Managing Sleep Disorders Disclosures and Depression in Patients No - PDF document
6/25/2018 Managing Sleep Disorders Disclosures and Depression in Patients No conflicts of interest to report with Liver Disease ECHO Program Presentation, June 25, 2018 Richard Yanofsky, MD, FRCPC Lecturer, University of Toronto
6/25/2018 Managing Sleep Disorders Disclosures and Depression in Patients • No conflicts of interest to report with Liver Disease ECHO Program Presentation, June 25, 2018 Richard Yanofsky, MD, FRCPC Lecturer, University of Toronto University Health Network, Centre for Metal Health Psychiatrist, Francis Family Liver Clinic richard.yanofsky@uhn.ca Why have this talk? Why have this talk? • High comorbidity of depression in patients with chronic liver disease • Prevalence rates of Sleep-Wake disturbances are amongst highest of chronic medical conditions • Linked prognostically with severity of liver disease • Early indicator of covert hepatic encephalopathy • Vulnerable population for medication induced adverse reactions • Associated with critical comorbidities • Concerns related to drug induced liver injury for certain psychotropic • Under-diagnoses and poorly managed medications • Liver disease interferes with drug metabolism at multiple • Contributes greatly to risk, morbidity and QOL pharmacokinetic stages Learning Objectives Two topics • Review major considerations for treatment of depression in patients • Depression with liver disease • Pharmacokinetics • Drug-induced liver injury • Develop a better understanding of the nature of Sleep-Wake • Monitoring disturbances in Cirrhotic Patients • Sleep-wake disturbances • Increase comfort with the diagnosis and management of these • Insomnia common complaints • Hypersomnolence • Sleep associated disturbed behaviours 1
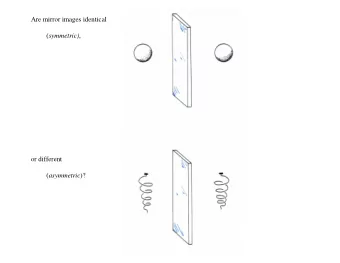
6/25/2018 Depression in CLD Depression in CLD – Pharmacokinetics • Comorbidity is higher than expected, even compared to other Distribution chronic medical conditions (40%) • Intra and extra (and therapeutic) shunts and decreased first-pass • Severity of depression is correlated to severity of liver disease metabolism • Depression severity impacts CLD outcomes • Less drug passes through the liver before systemic distribution • Antidepressants are effective treatments for depression in CLD • Elevation in drug concentrations in the blood patients • His effect is particularly important for drugs with extensive first-pass metabolism Depression in CLD – Pharmacokinetics Depression in CLD – Pharmacokinetics Protein Binding • Most psychotropic medications are highly protein bound • Higher concentration of free, active drug when liver is cirrhotic • Particularly important for highly protein-bound drugs, such as benzodiazepines • Venlafaxine, lithium, topiramate, gabapentin, pregabalin, methylphenidate are minimally protein bound (Telles-Correia et al, 2017) Depression in CLD – Pharmacokinetics Depression in CLD – DILI • 0.5%-3% of patients treated with antidepressants may develop Metabolism • Lithium, gabapentin and topiramate are the only psychotropic medications asymptomatic mild elevation of serum aminotransferase levels that are excreted in the urine unchanged • All antidepressants may be hepatotoxicit, and liver damage in most • Phase I cytochrome P-450 enzymes can be significantly impaired in cirrhosis cases is unpredictable and unrelated to drug dosage and required for conversion of most psychotropics into inactive form • The interval between treatment initiation and onset of liver injury is • Phase I enzymes are occasionally required to convert prodrug to active metabolite (certain TCAs, and notably risperidone) generally between several days and 6 months • Phase II conjugation with glucuronic acid is normally preserved even in • Life-threatening antidepressant-induced liver injury has been severe cirrhosis described involving fulminant liver failure or death • Temazepam, oxazepam, or lorazepam do not undergo phase I metabolism • Hepatocellular type hepatoxicity is more common than cholestatic and are preferred to diazepam and other benzodiazepines for this reason and mixed types 2
6/25/2018 Depression in CLD – DILI Depression in CLD – Monitoring • Greater risks of hepatotoxicity are iproniazid, nefazodone, • Baseline history and physical, plus LFTs before starting any psychotropic medication in a patient with CLD phenelzine, imipramine, amitriptyline, duloxetine, bupropion, • Non-pharmacological treatment options (which can be highly effective but trazodone, tianeptine, and agomelatine often challenging to access and complete in patients with CLD) • Lower potential for hepatotoxicity are citalopram, escitalopram, • There is no unanimous agreement regarding the frequency of analysis re- paroxetine, and fluvoxamine assessment • Cross-toxicity has been described, mainly for tricyclic and tetracyclic • Laboratory tests with ALT > 3ULN or ALP > 2ULN are considered sensitive markers for liver damage, and in these cases, the psychotropic agent should antidepressants be stopped • Patients should be counselled to report signs and symptoms of liver (Voican et al 2014) dysfunction Physiological Sleep Regulation Physiological Sleep Regulation Homeostatic ‘Sleep Pressure’ Circadian Rhythm Time Awake Sleep Awakening 7 7 onset Time of Day 3
6/25/2018 Physiological Sleep Regulation Physiological Sleep Regulation Sex hormone regulation Melatonin Pleiotropism (Inhibits Prolactin, LH, FSH) Mediates blood pressure Mitochondrial through vasoconstriction ETC effects and dilation Poorly Regulates skin understood pigmentation in immune response to modulating sunlight role Inhibits pancreatic B-cell Phasing of insulin secretion circadian Anti-inflammatory and pacemaker antioxidant effects Disturbance of Sleep Regulation Disturbance of Sleep Regulation ‘Melatonin Model’ ‘Melatonin Model’ Disturbance of Sleep Regulation Disturbance of Sleep Regulation ‘Pressure Deficit Model’ ‘Melatonin Model’ 4
6/25/2018 Pathophysiology of Disturbance Sleep architecture Decompensate Cirrhosis Cirrhosis + HE d Cirrhosis Sleep attributes of cirrhotic patients Sleep architecture disruption in cirrhosis Sleep attributes of cirrhotic patients Approach to management • Sleep History • Comorbidity workup • Sleep Journal • Standardized rating scales • Behavioural treatments • Pharmacological management 5
6/25/2018 Approach to managment Approach to managment • Sleep History • Sleep History • Onset, frequency, duration, severity • Comorbidity workup • Sleep patterns, environment, psychosoical stressors • Rule out HE • Reports from bed partner • Pain, pruritus, nocturia, ascites • Nicotine, caffeine, alcohol use disorders • Depression, anxiety • Obstructive sleep apnea (OSA) • Restless leg syndrome (RLS) Approach to managment STOP BANG • Sleep History • Routine screening suggested for • Comorbidity workup patients with insomnia • Sleep Journal • 2/4 “STOP” or 3/8 “STOP BANG” = 70% specificity for OSA • Total sleep duration, sleep schedule, time to sleep onset, number of • Triage patients for awakenings, daytime nap, medications polysomnographyh • 2 week duration of recording • Diagnostic and therapeutic value Approach to management • Sleep History • Comorbidity workup • Sleep Journal • Standardized rating scales • Pittsburgh Sleep Quality Index • Athens Insomnia Scale • Berlin Questionnaire • Epworth Sleepiness Scale • Restless Legs Sleep Questionnaire 6
6/25/2018 Approach to managment Sleep Hygeine • Sleep History • Sleep only when sleepy • Comorbidity workup • If you cannot fall asleep within 20 minutes, get up and do something boring until you feel sleepy • Sleep Journal • Maintain a regular sleep-wake schedule even on • Standardized rating scales weekends • Behavioural treatments • Do regular exercise at least 4 hours before bedtime • Sleep hygiene • Develop sleep rituals to cue your body for sleep • CBT for insomnia (CBT-i) • Only use your bed for sleep and intimacy Sleep Hygiene • Stay away from caffeine-containing food, beverages, and medications, nicotine and alcohol for at least 4-6 hours before bedtime • Nap only as recommended or necessary • Have a light snack and glass of milk before bed • Take a hot bath before bed • Make sure your bed and room are quiet and comfortable, a cooler room is recommended CBT-i CBT-i • Sleep Efficiency = (Total Sleep Time / Time In Bed) • Time In Bed (TIB) is restricted to increas Sleep Efficiency (SE) • Increase or decrease TIB weekly by only 20-30 min • Increase TIB if SE >90% • Decrease TIB if SE <80% • Other domains include relaxation training, sleep environment improvement, stimulus control • Delivered weekly for 5-12 weeks • Online free, paid, app, 1:1, group 7
6/25/2018 CBT-i Progressive muscle relaxation • Most effective evidence based treatment for insomnia (period!) • More effective than treatment with hypnotic alone • CBT-i alone = CBT-i + hypnotic • No trials in cirrhosis • Compliance, capacity, motivation issues Guided meditation Approach to management • Sleep History • Comorbidity workup • Sleep Journal • Standardized rating scales • Behavioural treatments • Pharmacological management • Hydroxyzine • Lactulose • Modafinil • Melatonin • Stimulants • Z-drugs • Antidepressants Pharmacological management Z-Drugs Ideal Hypnotic in cirrhosis: • Negligible hepatic metabolism • Short half-life • No active metabolites • Limited lipophilia 8
Recommend
More recommend
Explore More Topics
Stay informed with curated content and fresh updates.