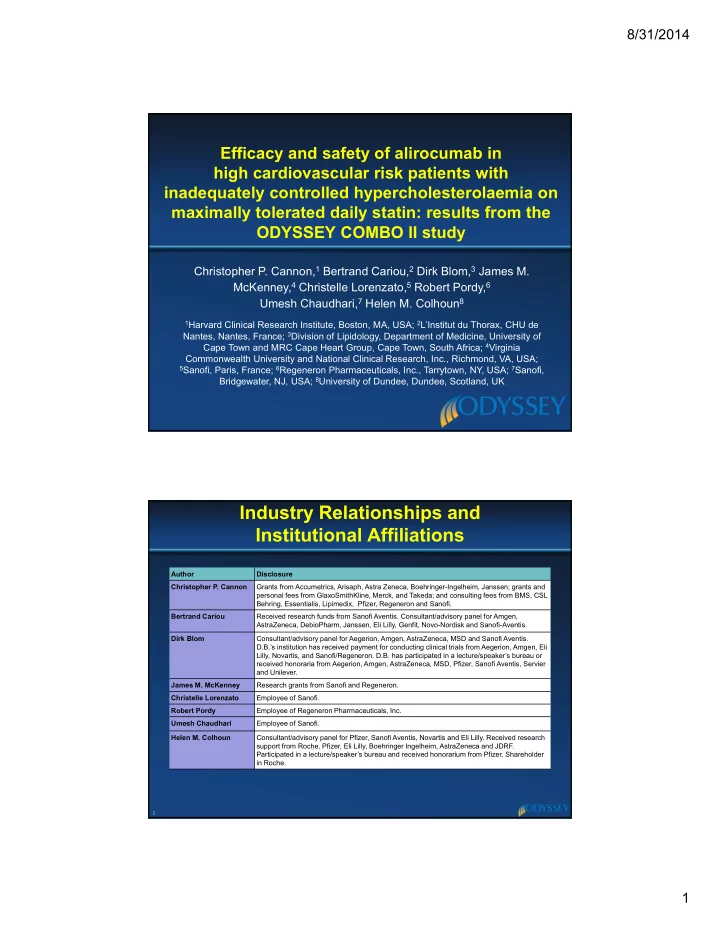
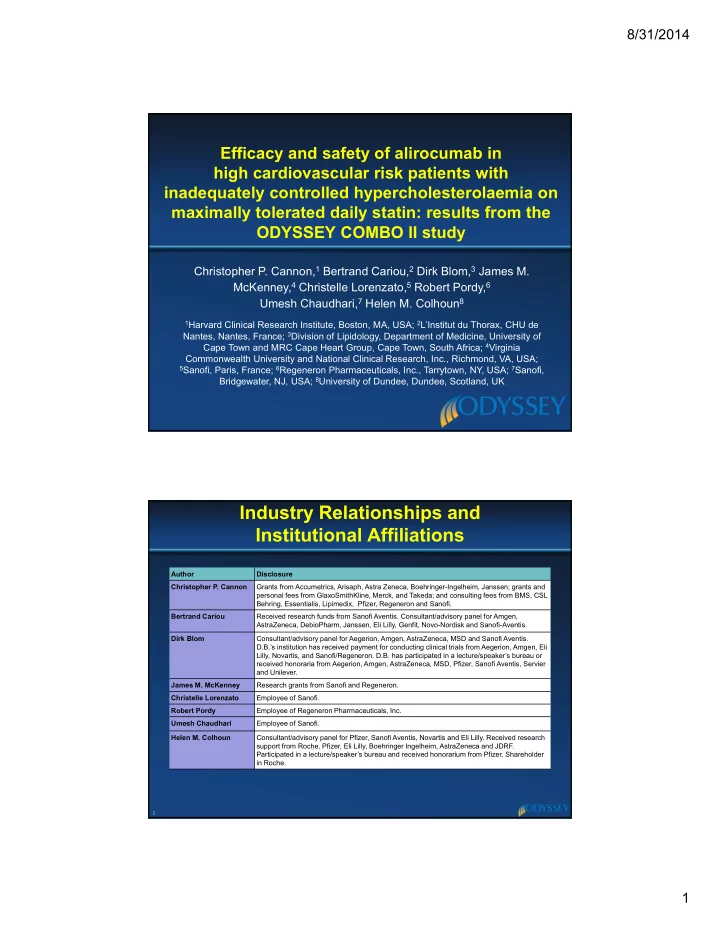
8/31/2014 Efficacy and safety of alirocumab in high cardiovascular risk patients with inadequately controlled hypercholesterolaemia on maximally tolerated daily statin: results from the ODYSSEY COMBO II study Christopher P. Cannon, 1 Bertrand Cariou, 2 Dirk Blom, 3 James M. McKenney, 4 Christelle Lorenzato, 5 Robert Pordy, 6 Umesh Chaudhari, 7 Helen M. Colhoun 8 1 Harvard Clinical Research Institute, Boston, MA, USA; 2 L’Institut du Thorax, CHU de Nantes, Nantes, France; 3 Division of Lipidology, Department of Medicine, University of Cape Town and MRC Cape Heart Group, Cape Town, South Africa; 4 Virginia Commonwealth University and National Clinical Research, Inc., Richmond, VA, USA; 5 Sanofi, Paris, France; 6 Regeneron Pharmaceuticals, Inc., Tarrytown, NY, USA; 7 Sanofi, Bridgewater, NJ, USA; 8 University of Dundee, Dundee, Scotland, UK Industry Relationships and Institutional Affiliations Author Disclosure Christopher P. Cannon Grants from Accumetrics, Arisaph, Astra Zeneca, Boehringer-Ingelheim, Janssen; grants and personal fees from GlaxoSmithKline, Merck, and Takeda; and consulting fees from BMS, CSL Behring, Essentialis, Lipimedix, Pfizer, Regeneron and Sanofi. Bertrand Cariou Received research funds from Sanofi Aventis. Consultant/advisory panel for Amgen, AstraZeneca, DebioPharm, Janssen, Eli Lilly, Genfit, Novo-Nordisk and Sanofi-Aventis. Dirk Blom Consultant/advisory panel for Aegerion, Amgen, AstraZeneca, MSD and Sanofi Aventis. D.B.’s institution has received payment for conducting clinical trials from Aegerion, Amgen, Eli Lilly, Novartis, and Sanofi/Regeneron. D.B. has participated in a lecture/speaker’s bureau or received honoraria from Aegerion, Amgen, AstraZeneca, MSD, Pfizer, Sanofi Aventis, Servier and Unilever. James M. McKenney Research grants from Sanofi and Regeneron. Christelle Lorenzato Employee of Sanofi. Robert Pordy Employee of Regeneron Pharmaceuticals, Inc. Umesh Chaudhari Employee of Sanofi. Helen M. Colhoun Consultant/advisory panel for Pfizer, Sanofi Aventis, Novartis and Eli Lilly. Received research support from Roche, Pfizer, Eli Lilly, Boehringer Ingelheim, AstraZeneca and JDRF. Participated in a lecture/speaker’s bureau and received honorarium from Pfizer. Shareholder in Roche. 2 1
8/31/2014 ODYSSEY COMBO II Study Design Follow-up (8 weeks) Double-blind treatment period (104 weeks) High CV-risk High CV-risk patients on patients on Alirocumab 75 mg with potential ↑ to 150 mg Q2W SC max-tolerated statin † max-tolerated statin † + placebo ezetimibe PO (single 1-mL injection using prefilled pen for self-administration) LDL-C ≥ 1.81 mmol/L LDL-C ≥ 1.81 mmol/L n=479 [70 mg/dL] [70 mg/dL] Per-protocol dose ↑ possible based (history of CVD) (history of CVD) R on pre-specified LDL-C level or or n=241 ≥ 2.59 mmol/L ≥ 2.59 mmol/L Ezetimibe 10 mg/day PO [100 mg/dL] [100 mg/dL] + placebo Q2W SC (no history of CVD) (no history of CVD) W4 W8 W16 Assessments W0 W12 W24 W36 W52 W64 W76 W88 W104 Dose ↑ if Primary Pre-specified analysis LDL-C >70 mg/dL endpoint Efficacy: All Patients To W52 at W8 Safety: Baseline-W102 (all patients at least W52) † Other LLT not allowed. Clinicaltrials.gov identifier: NCT01644188. 3 Baseline Characteristics All patients on background max Alirocumab Ezetimibe tolerated statin (n=479) (n=241) Age, years, mean ( SD ) 61.7 ( 9.4 ) 61.3 ( 9.2 ) Male, % (n) 75.2% (360) 70.5% (170) Race, White, % (n) 84.3% (404) 85.5% (206) BMI, kg/m 2 , mean ( SD ) 30.0 ( 5.4 ) 30.3 ( 5.1 ) CHD history, % (n) 91.2% (437) 88.0% (212) Hypertension, % (n) 79.7% (382) 82.2% (198) Type 2 diabetes, % (n) 30.3% (145) 31.5% (76) Any statin † ,% (n) 99.8% (478) 100% (241) High-intensity statin ‡ , % (n) 66.8% (320) 66.4% (160) LDL-C, calculated 2.8 ( 0.9 ) 2.7 ( 0.9 ) mean ( SD ) , mmol/L [mg/dL] [109 ( 37 ) ] [105 ( 34 ) ] † Patients should receive either rosuvastatin 20-40 mg, atorvastatin 40-80 mg daily, or simvastatin 80 mg daily unless not tolerated and/or appropriate other dose given according to the judgement of the investigator. ‡ High-intensity statin: atorvastatin 40-80 mg or rosuvastatin 20-40 mg daily. 4 2
8/31/2014 Alirocumab Significantly Reduced LDL-C from Baseline to Week 24 versus Ezetimibe Primary Endpoint: Percent Change from Baseline to Week 24 in LDL-C All patients on background of maximally-tolerated statin n=467 n=240 0 LS mean (SE) % change from -10 baseline to Week 24 Alirocumab 18.4% -20 had Ezetimibe dose -20.7% -30 increase at W12 -40 -50 LS mean difference (SE) vs. ezetimibe: − 29.8% (2.3); P <0.0001 -50.6% -60 Intent-to-treat (ITT) analysis 5 Alirocumab Maintained Consistent LDL-C Reductions over 52 Weeks Achieved LDL-C Over Time on Background of Maximally-Tolerated Statin 3 116 Ezetimibe LDL-C, LS mean (SE), mmol/L 109 2.8 Alirocumab 102 2.6 2.2 mmol/L 95 2.4 2.1 mmol/L 85.3 mg/dL 88 82.5 mg/dL 2.2 mg/dL 81 − 18.3% 2 − 20.7% 74 1.8 67 1.4 mmol/L 1.6 1.3 mmol/L 60 53.3 mg/dL 51.6 mg/dL 1.4 53 − 49.5% 1.2 − 50.6% 46 1 39 0 4 8 12 16 20 24 28 32 36 40 44 48 52 Week Dose ↑ if LDL-C >70 mg/dL at W8 Intent-to-treat (ITT) analysis 6 3
8/31/2014 Most of These High CV-Risk Patients Receiving Alirocumab on Background Statin Achieved LDL-C Goal All patients on background of maximally-tolerated statin Proportion of Patients Reaching Proportion of Patients Reaching LDL-C <1.81 mmol/L (70 mg/dL) at Week 24 LDL-C <1.3 mmol/L (50 mg/dL) at Week 24 Alirocumab 90 90 Ezetimibe 77.0% 80 80 70 70 60.3% 60 60 % patients 45.6% 50 50 % patients 40 40 30 30 20 20 14.2% 10 10 0 0 P <0.0001 Post hoc Intent-to-treat (ITT) analysis 7 Safety Analysis (Baseline-W102) Including All Data Collected Until Last Patient Visit at Week 52 % (n) of patients Alirocumab Ezetimibe All patients on background max (n=479) (n=241) tolerated statin TEAEs 71.2% (341) 67.2% (162) Treatment-emergent SAEs 18.8% (90) 17.8% (43) TEAE leading to death † 0.4% (2) 1.7% (4) TEAEs leading to discontinuation 7.5% (36) 5.4% (13) Adverse Events of Interest Adjudicated CV events ‡ 4.8% (23) 3.7% (9) Injection-site reactions 2.5% (12) 0.8% (2) Neurocognitive disorders 0.8% (4) 1.2% (3) ALT >3 x ULN 1.7% (8/470) 0.4% (1/240) Creatine kinase >3 x ULN 2.8% (13/467) 2.5% (6/236) † Both deaths in the alirocumab arm were due to CV events (cardiac arrest and sudden cardiac death). Of the four deaths in the ezetimibe arm, two were due to CV events (malignant lung neoplasm, suicide, defect conduction intraventricular, sudden cardiac death and sudden death – one patient was counted in two categories) ‡ Adjudicated CV events include all CV AEs positively adjudicated. The adjudication categories are the following: CHD death, non-fatal MI, fatal and non-fatal ischemic stroke, unstable angina requiring hospitalisation, congestive heart failure requiring hospitalisation, ischemia driven coronary revascularisation procedure [PCI, CABG]. Statistical analyses have not been performed. 8 4
8/31/2014 Safety Analysis (Baseline-W102) TEAEs Occurring in ≥ 5% of Either Alirocumab or Ezetimibe Patients % (n) of patients Alirocumab Ezetimibe All patients on background max (n=479) (n=241) tolerated statin Upper respiratory tract infection 6.5% (31) 5.8% (14) Accidental overdose † 6.3% (30) 6.6% (16) Dizziness 4.8% (23) 5.4% (13) Myalgia 4.4% (21) 5.0% (12) † Accidental overdose is an event suspected by the Investigator or spontaneously notified by the patient (not based on systematic injection/capsule counts) and defined as at least twice the intended dose within the intended therapeutic interval (i.e., ≥ 2 injections from the double-blind treatment kit administered in <7 calendar days or ≥ 2 capsules from the double-blind treatment kit are administered within 1 calendar day). Statistical analyses have not been performed. 9 Conclusions In this population of high CV-risk patients who had poorly controlled LDL-C on maximally-tolerated statin therapy: – LDL-C ↓ from baseline maintained with alirocumab: significantly greater ↓ vs. ezetimibe at W24, 51% vs 21% ( P <0.0001) – Self-administered alirocumab had good compliance and was well-tolerated – This “treat-to-target” approach with alirocumab resulted in ~80% pts not requiring a dose ↑ to 150 mg at W12 – 77% of alirocumab pts achieved LDL-C <1.81 mmol/L (70 mg/dL) at W24 – Mean achieved LDL-C levels of 1.4 mmol/L (53.3 mg/dL) at W52 with alirocumab – TEAEs similar between alirocumab and ezetimibe arms 10 5
8/31/2014 Thank you to all principal investigators and national coordinators! Russia: 15 sites Canada: France: 4 sites Hungary: 4 sites 5 sites Ukraine: 2 sites Denmark: USA: 9 sites Israel: 58 sites South Korea: 7 sites 14 sites South Africa: 8 sites 126 sites worldwide 11 6
Recommend
More recommend