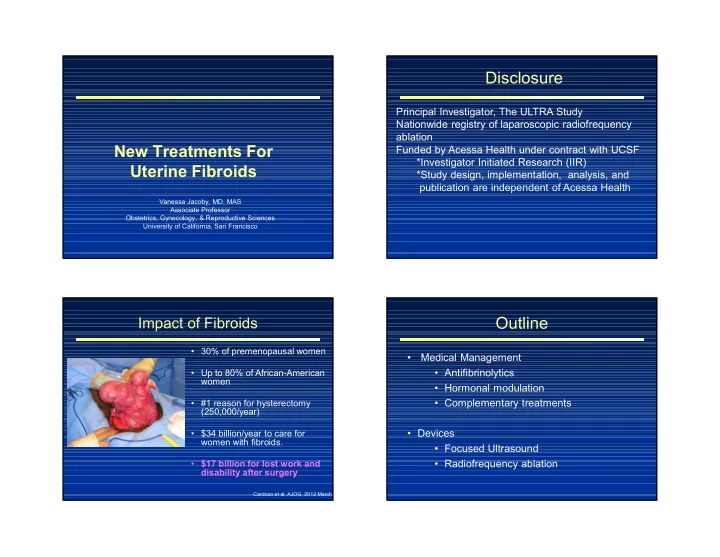
Disclosure Principal Investigator, The ULTRA Study Nationwide registry of laparoscopic radiofrequency ablation New Treatments For Funded by Acessa Health under contract with UCSF *Investigator Initiated Research (IIR) Uterine Fibroids *Study design, implementation, analysis, and publication are independent of Acessa Health Vanessa Jacoby, MD, MAS Associate Professor Obstetrics, Gynecology, & Reproductive Sciences University of California, San Francisco Outline Impact of Fibroids • 30% of premenopausal women • Medical Management • Antifibrinolytics • Up to 80% of African-American women • Hormonal modulation • Complementary treatments • #1 reason for hysterectomy (250,000/year) • Devices • $34 billion/year to care for women with fibroids. • Focused Ultrasound • Radiofrequency ablation • $17 billion for lost work and disability after surgery Cardozo et al, AJOG, 2012 March
Antifibrinolytic: Tranexamic Acid Tranexamic Acid: Pivotal RCT • Nonhormonal medication for heavy menses • Binds to plasmin to inhibit fibrinolysis N=297 2% decrease 26% decrease 39% decrease Freeman et al, AJOG, 2011, pg 319. e1-7 Tranexamic Acid RCTs: Tranexamic Acid: Limitations Subgroup with Fibroids in Two Pivotal Trials With fibroids, N=147 • Unknown fibroid size, number, location in subgroup • Excluded if MD thought fibroids better for surgery 44% decrease • Potential thrombotic risk (VTE) • Not observed in meta-analysis (n=1,400) • Women on OCP and others with VTE risk Without fibroids, N=224 have been excluded 36% decrease Freeman et al, AJOG, 2011, pg 319. e1-7 Eder et al, Women’s Health, 2013
Medical Management: Selective Progesterone Receptor Hormonal Manipulation Modulators (SPRM) • Agonist and Antiagonist effect at PR binding site • Decrease fibroid volume • Induce apoptosis, suppress vascularization, reduce Progesterone Estrogen collagen deposition • Reduce bleeding • Endometrial changes, suppress ovulation (but not estrogen levels), amenorrhea New Drug Targets : Selective hormone modulation Selective Progesterone Receptor Ulipristal (PEARL I and II) Modulators (SPRM) Ulipristal Acetate: • European trials (85-90% white participants) decreased bleeding, improved QOL • Placebo vs. Ulipristal (n=242) • Lupron vs. Ulipristal (n=307) • Participants with heavy bleeding, anemia, uterus <16 weeks (largest fibroid <10cm) • Received13 weeks of medication prior to surgery Donnez et al, NEJM, 2012: 366:421-32.
Ulipristal Trials: PEARL I and II Ulipristal (VENUS I) Ulipristal vs. Placebo Ulipristal vs. Lupron • US Trial, 25 sites U 5mg Placebo U 5mg Lupron (68% African-American/black participants) N=95 N=48 N=93 N=93 PBAC<75 • Placebo vs. 5mg vs. 10mg (n=157) (normal) 91% 19%* 75% 80% • Participants with heavy bleeding, Amenorrhea 73% 6%* 90% 89% uterus <20 weeks (largest fibroid <10cm) Change in -21% +3%* -36% -53% fibroid • Received12 weeks of medication volume Moderate to 11% 40%* severe hot flashes * p<.05 compared with 5mg Donnez et al, NEJM, 2012 Simon et al, Obstet Gynecol, March 2018 Ulipristal Trials: VENUS I PRM Endometrial Changes Placebo Ulipristal Ulipristal • PRM-associated endometrial 5mg 10mg changes (PAEC) N=56 N=53 N=48 Amenorrhea 1.8% 47.2%* 58.3% • PAEC occurs in 8-20% of women Amenorrhea by day 11 0 43.4%* 58.3%* Change in fibroid volume +7.2% -9.6%* -16.3% • Concern for possible long-term transformation to endometrial Hot flashes 0 5.7% 4.2% hyperplasia/ca Hypertension 0 6.3% 3.0% p<.05 compared with 5mg • PAEC regresses spontaneously after stopping drug Simon et al, Obstet Gynecol, March 2018
Long-Term Ulipristal Ulipristal and Liver Toxicity Endometrial Changes: PEARL IV • Trial of 4 treatment periods, 12 weeks each with December 2017.. menses in between (spontaneous or northindrone) • N=230 on 5mg daily, N=221 on 10mg • EMB prior to treatment, all normal May 2018.. • During study, EMB after each 12 week cycle • Simple hyperplasia, n=3 • Complex atypical hyperplasia, n=1 during study, N=1 at 3 month f/u August 2018… • Endometrial adenocarcinoma, n=1 Donnez et al, Fert Ster, Jan 2016 Ulipristal and Liver Toxicity GnRH Antagonist: Elagolix • 52 cases liver toxicity reported worldwide • Suppresses pituitary-ovarian axis (voluntary reporting!) • NOT Lupron: oral dosing, no hormone “flare” • 4 liver transplants • Phase 2 randomized trial (N=271, 74% African- • 700,000 women who have taken the drug American/black): • Premenopausal women, bleeding >80cc/cycle, 12 week treatment, 200-600mg, QD or BID • 2 groups with add back (daily vs. cyclic progestin)
Aromatase Inhibitors: GnRH Antagonist: Elagolix letrozole and anastrozole • Blocks action of aromatase enzyme in ovaries and peripheral tissue, including fibroids Reduction in blood loss from baseline to last month of treatment Improvement in fibroid symptoms and QOL in Fibroid some, not all groups Hot flashes: Elagolix alone 46-63% Elagolix/add back 19-27% Aromatase Androgens Placebo12% Estrogen Enzyme Archer et al, Fert Steril, July 2017 Letrozole: Decreases Fibroid Volume Aromatase Inhibitors • Benefits • Estrogen levels in serum remain normal • No hot flashes Fibroid • Limitations volume in cc • Small, mostly uncontrolled trials, none in U.S. • No assessment of fibroid symptoms • Long Term Risks • Unknown for premenopausal women • Concern for osteoporosis because postmenopasual women 46% with breast cancer on AIs have increased risk of fracture decrease compared tamoxifen. Parsanezhad et al, Fert Ster: Jan 2010: 93:1
Complementary Treatments Green Tea Randomized Trial • Placebo-controlled trial N=39 • EGCG 800mg vs. Placebo • Improved fibroid symptoms • Increased Hb (11.7 to 12.4 (g/dL) • Anti-inflammatory • Anti-proliferative • Decreased volume 33% • Antioxidant • Animal and in vitro -No information on baseline – Inhibit proliferation and induce apoptosis in fibroid volume fibroid cells -No U.S. data Epigallocatechin (EGCG) Roshdy et al, Jo Women’s Health, 2013 Zhang et al, Fertil Steril 2010 and AJOG 2010 Complementary Treatments Vitamin D: Epidemiologic Evidence • Women with sufficient levels of vitamin D (>20ng/mL) less likely to have uterine fibroids (OR 0.68, CI 0.48-0.96), N=1,036 Baird et al. Epidemiology 2013;24:447-53 • Women with vitamin D deficiency more likely to have fibroids ( OR 2.5, CI 1.2-4.9), N=384 Paffoni et al. J Clin Endocrinol Metab 2013;98:E1374-8 • Reduces cell proliferation • Increases apoptosis • Inverse relationship between vitamin D and fibroid size • Regulates extracellular matrix (ECM) Sabry et al. Int J Womens Health 2013;5:93-100 • Regulates gene transcription of ER/PR
MR Guided Focused Ultrasound Fibroid Devices (MRgFUS) FDA approved 2003, very limited availability across U.S. • Unlike new drugs, FDA does not require comparative trials for new devices • Low quality evidence for devices when enter market • Treatments aim to destroy fibroid tissue, decrease volume, improve symptoms •Focused ultrasound beam heats tissue to 150-185 0 F •Coagulative necrosis occurs MRgFUS Symptom Improvement MRgFUS Outcomes Study N NPV Shrinkage Reoperation Largest trial to date (n=359) Low treatment volumes Stewart et al 359 Variable 20% average Depends on NPV AE: abdominal pain (33%) 2007 ( 24% at 2 years for skin burns (5%) 45% NPV) Gorny 45% 2011 130 N/A 7.4% at 12 mo LeBlang 80 55% 31% at 6 mo N/A 2010 Funaki 2009 91 40% at 24 mo 15% at 34 mo Stewart EA, Gostout B, et al, Obstet Gynecol, Aug 2007
Placebo-controlled Trial of MRgFUS FIRSTT Study: UAE vs. MRgFUS • RCT (n=57) and parallel cohort (n=34) Pilot, N=20 • Compared outcomes within 6 weeks of procedure Symptom severity score • No difference in quantity or quality of AEs -13 MRgFUS: less pain, lower use of opioids/NSAIDS, faster recovery (4 vs. 8 days, p<.001) -31 UAE: Faster procedure (139 vs. 405 minutes, p<.001) p=.90 p=.20 Jacoby V, et al, Fertil Steril, March 2016 Barnard et al, AJOG, May 2017 Radiofrequency Ablation The Radiofrequency Ablation Device • FDA approved for fibroids November 2012 (Acessa) Generator with Foot Pedal 3mm RF Handpiece Laparoscopic Ultrasound
RF Ablation: Current Evidence Radiofrequency Ablation • Fibroids identified with • Largest study, n=135 ultrasound (1cm incision) • FDA pivotal trial • Radiofrequency (RF) probe • Uncontrolled, all women treated with RF ablation placed under ultrasound guidance (3mm incision) Fibroid criteria • Monopolar RF energy delivered to fibroids •<14 week uterus •<6 fibroids • Tissue heats to 100 0 C to •<7cm fibroid cause coagulative necrosis • Fibroid cells reabsorbed Chudnoff et al, Green Jo, May 2013 RF Ablation: Current Evidence RF Ablation: Current Evidence Change in Fibroid and Uterine Volume from Baseline Uterine Volume Fibroid Volume 3 months -15% (CI 11-20)* -40% (CI 36-44)* 12 months -24% (CI 19-30)* -45% (CI 39-52)* 52% decrease in symptom Chudnoff et al, Green Jo, May 2013 *P<.001 score Chudnoff et al, Green Jo, May 2013
Recommend
More recommend