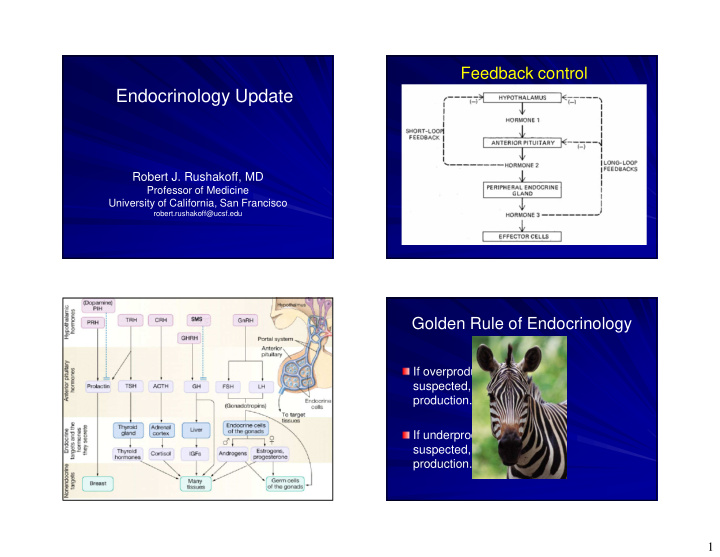


Feedback control Endocrinology Update Robert J. Rushakoff, MD Professor of Medicine University of California, San Francisco robert.rushakoff@ucsf.edu Golden Rule of Endocrinology If overproduction is suspected, try to suppress production. If underproduction is suspected, try to stimulate production. 1
Pituitary Hormones and Their Function Pituitary Hormones and Their Function Hormone Increased by Decreased by Excess Deficiency Notes Hormone Increased by Decreased by Excess Deficiency Notes ADH Thirst, high serum osmolality Low serum osmolality, SIADH DI ADH Thirst, high Low serum SIADH DI low serum K + serum osmolality osmolality, ACTH CRH, Stress High cortisol Cushing ’ s syndrome Adrenal insufficiency Diurnal variation (peak at 3 – 4 a.m.) low serum K + ACTH CRH, Stress High cortisol Cushing ’ s Adrenal Diurnal syndrome insufficiency variation (peak at 3 – 4 a.m.) TSH TRH High T 4 and/or Hyperthyroidism Hypothyroidism High T4 Hyper- Hypo- TSH TRH T 3 and/or T3 thyroidism thyroidism LH/FSH GnRH Gonadal sex Hypogonadism In men, inhibin steroids inhibits FSH GH GHRH, Somatostatin Childhood: Child: short hypoglycemia, gigantism stature dopamine Adulthood: Adult: poor sense LH/FSH GnRH Gonadal sex steroids Hypogonadism In men, inhibin inhibits FSH acromegaly of well-being Prolactin Pregnancy, Dopamine Galactorrhea, Inability to lactate Under tonic GH GHRH, hypoglycemia, Somatostatin Childhood: gigantism Child: short stature dopamine Adulthood: acromegaly Adult: poor sense of well-being nursing, TRH, hypogonadism inhibition by Prolactin Pregnancy, nursing, TRH, stress Dopamine Galactorrhea, hypogonadism Inability to lactate Under tonic inhibition by stress hypothalamic hypothalamic dopamine dopamine Pituitary Hormones and Their Function Pituitary Hormones and Their Function Hormone Increased by Decreased by Excess Deficiency Notes Hormone Increased by Decreased by Excess Deficiency Notes ADH Thirst, high serum osmolality Low serum osmolality, SIADH DI ADH Thirst, high serum osmolality Low serum osmolality, SIADH DI low serum K + low serum K + ACTH CRH, Stress High cortisol Cushing ’ s syndrome Adrenal insufficiency Diurnal variation (peak at 3 – 4 a.m.) TSH TRH High T 4 and/or T 3 Hyperthyroidism Hypothyroidism LH/FSH GnRH Gonadal sex steroids Hypogonadism In men, inhibin inhibits FSH Diurnal Cushing ’ s CRH, High Adrenal variation ACTH Stress cortisol syndrome insufficiency (peak at Child: short Childhood: 3 – 4 a.m.) GHRH, stature gigantism GH hypoglycemia, Somatostatin Adult: poor Adulthood: dopamine sense of well- acromegaly being TSH TRH High T 4 and/or T 3 Hyperthyroidism Hypothyroidism LH/FSH GnRH Gonadal sex steroids Hypogonadism In men, inhibin inhibits FSH GH GHRH, hypoglycemia, Somatostatin Childhood: gigantism Child: short stature dopamine Adulthood: acromegaly Adult: poor sense of well-being Prolactin Pregnancy, nursing, TRH, Dopamine Galactorrhea, hypogonadism Inability to lactate Under tonic inhibition by Prolactin Pregnancy, nursing, TRH, stress Dopamine Galactorrhea, hypogonadism Inability to lactate Under tonic inhibition by stress hypothalamic dopamine hypothalamic dopamine 2
Pituitary Hormones and Their Function - Hormone Increased by Decreased by Excess Deficiency Notes Hypothalamus ADH Thirst, high serum osmolality Low serum osmolality, SIADH DI low serum K + ACTH CRH, Stress High cortisol Cushing ’ s syndrome Adrenal insufficiency Diurnal variation (peak at 3 – 4 a.m.) - SOMATOSTATIN TSH TRH High T 4 and/or T 3 Hyperthyroidism Hypothyroidism TRH + LH/FSH GnRH Gonadal sex steroids Hypogonadism In men, inhibin inhibits FSH GH GHRH, hypoglycemia, Somatostatin Childhood: gigantism Child: short stature dopamine Adulthood: acromegaly Adult: poor sense of well-being - PIT TSH + Under tonic Pregnancy, Inability to Galactorrhea, inhibition by Prolactin nursing, TRH, Dopamine lactate hypogonadism hypothalamic stress dopamine T 4 T 3 Hormone Action Hormone Action Thyroid Failure Thyroid Thyroid TSH (+) ↑↑ TSH (+) PITUITARY PITUITARY (+) X T 4 , T 3 (-) T 4 , T 3 (-) T 4 , T 3 T 4 , T 3 (+) Thyroid Thyroid Hormone Hormone Action Action 3
Hormone Action Thyroid Function Tests Primary Hyperthyroidism � Total Thyroid Hormone � T 4 Thyroid ↓ ↓ TSH � T 3 PITUITARY (+) � Free Thyroid Hormone � direct and indirect measurement � FT 4, FT 3 ↑ T 4 , T 3 � Tests for Thyroid hormone binding protein ↑ T 4 , T 3 � T 3 U (-) � TBG Excess Thyroid Hormone Action Radioactive Iodine Uptake � 123 I given orally � Gamma counter over area of thyroid measures radioactivity at 24 hours TSH � Useful for differential diagnosis of thyrotoxicosis normal � NOT A TEST FOR ASSESSMENT OF THYROID FUNCTION � Dependent on iodine intake Primary Primary Euthyroid Hypothyroid Hyperthyroid 4
Thyroid Function and Oral Radioactive Iodine Scanning Contraceptives � Image of thyroid obtained after the administration of RAI Hyperthyroid Euthyroid � NOT A TEST FOR ASSESSMENT OF Serum T 4 THYROID FUNCTION � Useful for when thyrotoxic nodular disease T 3 Uptake is suspected. Free T 4 TSH Patient ASBP Patient SF Patient TDF FH + for mother with thyroid disease Medications: none Euthyroid Serum T 4 Exam: Thin female, hyperactive Pulse regular at 120. BP: 98/60 T 3 Uptake Anabolic HEENT: + stare, + lid lag Steroids TSH at 98mm measure 17mm bilat Free T 4 5
Patient SF Do you suspect that the patient Neck: thyroid enlarged 2X, beefy, no nodules has Heart: + Means-Lerman systolic scratch (rubbing together of normal pleural and hyperthyroidism? pericardial surfaces) Ext: fine tremor, no rash Symptoms of Hyperthyroidism Symptoms of Hyperthyroidism � Palpitations � Heat intolerance � Palpitations � Heat intolerance � nervousness � weight loss (with � nervousness � weight loss (with increased appetite) increased appetite) � fatigue � fatigue � Neck swelling � Neck swelling � hyperkinesia � hyperkinesia � Neck pain � Neck pain � hyperdefication � hyperdefication � Changes in eyes � Changes in eyes � sweating � sweating � decrease in menstrual � decrease in periods menstrual periods Patient SF 6
Signs of Hyperthyroidism � Tachycardia � Onycholysis (separation of the nail � Lid lag from its bed) � Stare � brisk reflexes � exophthalmus � Dermopathy (Graves’ disease) (thickened skin, most � Tremor often pretibial) � Thyroid enlargement 7
Is the patient thyrotoxic? FT 4 is 36 (nl 12-24) TSH is 0 (nl 0.5-5) Laboratory Tests for Laboratory Tests for Thyrotoxicosis Thyrotoxicosis TSH TSH Primary ? T 3 toxicosis FT 4 FT 4 thyrotoxicosis TSH TSH Secondary T 3 toxicosis FT 4 thyrotoxicosis FT 4 FT 3 8
Laboratory Tests Not Usually Causes of Thyrotoxicosis Needed for Diagnosis � Common Causes � Graves’ Disease autoimmune disease - B lymphocytes produce TSI Female:Male 5:1 � TSI Peak age 20-40 � Thyroid Antibodies � Toxic Multinodular Goiter (TMNG) � older patients with history of multinodular goiter � may be precipitated by iodine Causes of Thyrotoxicosis Causes of Thyrotoxicosis � Common Causes � Toxic Nodule (Plummer’s Nodule) � Less Common Causes Single autonomous nodule (>3cm) � Jod Basedow Age usually > 40 iodine induced (usually in patient with underlying goiter) � Silent Thyroiditis � Subacute thyroiditis � factitious � Young patient � excessive thyroid hormone ingested, usually for weight � history of malaise, neck pain, viral infection control � thyroid may be slightly large and tender � Most often someone in medical field 9
Causes of Thyrotoxicosis Tests for Differential Diagnosis � Less Common Causes TSH FT 4 24h RAI uptake � hypothalamic-pituitary Graves’ � post-partum Disease “postpartum depression” followed by hypothyroidism Subacute � molar pregnancy Thyroiditis high levels of hCG � Struma Ovarii Graves’ gland “beefy” teratoma of ovary containing thyroid tissue Thyroiditis gland hard ESR high in Subacute thyroiditis Tests for Differential Diagnosis Tests for Differential Diagnosis TSH FT 4 24h RAI uptake TSH FT 4 FT 3 24h RAI uptake Graves’ TMNG Disease Subacute Toxic Thyroiditis Nodule Graves’ gland “beefy” TMNG : feel a multinodular goiter, scan shows hot spots Thyroiditis gland hard Toxic nodule : palpate a single large nodule, scan shows single hot ESR high in Subacute thyroiditis spot 10
Graves’ Disease Treatment Antithyroid Drug Therapy � Best in young patients with small gland and mild disease Antithyroid Surgery � About 30% of patients have “remission” Drugs after 6 months to several years � >60% relapse Radioactive iodine Antithyroid Drug Therapy Antithyroid Drug Therapy � Propylthiouracil (PTU) 1. Start Tapazole 20-30 mg per day � Initail dose 150-200 mg tid 2. Start propranolol 20-40 mg tid and have patient � Methimazole (tapazole) titrate to maintain pulse 60-90. Large doses may be required. � Initial dose 20-30 mg qd � Side effects � rash in 5% - can often just treat with antihistamine 1. Follow FT 4 monthly lowering Tapazole to � agranulocytosis in <0.5% - patients told to stop drug maintain in normal FT 4 . TSH will remain suppressed for months and will not be useful. and get WBC if fever and sore throat 2. Titrate propranolol off as patient becomes euthyroid. 11
Recommend
More recommend