inhibition in ovarian high grade serous ovarian carcinoma Iain - PowerPoint PPT Presentation
HRD as a predictive biomarker for response to PARP inhibition in ovarian high grade serous ovarian carcinoma Iain McNeish Professor of Gynaecological Oncology Wolfson Wohl Cancer Research Centre Institute of Cancer Sciences University of
HRD as a predictive biomarker for response to PARP inhibition in ovarian high grade serous ovarian carcinoma Iain McNeish Professor of Gynaecological Oncology Wolfson Wohl Cancer Research Centre Institute of Cancer Sciences University of Glasgow, UK
Broad assumptions PARP inhibitor sensitivity = f (HRD) PARP inhibitors function by blocking Base Excision Repair
Potential predictive biomarker assays to identify HRD • Functional • Phenotypic • Genomic
Different tests give different results Platinum response 60 – 65% Somatic and germline BRCA1 and TCGA Analysis 51% 2 mutations c.20% 10000 1000 CA125 100 10 0 50 100 150 200 250 Time (Days) TCGA, Nature (2011) 474:609 RAD51 assay 50% Mukhopadhyay, Cancer Res (2012) 72:5675
Potential predictive biomarker assays to identify HRD • Functional • Phenotypic • Genomic
Platinum response Assumption: platinum sensitivity = f (HRD) = PARPi sensitivity High grade serous ovarian cancer Platinum resistant Platinum Sensitive = HR defective
Response to platinum in relapse setting Ledermann et al. Lancet Oncol (2014) 15:852
Platinum response as predictor of single agent response Gelmon et al Lancet Oncol. (2011) 12:852-61
Potential predictive biomarker assays to identify HRD • Functional • Phenotypic • Genomic
TCGA Analysis 51% RAD51 assay 50% Somatic and germline BRCA1 and 2 mutations c.20% Mukhopadhyay, Cancer Res (2012) 72:5675 TCGA, Nature (2011) 474:609 How can genomics identify the other 30%?
Candidate panel gene sequencing – limited utility Differential sensitivity to Non-BRCA HR-pathway rucaparib (siRNA knockdown) gene mutations are rare siRNA knockdown of 28 HR genes in • • Determined frequencies of mutations in 28 3 ovarian cancer cell lines (shown are HR genes in ≈250 women siRNA of 10 genes in OVCAR-3) 16 genes with low frequency mutations • and 12 genes with no mutation found 1.2 Controls 14% IC 50 Fold Change vs NT4 Data source: TCGA HGOC High sensitivity 1 Frequency of Tumours 12% Intermediate sensitivity Low sensitivity 0.8 10% Cumulative frequency of 8% 0.6 non-BRCA HR gene mutations – 13% 6% 0.4 4% 0.2 2% 0 0% IC 50 =half maximal inhibitory concentration.
Defective HR causes widespread genomic damage Abkevich et al, Br J Cancer (2012) 107:1776
Comparative genomic hybridization (CGH) analysis from targeted deep NGS of cancer specimens CN=3 Log 2 ratio CN=2 CN=1 Concomitant change 0.5 0.4 0.3 Allele frequency >3,500 genome-wide SNPs sequenced to support copy number analysis
HRD causes genome-wide loss of heterozygosity (LOH) that can be measured by comprehensive genomic profiling based on NGS BRCA mut Hypothesis 1 : Ovarian cancer patients with high genomic LOH LOH-high suggesting BRCA-like signature will respond to rucaparib. BRCA wt Hypothesis 2 : Ovarian cancer patients who are “Biomarker Negative” LOH-low (ie, with low genomic LOH) will not respond to rucaparib. Chromosome No. NGS=next-generation sequencing; mut=mutation; wt=wild type.
HGSC patients can be classified into three molecular subgroups: BRCA mut , BRCA-like, Biomarker Negative BRCA wt Tumors LOH-low LOH-high BRCA mut Frequency of Genomic LOH cutoff Extent of Genomic LOH 15
Initial genomic LOH cutoff derived from public data and prospectively tested in ARIEL2 TCGA and AOCS overall survival data used to develop LOH cutoff to identify HGOC patient tumors with BRCA-like signature 100 0.30 High genomic LOH (n=97) Low genomic LOH (n=212) (high vs low LOH groups) 0.25 80 Survival Probability Log-rank P Value 0.20 Log-rank: P =0.0047 60 Hazard ratio=0.62 0.15 Independent predictor from 40 Optimal LOH cutoff BRCA mut status 0.10 20 Median overall survival: 0.05 56.4 vs 38.2 months 0 0 0 25 50 75 100 125 Genomic LOH Cutoff Overall Survival (months) Prospective testing of prespecified cutoff in ARIEL2 TCGA. Nature. (2011);474:609 Wang ZC et al. Clin Cancer Res. (2012);18:5806
Myriad myChoice cutoff Timms et al. Clin Cancer Res. (2016) 22:3764
ARIEL2 designed to assess rucaparib efficacy in three prospectively defined molecular subgroups Key Eligibility (N=180) • High-grade serous or BRCA mut Analysis of HRD endometrioid OC NGS of tumour Subgroups – Known gBRCA tissue allows Primary endpoint enrollment capped patients to be PFS at N=15 • classified LOH-high Secondary endpoints • ≥1 prior platinum chemotherapy • ORR 600 mg BID • Platinum-sensitive, relapsed, – RECIST rucaparib until measurable disease disease progression – RECIST + CA-125 • Tumour tissue (screening Safety • LOH-low biopsy and archival) • PK gBRCA=germline BRCA.
Overall similar genomic LOH levels between matched archival tumors and screening biopsies Increased genomic LOH levels found in only a subset of screening biopsies compared to matched archival tumors All patients (117 matched pairs) LOH high LOH low archival archival LOH high 67 17 screening LOH low 0 33 screening Classified into LOH high and LOH low groups based on the prespecified genomic LOH cutoff. 19
Final efficacy analysis Ariel2: PFS in BRCA mut and LOH-high versus LOH-low patients
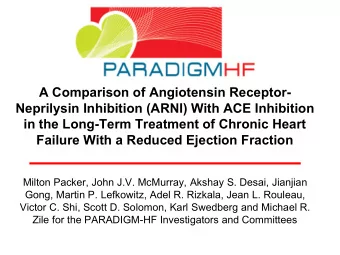
Final efficacy analysis NOVA: PFS in gBRCA mut and HRD positive versus HRD negative patients gBRCA WT gBRCA mut HRD positive HRD negative HR= 0.27 HR= 0.38 HR= 0.58 Mirza et al NEJM (2016) ePub 8 th Oct 2016
Duration of response in BRCA mut , LOH-high, and LOH-low patients Median duration of HRD Subgroup response, mo (95% CI) BRCA mut 9.8 (6.4, 12.9) LOH-high 10.8 (5.7, -) LOH-low 5.6 (4.6, 8.5)
Tumours with RAD51C alterations are BRCA-like (high genomic LOH) and responded to rucaparib HR-pathway Genetic Germline/somatic HRD molecular RECIST CA-125 gene alteration type inference subgroup response response NBN Truncation Germline Biomarker Negative PR Yes RAD51C Truncation Germline BRCA-like PR Yes RAD51C Homozygous Del Somatic BRCA-like PR Yes RAD51C Splice Germline BRCA-like PR Yes RAD51C Splice Germline BRCA-like SD Yes ATM Homozygous Del Somatic Indeterminate SD Yes RAD51L3 Truncation Indeterminate BRCA-like SD Yes BRIP1 Splice Germline Biomarker Negative SD No BRIP1 Truncation Germline Biomarker Negative SD No CHEK2 Splice Indeterminate Biomarker Negative SD No CHEK2 Truncation Germline BRCA-like SD No RAD51L1 Truncation Indeterminate Biomarker Negative SD No NBN Truncation Germline Indeterminate SD NE RAD54L Truncation Somatic (subclonal) Biomarker Negative SD NE FANCA Homozygous Del Somatic BRCA-like SD NE FANCI Truncation Germline Biomarker Negative PD No ATM Truncation Somatic Indeterminate NE NE PR=partial response; SD=stable disease; PD=progressive disease; NE=not evaluable.
LOH high as a predictor of response in BRCA wt tumours Sensitivity (%) p value LOH high 78 - HRD mutation 11 <0.001 BRCA1/RAD5 1C 48 0.02 methylation HRD mutation or BRCA1/RAD5 1C 59 0.13 methylation 24
How to assess HRD in 2016 • Germline or somatic BRCA1/2 (+/- RAD51C ) mutations • Platinum sensitivity matters – “extreme platinum responders” • LOH analyses more sensitive than either panel sequencing or methylation analyses • Archival tissues can be adequate but fresh biopsy preferable
NOVA – extreme platinum responders HGSC = 70% • Relapse in platinum-sensitive timeframe = 80% of • 70% CR/Excellent PR to platinum in relapse setting = 40 • - 50% of 80% of 70% 22 - 28% all HGSC patients
Ovarian high-grade serous carcinoma • Extreme chromosomal instability TCGA, Nature (2011) 474:609
Hoadley et al, Cell (2014) 158:929
Recommend
More recommend
Explore More Topics
Stay informed with curated content and fresh updates.







![Try it >>> for name in ["Andrew", "Teboho", "Xian"]:](https://c.sambuz.com/720005/try-it-s.webp)