 Justice Stewart on Attempts to define “ Futility ” Pornography • When physicians conclude (either through personal "I shall not today experience, experiences shared with colleagues, or attempt further to consideration of published empiric data) that in the define... pornography; last 100 cases a medical treatment has been useless, and perhaps I could they should regard that treatment as futile never succeed in intelligibly doing so. • If a treatment merely preserves permanent unconsciousness or cannot end dependence on But I know it when I see intensive medical care, the treatment should be it..." considered futile Schneiderman et al. Ann.Intern.Med. 1990; 112:949. The Failure to Define Futility • This insight lies behind the movement to develop procedural rather that definitional approaches to determining futility. • “Judgments of futility cannot be made by reference to rules or definitions, but must be determined on a case by case basis.” American Medical Association Plows et al. JAMA 1999; 281:937. Beyond Hospital Policy … Texas Advance Directives Act • Some states are now adopting futility legislation • The physician’s refusal to treat must be reviewed by a hospital ethics committee. • These laws follow the procedural approach that has been developing in hospitals • The family must be given 48 hours notice and be • Most of the experience so far has been in Texas invited to participate in the process. • The hospital must make reasonable efforts to transfer the patient’s care to others. 6
Recommend
More recommend