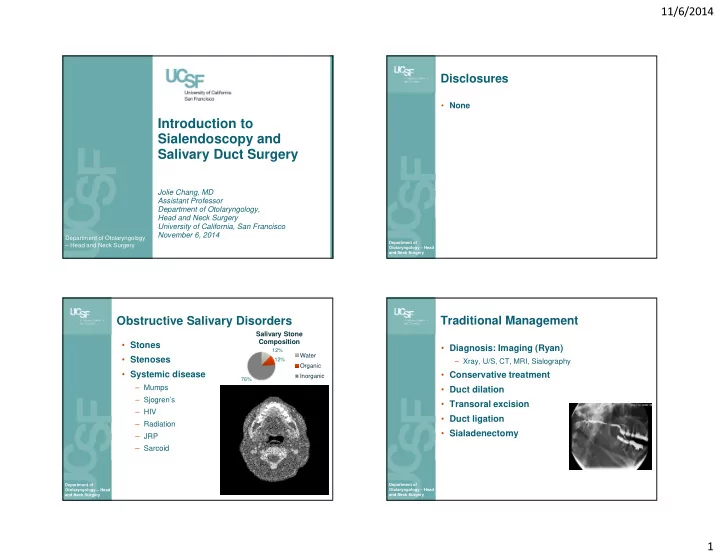
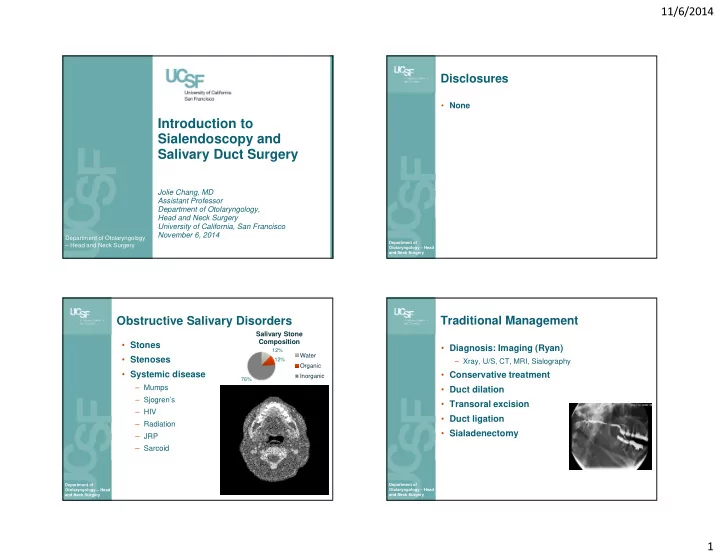
11/6/2014 Disclosures • None Introduction to Sialendoscopy and Salivary Duct Surgery Jolie Chang, MD Assistant Professor Department of Otolaryngology, Head and Neck Surgery University of California, San Francisco November 6, 2014 Department of Otolaryngology Department of – Head and Neck Surgery Otolaryngology – Head and Neck Surgery Obstructive Salivary Disorders Traditional Management Salivary Stone Composition • Stones • Diagnosis: Imaging (Ryan) 12% Water • Stenoses 12% – Xray, U/S, CT, MRI, Sialography Organic • Systemic disease • Conservative treatment Inorganic 76% – Mumps • Duct dilation – Sjogren’s • Transoral excision – HIV • Duct ligation – Radiation • Sialadenectomy – JRP – Sarcoid Department of Department of Otolaryngology – Head Otolaryngology – Head and Neck Surgery and Neck Surgery 1
11/6/2014 Minimally Invasive Approach Sialendoscopy Benefits • Endoscopic visualization of the salivary duct • Diagnostic – Gundlach; Konigsberger et al. HNO. 1990 – Stone location – Nahlieli et al. J Oral Maxillofac Surg. 1994. – Swelling of unknown eitology – Recurrent sialadenitis – Marchal et al. NEMJ. 1999. • Therapeutic – FDA approved 2005 – Stone removal: access to posterior stones – Stenosis dilation – Spares salivary glands – Reduced risk Department of Department of Otolaryngology – Head Otolaryngology – Head and Neck Surgery and Neck Surgery The salivary gland recovers Xerostomia • SMG saliva • Submandibular glands removed for sialolithiasis have normal histology. – 70% of resting salivary flow (Marchal et al 2001) – Xerostomia: Risk for dental caries • After stone removal, salivary function • After SMG removal improves. (Makdissi et al. 2004) – 22% report xerostomia in long-term follow up (Springbog and Moller. Eur Arch Otorhinolaryngol. 2013.) • Animal studies: gland tissue recovers – Reduced unstimulated salivary flow (Cunning et al. Laryngoscope. 1998.) Department of Department of Otolaryngology – Head Otolaryngology – Head and Neck Surgery and Neck Surgery 2
11/6/2014 Contraindication Clinical History • Active infection • History • PMH: prior XRT, RAI, autoimmune disease • Exam: – Salivary expression – Papilla location – Bimanual palpation – Mandibular tori – TMJ, trismus – Imaging Department of Department of Otolaryngology – Head Otolaryngology – Head and Neck Surgery and Neck Surgery Equipment Sialendoscopy Setup • Sialendoscope • General anesthesia – Avoid anticholinergic agents • Diagnostic sheath • Intubation – Single channel – Oral • Therapeutic sheath – Nasal: posterior stones in SMG • Preoperative Medications – Working channel – Antibiotics – Decadron • Positioning Department of Department of ENT today. June 2008. Otolaryngology – Head Otolaryngology – Head and Neck Surgery and Neck Surgery 3
11/6/2014 Equipment (Walvekar) Technique – the Papilla • Identify the papilla – Gland massage – Symmetry – Magnification – Inject papilla – Methylene blue • Papilla dilation – Start with smallest dilator 0000 up to size 3-4 – Avoid making pseudo openings with needle/forceps Department of Department of Otolaryngology – Head Otolaryngology – Head and Neck Surgery and Neck Surgery Technique - Sialendoscopy Examination • Setup • Ducts and branches – Orient camera • Stones – Location – Brightness – Mobility • Introduce sialendoscope – Number – Saline irrigation – no air • Stenoses – Small movements – Location – Backing out helps to find lumen – Extent • Other – Advance under visualization – Foreign body – Be careful of teeth, mandibular tori – Lesions Department of Department of Otolaryngology – Head Otolaryngology – Head and Neck Surgery and Neck Surgery 4
11/6/2014 Stones – Tools for Management • Basket/ Dochotomy • Lithotripsy: Laser – Forceps – Endoscopic drill • Combined approach Department of Department of Otolaryngology – Head Otolaryngology – Head and Neck Surgery and Neck Surgery Lithotripsy Combined approach • Impacted large stones • Due to size & location, stone may not be amenable to endoscopic management • Fragmentation: – Forceps; Hand Drill • Sialendoscopy to localize and characterize the stone – Laser Ho:YAG • Submandibular – ECSWL – Posterior sialodochtomy over palpable stone – Endoscopic Intracorporeal SL • Parotid • Lithotripsy – Transoral sialodochotomy to release distal stones – Slow – Transfacial approach for impacted proximal stones – Can damage duct and scope – Multiple sessions required Department of Department of Otolaryngology – Head Otolaryngology – Head and Neck Surgery and Neck Surgery 5
11/6/2014 Combined Approach Marchal F. Laryngoscope 2007. Department of Department of Otolaryngology – Head Otolaryngology – Head and Neck Surgery and Neck Surgery Stenosis Management Salivary Duct Stenosis • Diagnosis – Sialography • Koch M et al. Oto HNS 2005 – Sialendoscopy: determine – Sialendoscopy in 103 location, extent, length cases with negative imaging (U/S) • Treatment: Dilation – 33% with stones – Dilation: Hydraulic, balloon, – 56% with stenoses – Stents, steroids • Causes of stenosis – Sialodochotomy – Iatrogenic: prior surgery – Combined Approach: Excision, Vein graft – Inflammatory: autoimmune, XRT, RAI – Sialadenectomy Department of Department of Otolaryngology – Head Otolaryngology – Head Marchal et al. J Stoma 2011 . and Neck Surgery and Neck Surgery 6
11/6/2014 Conclusions - Sialendoscopy • Minimally invasive, gland sparing approach • Diagnostic and therapeutic • Treatment of sialolithiasis and stenosis • Reduced need for sialadenectomy Department of Otolaryngology – Head and Neck Surgery 7
Recommend
More recommend