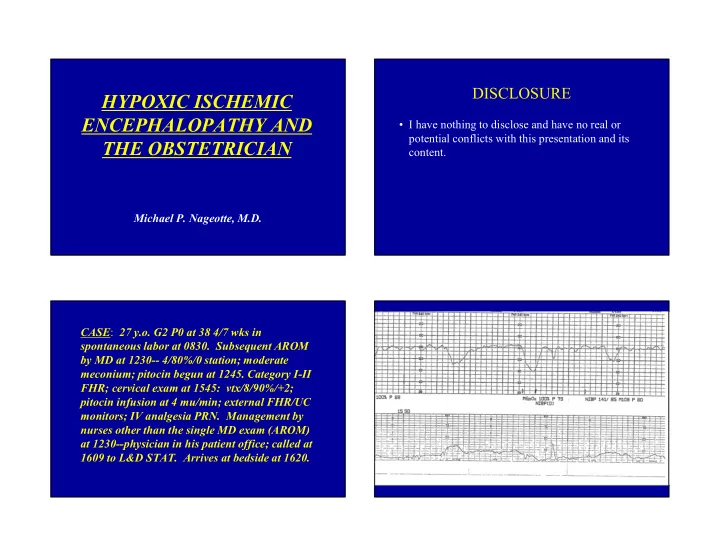
DISCLOSURE HYPOXIC ISCHEMIC ENCEPHALOPATHY AND • I have nothing to disclose and have no real or potential conflicts with this presentation and its THE OBSTETRICIAN content. Michael P. Nageotte, M.D. CASE : 27 y.o. G2 P0 at 38 4/7 wks in spontaneous labor at 0830. Subsequent AROM by MD at 1230-- 4/80%/0 station; moderate meconium; pitocin begun at 1245. Category I-II FHR; cervical exam at 1545: vtx/8/90%/+2; pitocin infusion at 4 mu/min; external FHR/UC monitors; IV analgesia PRN. Management by nurses other than the single MD exam (AROM) at 1230--physician in his patient office; called at 1609 to L&D STAT. Arrives at bedside at 1620.
DELIVERY ROOM DATA • Emergency primary L/T C/S under general anesthesia with skin incision at 1630 and delivery at 1632 • 2310 gm SGA male; tight NC x3 with thin cord; thick meconium; Apgars 1/4/4 at one, five and ten minutes • Cord gases: Artery 6.99/115/10/-12; Vein 7.04/84/15/-8 • Several intubations and full CPR in Delivery Room • In NICU, early onset seizures; unable to oxygenate well and requiring intubation; Admit Dx: “Hypoxic Ischemic Encephalopathy”; transfer to Level III for total body cooling despite IUGR
Question NOMENCLATURE Should the admitting diagnosis to the NICU be • Hypoxia hypoxic ischemic encephalopathy? • Acidosis A. Yes 82% • Asphyxia B. No • Neonatal Encephalopathy • Hypoxic Ischemic Encephalopathy (HIE) 18% • Cerebral Palsy • Negligence s o e N Y It is critical to understand that the What do these terms mean, are diagnostic labels applied to the they different, what causes them neurologically depressed neonate have and can they be prevented? potentially profound consequences for the child, the family, the physicians for both mother and baby, the nurses and the hospital.
ASPHYXIA Hypoxia : Reduced amount of oxygen delivered to tissues; encephalopathy or brain injury unlikely in the fetus or newborn • Condition of impaired gas exchange leading, if it Hypoxemia: Reduced oxygen concentration in blood; associated persists, to progressive hypoxemia and hypercapnia with hypoxia but injury unlikely if adequate cerebral blood flow with a significant metabolic acidosis resulting Hypoxia-Ischemia: Reduced oxygen and inadequate volume (World Federation of Neurology, 1993) of blood delivered to tissues; can cause brain injury if both intracellular oxygen and glucose remain below critical levels • This term describes a process of varying severity and Metabolic Acidosis: Low pH due to increased lactic acid in the duration rather than an endpoint and should not be blood reflecting severity of asphyxia and/or hypoxia-ischemia applied to birth events unless specific evidence of Respiratory Acidosis: Low pH due to increased carbon dioxide markedly impaired intrapartum or immediate postnatal in blood; may protect the fetal/neonatal brain due to reflex gas exchange can be linked to neurologic illness in the cerebral vasodilation and increased cerebral blood flow neonate (Low, 1997) Mixed Acidosis: Low pH reflecting both increased carbon dioxide (respiratory) and lactic acid (metabolic); most common form of clinically significant neonatal acidosis NEONATAL ENCEPHALOPATHY NEONATAL • A clinically defined syndrome of disturbed neurologic function in the earliest days of ENCEPHALOPATHY life in a neonate at or beyond 35 weeks of gestation, manifested by subnormal level of consciousness or seizures often accompanied by difficulty with initiating and maintaining respiration and with various degrees of depression of both muscle tone and reflexes.
NEONATAL ENCEPHALOPATHY Potential Etiologies of Neonatal Encephalopathy • Applied in various clinical settings with altered neurologic signs in neonates born > 35 weeks • Chronic persistent or acute fetal • Descriptive term which is often erroneously hypoxemia/ischemia interchanged with such terms as hypoxia, acidosis • Maternal/Fetal(FIRS)/Neonatal Infection and asphyxia particularly during the immediate • Inborn errors of metabolism; genetics neonatal period and continued throughout the • Trauma (skull fracture, CNS bleeding) medical chart • Coagulation disorders, acute anemia • Generally classified as mild, moderate or severe • Fetal/Neonatal Stroke; anomalies (Sarnat classification) with death or developmental impairment usually confined to • Unknown infants with moderate or severe NE Hypoxic Ischemic Encephalopathy • Assumptions on the role of intrapartum events on newborn and neonatal status have given rise to the term HYPOXIC ISCHEMIC hypoxic ischemic encephalopathy (HIE) • HIE (post-asphyxial encephalopathy, birth asphyxia, ENCEPHALOPATHY perinatal asphyxia) describes a subset of NE present in the first week of life in term/near term infants believed to have experienced significant hypoxemia/asphyxia prior to or during labor and delivery • Findings: altered consciousness, tone and reflexes; the most severe state characterized by hypotonia, apnea/respiratory depression, coma and seizures • Diagnosis confirmed with specific MRI changes
Question Since the introduction of continuous fetal heart rate monitoring in, the reported rate of cerebral palsy in CEREBRAL PALSY the developed world has: 80% A. increased B. decreased C. remained unchanged 17% 3% d d d e e e s s a a g n e e a r r c c h n e c i d n u d e n i a m e r CEREBRAL PALSY CEREBRAL PALSY Cerebral palsy describes a group of conditions specifically involving motor disability of early onset • Associated impairments including vision, hearing, which, despite a wide range of possible abilities and cognition, speech, epilepsy and behavioral disorders disabilities, must satisfy the following: often accompany the motor impairment. 1) motor disorder (specifically, spasticity, dyskinesia, ataxia, mixed or hypotonia) is present by age of four • The more severe the motor impairment, the more 2) cerebral not peripheral nerve or muscular abnormality likely that a number of these impairments will add to 3) arises early in development the complexity of the disorder. 4) is not progressive or degenerative but life-long and • For term and near term infants, if CP is present it is with no known cure generally a more severe form with milder CP evident 5) may or may not be associated with other neurological only in surviving preterm infants. or intellectual abnormalities 6) if fetal asphyxia is implicated, the CP must be of the spastic quadriparetic or dyskinetic type
Elective and Emergency C-Sections and CEREBRAL PALSY Live Births with Cerebral Palsy in Western Australia, 1980-2009 • The risk of CP increases substantially as gestational age at birth decreases with < 32 weeks gestation being the strongest risk factor for CP. • While death and CP in the very preterm have declined steadily since the mid 1990s, this has had little impact on the overall prevalence of CP as births < 34 weeks comprise only 2% of all births. • Term and late preterm infants are at low risk for CP yet comprise 60% of CP cases (term/late preterm neonates account for 98% of all births). • Term CP rates have remained remarkably stable with the rate of 2/1000 consistent throughout the developed world for the past several decades. THREE ETIOLOGICAL GROUPS OF THREE GROUPS OF NEONATAL NEONATAL ENCEPHALOPATHY ENCEPHALOPATHY • In a minority of cases, encephalopathy is likely due • In a second subset of encephalopathy cases, an etiology to hypoxia-ischemia, with specific MRI established different from hypoxia-ischemia is identified (e.g. abnormalities, following a recognized obstetrical trauma, infection or specific metabolic disorder). sentinel event (e.g. uterine rupture, cord prolapse, maternal cardiac arrest). • The third group is the largest and presents a clinical conundrum as there is a lack of an obvious cause of • In such incontrovertible cases, HIE is frequently the accepted cause of encephalopathy but not all the neurologic abnormalities identified. sentinel events result in HIE and one cannot • Different etiologies of encephalopathy must be kept in implicate hypoxia-ischemia with 100% certainty mind in all cases and a clear history of hypoxia- because it is not possible to document blood flow ischemia associated with a sentinel event does not rule and oxygenation of the fetal brain. out other causes or contributors to the findings.
PRIMATE MODE OF TERM Magnetic Resonance Imaging NEONATAL BRAIN INJURY (R. • Dramatically improved technology with visualization Myers, 1972, 1975) of myelination and changes in cerebral structures • Specific regional distribution of injury • More sensitive and specific than U/S or CT associated with different durations and • Shows heterogeneous pattern, ranging from cortical severities of experimental ischemia (rhesus) dysplasia to focal infarcts and atrophy or basal ganglion lesions (related to insult timing/severity) • Prolonged partial asphyxia: cerebral white • Better anatomical resolution, particularly in the matter injury basal ganglia, thalamus and periphery of the • Acute profound asphyxia: deep gray nuclei cerebral cortex (basal ganglia and thalamus) injury rarely • Detects discrete lesions in cerebellum and brain stem with extension to white matter MRI PATTERNS OF INJURY-HIE AND ITS PRESUMED ETIOLOGIES So When Does the Injury 1 ) Selective neuronal necrosis of the cortex, predominantly the hippocampus and also the Occur? grey matter nuclei 2) Leucomalacia of periventricular to subcortical white matter 3) Focal or more generalized infarction There is dynamism to the MRI pattern until the final pattern is achieved.
Recommend
More recommend