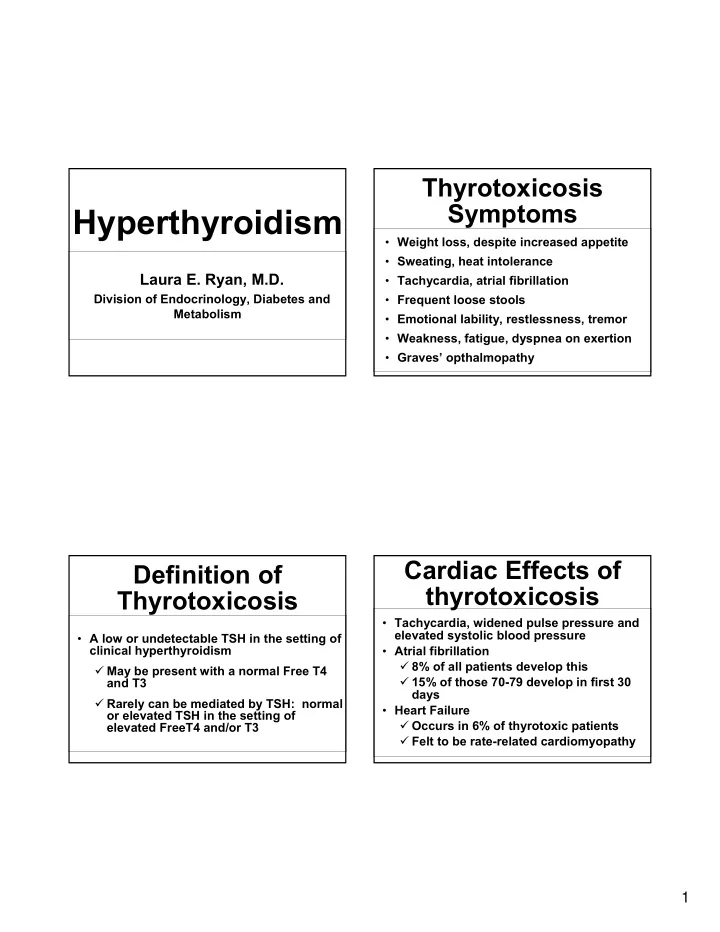
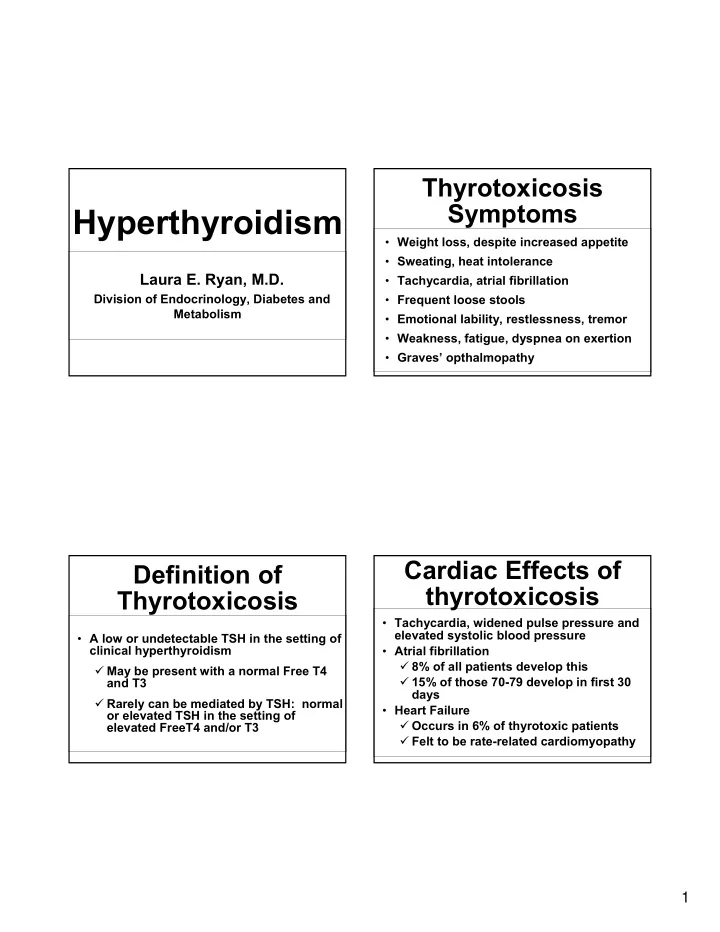
Thyrotoxicosis Symptoms Hyperthyroidism • Weight loss, despite increased appetite • Sweating, heat intolerance Laura E. Ryan, M.D. • Tachycardia, atrial fibrillation Division of Endocrinology, Diabetes and • Frequent loose stools Metabolism • Emotional lability, restlessness, tremor • Weakness, fatigue, dyspnea on exertion • Graves’ opthalmopathy Cardiac Effects of Definition of thyrotoxicosis Thyrotoxicosis • Tachycardia, widened pulse pressure and elevated systolic blood pressure • A low or undetectable TSH in the setting of clinical hyperthyroidism • Atrial fibrillation � 8% of all patients develop this � May be present with a normal Free T4 � 15% of those 70-79 develop in first 30 and T3 days � Rarely can be mediated by TSH: normal • Heart Failure or elevated TSH in the setting of � Occurs in 6% of thyrotoxic patients elevated FreeT4 and/or T3 � Felt to be rate-related cardiomyopathy 1
Physical Exam Critical diagnostic test: I 131 Uptake and Scan Findings • Tachycardia, systolic HTN • Low iodine uptake • High iodine uptake • Pressured speech, being “fidgety” � Thyroiditis � Graves’ disease • Exophthalmos, lid lag, scleral show � Exogenous � Toxic MNG • Goiter, thyroid nodule or tender thyroid � Ectopic � Toxic adenoma � Bruit over goiter pathognomonic for Graves’ � Iodine-induced � “hashitoxicosis” • Warm, sweaty skin that may be “smooth” � amiodarone � TSH-mediated • Fine tremor, brisk reflexes Suspect Graves’ Disease thyrotoxicosis: • Autoimmune hyperthyroidism TSH • Caused by antibodies that activate the TSH receptor TSH 0.1-0.4 TSH <0.1 TSH >0.4 � TSH receptor Ab’s and Thyroid Subclinical hyperthyroidism Normal Stimulating Immunoglobulin hyperthyroidism • “Hashimoto’s” antibodies usually also present: Anti thyroid peroxidase Abs Radioiodine Uptake and scan 2
Graves’ Disease • Peak incidence 30-50yo • Strong familial predisposition • Female:male 9:1 • 15-25% remission rate with medical management � Usually in patients with mild disease on presentation Radioiodine uptake and scan In Graves’ disease: • Uptake is high usually >50% • Scan shows diffuse, symmetric uptake Brent GA, NEJM 2008 Jun 12;358(24):2594-605. 3
Toxic Adenoma and Graves’ Disease Ophthalmopathy Exopthalmos (Proptosis) Toxic MNG • Focal hyperplasia of thyroid follicular cells with functional capacity which is independent of TSH regulation • More common in those >50yo • Localized, somatic activating mutation of the TSH receptor gene • Rarely if ever spontaneously remits • Can be associated with isolated T3 toxicosis 4
Radioiodine Scan of Toxic Multinodular Goiter Antithyroid Medications, cont • PTU – comes in 50mg tablets � Start at 100mg or 150mg TID � Non-compliance with TID dosing frequent • Methimazole – 5mg and 10mg tablets � Start at 20-30mg qd x 5d then can frequently decrease to 10mg per day • If they’ve been on these meds for 12mo and still hyper, the thyrotoxicosis is NOT going away – move to definitive therapy Uptake % may be WNL Scan shows patchy, heterogeneous uptake Treatment: Medications Treatment: I 131 • Beta blockade for symptomatic relief of • In Graves disease, goal should be total palpitations and cardio-protection ablation of thyroid gland • Thionamides: PTU and Methimazole � Typical doses of 10-22mCi � PTU: more inconvenient TID dosing • TMNG, can try to ablate hyperfunctional nodule(s) and leave remaining normal � Methimazole: Once daily tissue intact � 5% develop pruritic rash • Takes 6 weeks to 6 months for ablation � With longer exposure of higher doses, • Very safe: used since 1950’s with no agranulocytosis and elevated LFTs increased incidence cancer or leukemia 5
Thyroid Surgery for Definitive Radiation Safety Treatment of Hyperthyroidism • 3 foot (arm’s length) distance x 3 days � Should avoid small children completely • Avoid exposure to body fluids for 7 days • Avoid pregnancy for 6-12 months • Actual radiation dose/exposure is very small: similar to flying in a plane from Columbus to San Francisco and back! I 131 Therapy: follow-up Thyroid Surgery • Not first choice in most • Draw labs in 4 weeks: thyrotoxic pts FreeT4 • Risk of surgical complications � Every 4 weeks � Hypoparathyroidism • Begin Synthroid once FT4 is in the lower part � Recurrent laryngeal of the normal range nerve injury • Patient must be • Synthroid dosing: euthyroid prior to 1.6mcg/kg surgery 6
Subacute thyroiditis, Thyroid Surgery continued • Will not respond to Antithyroid medications • Treatment of Choice in Select individuals: or I 131 � Severe hyperthyroidism that failed I 131 • Beta blockade for symptomatic relief � Moderate to severe orbitopathy • Radioiodine uptake/scan shows very low • Could be made worse by radioactive percentage uptake - <5% iodine • Typical three phase response: � Suspicious “cold” nodule in the setting Hyperthyroidism, then hypo, then recovery of hyperthyroidism • 10% of patients go on to develop overt hypothyroidism Subacute Thyroiditis • Release of preformed hormone Em ai Print l • Frequently begins in setting of adjacent inflammation � URI or other viral illness • Self limited – typically lasts 6-12 weeks • May have thyroid tenderness Figure: 2009 uptodate 7
Amiodarone-induced Subclinical thyrotoxicosis Hyperthyroidism • Amiodarone is 33% iodine • Hypothyroidism is the more common result • Suppressed TSH with normal FreeT4 and FreeT3 • 2% of patients develop thyrotoxicosis � Dumping of stored hormone: thyroiditis • Etiology similar to overt hyperthyroidism • Lasts 2-6 months � More likely to be TMNG than Graves, • Treat with beta blockade, steroids however � Excess iodine load in Graves’ like • 40% remit within one year of diagnosis; picture rarely does this progress to thyrotoxicosis • Usually do see a goiter, family history • May respond to methimazole Amiodarone-induced Subclinical Hyperthyroidism thyrotoxicosis TSH low, FreeT4 And FreeT3 normal • Cannot use radioiodine scan for diagnosis • Cannot use I 131 for treatment TSH <0.1 TSH 0.1 – 0.4 • Thyroidectomy may be necessary Treat with ATDs Age >65 Age <65 � Not always the best surgical risk patients, though Risk of arrhythmia No cardiac disease Or fracture No bone disease • Endocrine consult definitely helpful! Observe 8
Elevated TSH levels Hypothyroidism 25 20 15 Jennifer Sipos, MD Percent of subjects 10 Men Assistant Professor Women 5 Division of Endocrinology 0 The Ohio State University 18- 25- 35- 45- 55- 65- > 74 24 34 44 54 64 74 Age ArchInternMed 2000;160:526-534 National Health and Nutrition TSH distribution by age in US Examination Surveys (NHANES III) • Survey of 13K people with no known Percent thyroid disease � 4.6% hypothyroid • 4.3% subclinical hypothyroidism • 0.3% overt hypothyroidism � 11% had elevated TPO Ab � 10% had elevated Tg Ab Upper TSH Concentration 9
Clinical Symptoms and Signs Associated Conditions • Fatigue • Hoarseness • Laboratory test abnormalities • Constipation • Goiter � Hypercholesterolemia • Impaired memory • Periorbital edema • Depression � Hyponatremia • Weight gain • Muscle weakness � Hyperprolactinemia • Nerve entrapment • Menstrual syndromes � Hyperhomocysteinemia disturbance • Bradycardia � Anemia • Infertility • Dry skin � CPK elevation • Cold intolerance Consequences of Hypothyroidism Percentage of patients with � Cholesterol When Mild & Overt hypothyroid symptoms 280 More 7.0 Abnormal TSH Level * * constipated Mean Total Cholesterol Level, Euthyroid 270 6.8 6.6 260 Feeling * P < 0.003 compared with euthyroid 6.4 colder 250 (mg/dL) Normal TSH * mmol/L 6.2 * Elevated TSH 240 6.0 * More tired * * 5.8 230 5.6 Slower 220 * 5.4 thinking 210 5.2 3 1 0 5 0 0 0 0 0 . . 1 1 2 4 6 8 8 0 5 - - - - - - > < - 1 0 5 0 0 0 0 5 10 15 20 25 3 200 . 1 1 2 4 6 . 5 0 > > > > > > TSH, mlU/L All differences reach statistical significance Ann Int Med 2000; 160: 526-534 Canaris GJ, et al. Arch Intern Med. 2000;160:526-534. 10
Medications affecting Radiological Abnormalities thyroid function Amiodarone Cholestyramine • • Lithium Ferrous Sulfate • • Interferon α , Interleukin 2 Omeprazole, lansoprazole • • Calcium carbonate • Dopamine, dobutamine • Glucocorticoids Phenobarbital • • Rifampin • � Pericardial effusion Estrogen Phenytoin • • � Pleural effusion Tamoxifen Carbamazepine • • Methadone � Pituitary enlargement • Causes of Hypothyroidism Treatment • T4 replacement • Hashimoto’s thyroiditis • Post-surgical � 1.6-1.8 mcg/kg (ideal body weight) • Radiation exposure � Elderly, CAD – 12.5 to 25mcg/day • Radioactive iodine • Check TFTs in 6-8 weeks • Drugs • Re-assess at 6 months • Central hypothyroidism • IV dose is 75-80% of PO • Iodine deficiency/excess Hashimoto Hakaru 11
Recommend
More recommend