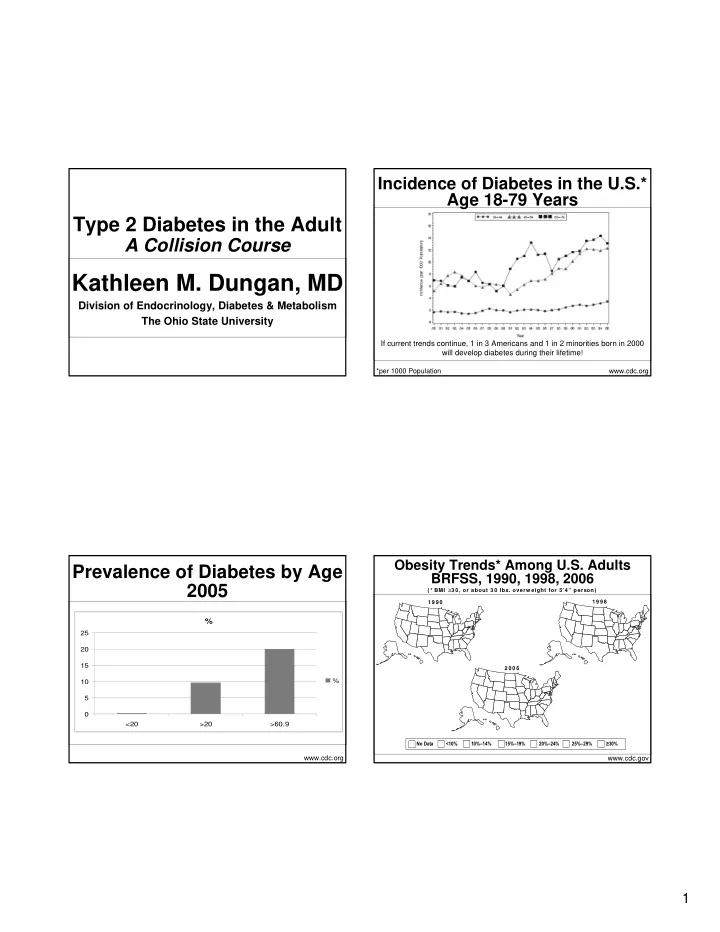
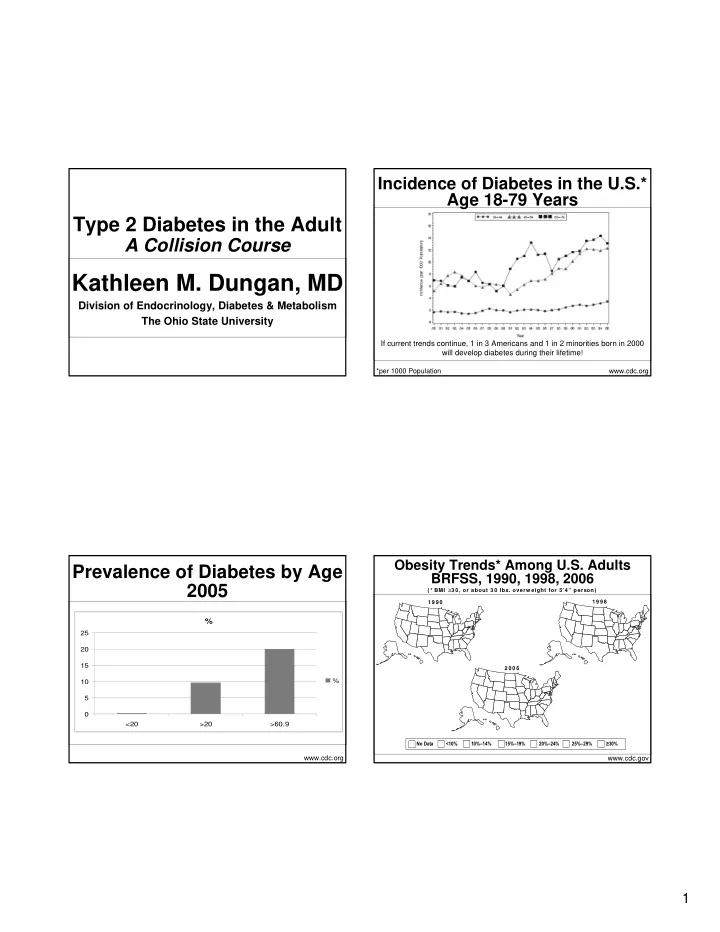
Incidence of Diabetes in the U.S.* Age 18-79 Years Type 2 Diabetes in the Adult A Collision Course Kathleen M. Dungan, MD Division of Endocrinology, Diabetes & Metabolism The Ohio State University If current trends continue, 1 in 3 Americans and 1 in 2 minorities born in 2000 will develop diabetes during their lifetime! *per 1000 Population www.cdc.org Obesity Trends* Among U.S. Adults Prevalence of Diabetes by Age BRFSS, 1990, 1998, 2006 2005 ( * BMI ≥ 3 0, or about 30 lbs. overw eight for 5’4” person) 1 9 9 0 1 9 9 8 % 25 20 15 2 0 0 6 % 10 5 0 <20 >20 >60.9 No Data <10% 10%–14% 15%–19% 20%–24% 25%–29% ≥ 30% www.cdc.org www.cdc.gov 1
Pre-Diabetes The Toll of Diabetes Prevalence of Glucose • 6 th leading cause of death in the U.S. Abnormalities (%) � Only 35% of patients have DM listed on certificate • FBG 100-125 mg/dl 4.9 2.1 � CAD and stroke account for 65% of deaths 18.2 • 2 hour OGTT • Leading cause of new blindness in adults 140-199 mg/dl • Leading cause of renal failure 74.8 • Leading cause of non-traumatic lower limb amputations Known Diagnosis Unknown Diagnosis Prediabet es Normal Glucose Tolerance www.diabetes.org www.diabetes.org Cheng et al Diabetes Care 2008;31:279-284 Diabetes Prevention Economic Costs 2007 Program Direct: $115 billion • 3200 adults with IFG + IGT Indirect: $58.2 billion • 3 Groups $174 billion � Standard care • $11,744 per patient/yr � Intensive lifestyle • 1 in 5 healthcare dollars is spent on � MTF patients with diabetes! ADA; Diabetes Care 2008;31(3):1-20 N Engl J Med. 2002 Feb 7;346(6):393-403. 2
Diabetes Prevention Weight Loss Program • 500-1000 calorie reduction • Lifestyle intervention • Diet alone is generally not effective long- term � Goal 7% weight reduction • Exercise is important for weight � Low-calorie, low fat diet maintenance and improved insulin sensitivity � Exercise 150 min/week • Structured programs that include � Intensive education education, diet, exercise, and regular • F/U 2.8 years contact can produce sustained weight loss of 5-7% N Engl J Med. 2002 Feb 7;346(6):393-403. ADA. Diabetes Care 31 (Suppl 1):S61-S78 Diabetes Prevention MNT Program • Carbohydrates: % of Patients • Metformin should be developing Diabetes � The total amount is more important considered if 11 12 than the type in determining � Very high risk: 10 glycemic effect 7.8 8 4.8 • IGT + IFG 6 � Low glycemic index foods may 4 reduce PPG � Obese 2 0 � <60 years of age Usual Metformin Lifestyle Care N Engl J Med. 2002 Feb 7;346(6):393-403. ADA. Diabetes Care 31 (Suppl 1):S61-S78 3
MNT Efficacy of MNT • Protein 2 1.8 � 15-20% of total calories A1C Reduction % 1.6 � High-protein, low-carb diets 1.4 UKPDS 1.2 • Short-term weight loss Franz 1 0.8 Kulkarn • Improved glycemia 0.6 i Glasgo • Long-term safety and efficacy is 0.4 0.2 unknown 0 • Increased LDL MNT MNT + DSMT ADA. Diabetes Care 31 (Suppl 1):S61-S78 Pastors et al. Diabetes Care 2002;25:608-613 MNT Insurance Coverage • 4 states do not mandate that • Fats insurers cover diabetes � Saturated fats <10% of total treatment and supplies calories � Alabama � Monounsaturated fat and CHO � Idaho should be 60-70% of total calories � Ohio � Cholesterol � North Dakota • <200 mg/day if LDL >100 mg/dl ADA. Diabetes Care 31 (Suppl 1):S61-S78 Pastors et al. Diabetes Care 2002;25:608-613 4
NHANES Data Insurance Coverage • MNT was associated with a 100 90 reduction in 80 � Utilization of hospital 70 56.8 60 services by 9.5% 49.4 50 1999-2000 36.9 � Utilization of physician 40 2001-2002 30 services by 23.5% 20 2003-2004 10 • Savings exceed costs of MNT in 0 patients > 55 years A1C <7% Pastors et al. Diabetes Care 2002;25:608-613 Hoerger et al. Diabetes Care 31:81-86, 2008 U.S. Adults with Diabetes who Measuring Success have ever attended Diabetes Self-Management Class ADA 1 ACE 2 A1C <7%* <6.5% Fasting/preprandial BG 90-130 <110 Postprandial BG <180 <140 (peak) (2 hour) *Goals should be individualized Risks/Benefits of a “normal” A1c (< 6%) are unclear 1. ADA Clinical Practice Recommendations. Diabetes Care 30 (Supp. 1), 2007; www.cdc.org 2. AACE Medical Guidelines for Clinical Practice for the Management of Diabetes Mellitus; Endocr Pract;13(Supp 1), 2007. 5
ADA/EASD Consensus Beta cell function declines over Algorithm time regardless of therapy Proportion of Patients Achieving A1C <7.0% 50 45 40 35 30 Diet SFU 25 20 Metformin 15 Insulin 10 5 0 3 year 6 year 9 year Nathan et al. Diabetes Care 2006;29:1963-1972. Turner et al. UKPDS 49; JAMA. 1999;281(21):2005-12 Matching Pharmacology to Greater glycemic durabililty with Pathophysiology Metformin and Rosiglitazone Monotherapy ↑ Glucagon Incretins p<0.001 Glucose influx secretion Pramlintide α -Glucosidase 35 inhibitors Incretins 30 p<0.001 Pramlintide 25 Insulin ↑ Hepatic Metformin ↓ Insulin Plasma SFU 20 glucose (glitazones ) glucose Glinides secretion Failure rate (%) output 15 Incretins 10 Glitazones (metformin) 5 ↓ Peripheral 0 glucose uptake Rosi Met Gly Kahn et al. N Engl J Med. 2006;355:2427-43 6
Conclusions Incidence • Diabetes places a substantial clinical and • Causes 2 - 3% of all cases of economic burden on the U.S. diabetes in children • Lifestyle changes, as part of a multi- • Mean age of diagnosis 12 - 14 disciplinary approach, can prevent or years delay DM • Highest incidence in ethnic groups • Initial therapy should be individualized and goal-directed with high prevalence of type 2 DM Definition Type 2 Diabetes in Children • Diabetes mellitus which does NOT require insulin for survival Dana S. Hardin, M.D. • Occurs in someone less than 18 years of age. Associate Professor • Does not meet the criterion for The Ohio State University maturity onset diabetes of youth Nationwide Children’s Hospital (MODY) 7
Incidence in Hispanics Characteristics Associated with Increased Incidence and Blacks of Type 2 DM • Southern California 21% of diabetic • Obesity Hispanic patients (Glasser, J.Invest.Med. 1995) • Family history of adult-onset type 2 DM • African-American children had odds ratio of 3.5:1 (boys) and 6.1:1 (girls) compared to • Acanthosis nigricans whites (Pinhaus-Hamiel, J.Ped. 1996) • Children of mothers with gestational • Houston, TX 12.6% of all DM in children diabetes (Yafi and Hardin JPEM 2004) • High-risk ethnicity Pathophysiology of Incidence by Ethnicity Type 2 Diabetes is • Pima children ages: Similar to Adults � 5-14 1:1000 � 15-24 9:1000 • Insulin resistance • Manitoba Native Indians ages: � 7-14 0.5:1000 • Impaired insulin secretion • Japan: • Excessive hepatic glucose production � 2.8-44.6:100,000 • Less well studied in other ethnic groups 8
Insulin Secretion in Insulin-Mediated Whole- Type 2 Diabetes Body Glucose Uptake Glucose Uptake (mg/kg/min) 10 • Initially insulin secretion is augmented to meet 9 the demands of impaired insulin action. 8 7 • Eventually β -cells become “exhausted” and 6 glucose intolerance develops. 5 4 • First phase insulin response remains intact until 3 type 2 DM has been on-going for some time. 2 • Cause of β -cell exhaustion is likely to be glucose 1 toxicity in a genetically predisposed β -cell. 0 Controls NIDDM (DeFronzo, Jm.J.Phys., 1979) Insulin Resistance Increased Hepatic Glucose in Type 2 DM Production in Type 2 DM • Type 2 DM patients have significantly • Increased hepatic glucose production decreased insulin sensitivity and hepatic insulin resistance � Demonstrated by fasting (DeFronzo, Diabetes 1981) hyperinsulinemia • Increased hepatic glucose production � Demonstrated by high insulin to glucose in MZ twins discordant for type 2 DM ratio post-prandially (Vaag, J.Clin.Invest., 1995) � Confirmed by hyperinsulimic euglycemic clamp studies 9
Contribution of Goals of Treatment Gluconeogenesis and Glycogenolysis • Correct hyperglycemia to prevent complications. Hepatic Glucose Output 25 � Traditional the focus has been on 20 reducing pre-meal glucose levels. (µmol/kg/min) � Reduction of post-prandial glucose 15 levels is equally important. 10 • Minimize the risk of hypoglycemia. 5 • Promote optimal psychological and social 0 adaptation to living with diabetes. Control NIDDM (Consoli, Diabetes, 1989) Glycemic and A1c Dose-Response Curve Relating Targets Insulin to the Suppression of HGP Blood 0-2 years 3-6 years 7-12 years >13 years Glucose mg/dl Premeal 100-180 70-150 70-150 70-150 2-3 hour < 200 < 200 < 180 < 180 postmeal Before bed 100-200 100-180 90-160 80-150 2-4 AM > 100 > 100 > 90 > 80 %HbA1c < 8.5 < 8.0 < 7.5 < 7.0 Portal Insulin Concentration Kaufman et al Contemporary Pediatrics 16:112,1999 10
Recommend
More recommend