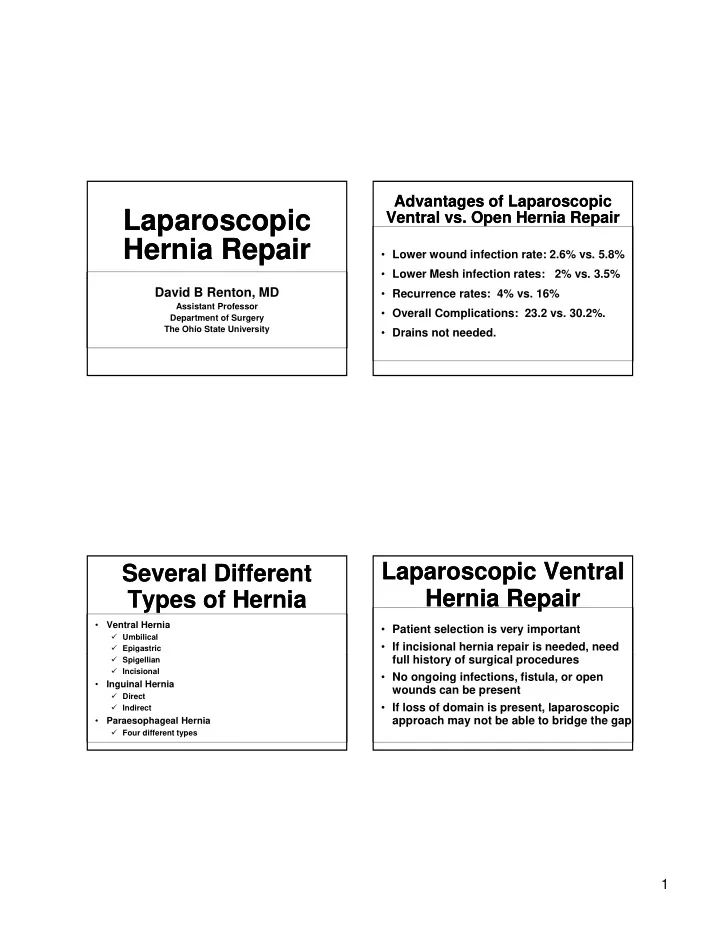
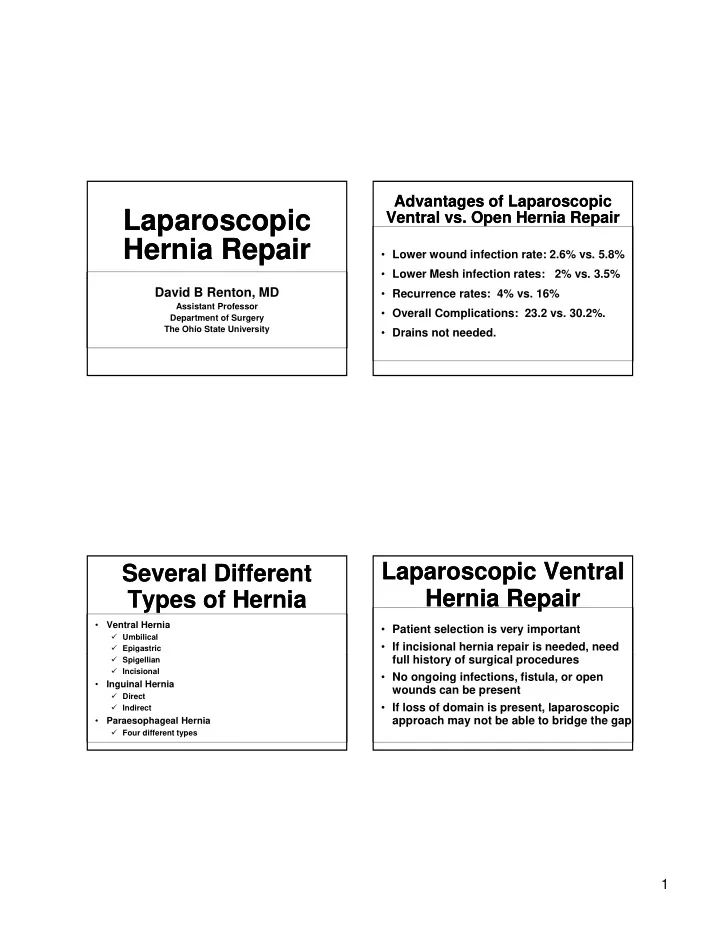
Advantages of Laparoscopic Advantages of Laparoscopic Laparoscopic Laparoscopic Ventral vs. Open Hernia Repair Ventral vs. Open Hernia Repair Hernia Repair Hernia Repair • Lower wound infection rate: 2.6% vs. 5.8% • Lower Mesh infection rates: 2% vs. 3.5% David B Renton, MD • Recurrence rates: 4% vs. 16% Assistant Professor • Overall Complications: 23.2 vs. 30.2%. Department of Surgery The Ohio State University • Drains not needed. Laparoscopic Ventral Laparoscopic Ventral Several Different Several Different Hernia Repair Hernia Repair Types of Hernia Types of Hernia • Ventral Hernia • Patient selection is very important � Umbilical • If incisional hernia repair is needed, need � Epigastric full history of surgical procedures � Spigellian � Incisional • No ongoing infections, fistula, or open • Inguinal Hernia wounds can be present � Direct � Indirect • If loss of domain is present, laparoscopic approach may not be able to bridge the gap • Paraesophageal Hernia � Four different types 1
Laparoscopic Inguinal Laparoscopic Inguinal Trocar Placement for Laparoscopic Trocar Placement for Laparoscopic Hernia Repair Hernia Repair Incisional Hernia Repair Incisional Hernia Repair Author Type of Number Follow-up Complicat Hernia repair of period ion recurrence patients rate (%) rate (%) Rutledge McVay 906 9 years NR 2.0 Amid Lichtenstein 3,250 Average of 4 NR 1.5 years (range: 1 to 8 years Rutkow and Rutkow 2060 NR 0.3 0.1 Robbins Nyhus Posterior 1200 37 years NR 1-6 Iliopubic tract repair Felix Transabdominal 733 24 months 13 0.3 preperitoneal laparoscopic repair TAPP Felix Total 382 Average of 9 11 0.3 extraperitoneal months laparoscopic repair TEP Trocar Placement Trocar Placement 2
Inguinal Hernias Inguinal Hernias Paraesophageal Hernia Paraesophageal Hernia Type I (sliding hernia) • Upward migration of GE • junction into posterior mediastinum Represent 90% of PEHs R t 90% f PEH • Found in greater than 10% • patients on routine GI studies Prevalent during third to fifth • decades Often associated with • symptoms of GERD Inguinal Hernias Inguinal Hernias Paraesophageal Hernia Paraesophageal Hernia • Type II (rolling) • Upward displacement of gastric fundus with normal positioned GE junction • Less than 2% of all HHs • Common symptoms include postprandial fullness/pain, nausea, dysphagia and heartburn • Can present with anemia and pulmonary dysfunction less commonly 3
Paraesophageal Hernia Paraesophageal Hernia Type III (mixed) • About 5% of all HHs • Combines type I and type II • Symptoms similar to type II • M Most prevalent in fifth to t l t i fifth t • sixth decade Most commonly on left • side of diaphragm Divided into Type 3A • (natural) and Type 3B (postoperative/iatrogenic) Type IV contains • omentum/colon Laparoscopic Hernia Laparoscopic Hernia Paraesophageal Hernia Paraesophageal Hernia Repair Repair • Lots of different types of hernias • Many can be fixed using laparoscopic • Many can be fixed using laparoscopic techniques • Patient selection is important • Surgical wisdom comes in knowing when not to operate 4
Ventral Hernia Repair Principles Ventral Hernia Repair Principles Abdominal Wall Abdominal Wall Reconstruction Reconstruction • Incorporation of the remaining abdominal wall in the repair p A.V.Manilchuk M.D. • Tension-free Assistant Professor • Dynamic muscular support Department of Surgery The Ohio State University Muscle and Investing Fascia Muscle and Investing Fascia Abdominal Wall Reconstruction Abdominal Wall Reconstruction • Autologous tissue rearrangement • Prosthetic or bioprosthetic materials • Structural anatomy should be integrated with understanding the dynamic function of the abdominal wall. 5
Treatment Options Treatment Options Mesh Mesh • Nonabsorbable: • Primary Repair Polypropylene / Polyester / PTFE • Mesh • Bioprosthetic p • “Components Separation” with and without “C S • Anchor mesh to well vascularized tissue mesh • Complications: • Local flaps and Free tissue transfer � Seroma, Infection, fistula formation, • Staged repair erosion, & continued drainage Primary Repair Primary Repair Mesh Placement Mesh Placement • Patient selection • Limited to small defect Limited to small defect • Highest recurrence rate • Tension leads to ischemia and failure 6
Intraperitoneal Intraperitoneal Onlay Technique Onlay Technique Underlay Placement Underlay Placement • Still most popular • Milliken survey : 1/2 of surgeons use this • Open and laparoscopic. repair without closing the fascial defect. • Large overlap allows for better tissue • Large overlap allows for better tissue • The disadvantages: ingrowth � Wide tissue undermining predisposes to wound complications • Different Fixation techniques � The pressure required to disrupt the • Recurrence 5% mesh from the anterior abdominal wall is less than other repairs Open Intraperitoneal Open Intraperitoneal Inlay Technique Inlay Technique Underlay Underlay • Provides for a tension-free repair at the time of surgery • No undermining of the onlay repair • Intra-abdominal pressure - tension to the mesh-fascial interface, which is the weakest point of the repair 7
Retrorectus, Retrorectus, Components Separation Components Separation Retroperitoneal Underlay Retroperitoneal Underlay • Oscar Ramirez (1990) : � Cadaveric dissection • Rives and Stoppa � Incision 1cm lateral to linea semilunaris • Mesh - above the posterior rectus sheath and � Ext oblique (easily separated from � Ext oblique (easily separated from beneath the rectus muscle beneath the rect s m scle internal oblique in avascular plane • Overlap between the mesh and fascia � Rectus flap can be advanced • Distribution of pressure over a wider area (Pascal's principle), • 5cm epigastrium • Pressure-induced apposition promotes ingrowth • 8-10cm middle • Physiologic repair • 3cm suprapubic Rives-Stoppa Repair Rives-Stoppa Repair Open Components Separation Open Components Separation 8
Open Component Open Component Minimally Invasive Minimally Invasive Separation Separation Component Separation Component Separation • Rectus Abdominis Perforators Preservation Significantly Reduces Wound • Rectus muscle medialization - restores Complications dy a dynamic abdominal wall function c abdo a a u ct o • Cosmetic improvement -excision of excess tissue • Drawback – large flap dissection with devascularization When laparoscopic approach When laparoscopic approach When laparoscopic When laparoscopic is not an option is not an option approach is not an option approach is not an option enterocutaneous fistulas 9
When laparoscopic When laparoscopic When laparoscopic approach is not an option When laparoscopic approach is not an option approach is not an option approach is not an option enterocutaneous fistulas When laparoscopic approach is not an option When laparoscopic approach is not an option When laparoscopic approach is not an option When laparoscopic approach is not an option enterocutaneous fistulas 10
When laparoscopic approach is not an option When laparoscopic approach is not an option 11
Recommend
More recommend