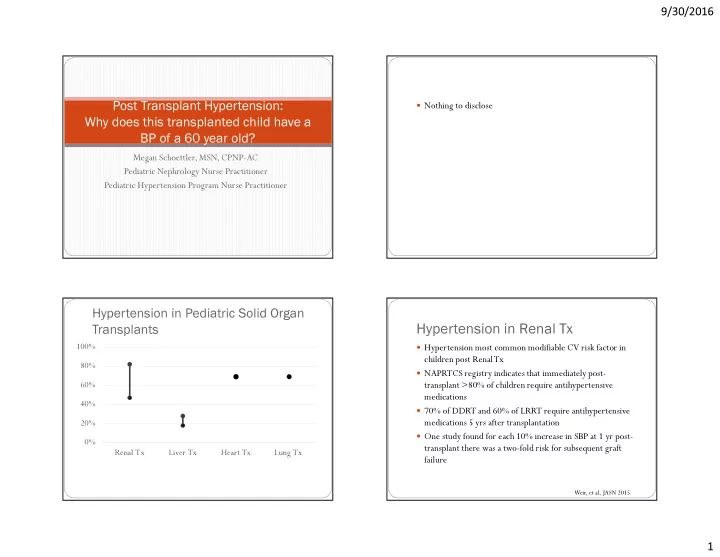
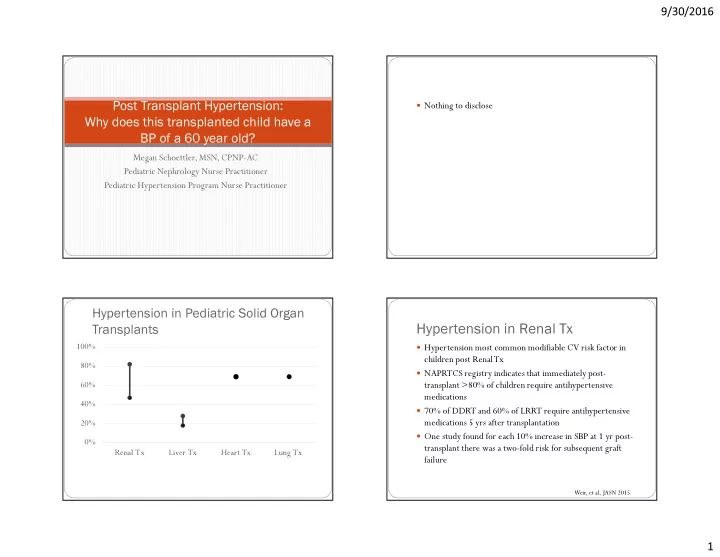
9/30/2016 � Nothing to disclose Post Transplant Hypertension: Why does this transplanted child have a BP of a 60 year old? Megan Schoettler, MSN, CPNP-AC Pediatric Nephrology Nurse Practitioner Pediatric Hypertension Program Nurse Practitioner Hypertension in Pediatric Solid Organ Hypertension in Renal Tx Transplants 100% � Hypertension most common modifiable CV risk factor in children post Renal Tx 80% � NAPRTCS registry indicates that immediately post- 60% transplant >80% of children require antihypertensive medications 40% � 70% of DDRT and 60% of LRRT require antihypertensive 20% medications 5 yrs after transplantation � One study found for each 10% increase in SBP at 1 yr post- 0% transplant there was a two-fold risk for subsequent graft Renal Tx Liver Tx Heart Tx Lung Tx failure Weir, et al, JASN 2015 1
9/30/2016 Hypertension in Liver Tx Hypertension in Heart Tx � ~40% of pediatric liver � Common, severe and occurs frequently at night transplant recipients � Associated with the number and type of immunosuppressive develop CKD post- agents used, specifically with the combo of Sirolimus and transplant Prednisone � ~25% are left with � Difficult to control, therefore advocating for alternative clinical hypertension interventions like decreased sodium intake � ABPM studies echo this at a 30% prevalence of masked hypertension Filler, PT, 2016 Roche, JHLT, 2008 Matloff, CGR, 2015 McLin et al, AJT, 2012 Hypertension in Lung Tx Pediatric Hypertension Definitions BP Classification BP Classification SBP and/or DBP Percentile SBP and/or DBP Percentile Within Total N with Total N with Within Total N with Within Outcome 5 Years known known 7 Years <90 th percentile <90 th percentile 1 Year known response Normal BP Normal BP response response 90 th percentile to <95 th percentile; 90 th percentile to <95 th percentile; Pre-Hypertension Pre-Hypertension 41.4% (N = 765) 67.7% (N = 229) – Hypertension adolescents BP >120/80 up to adolescents BP >120/80 up to <95th percentile <95th percentile Renal Dysfunction 9.4% (N = 795) 29.6% (N = 247) 42.8% (N = 138) 95 th percentile up to the 99 th 95 th percentile up to the 99 th Stage 1 hypertension Stage 1 hypertension Abnormal Creatinine ≤ 2.5 mg/dl 6.5% 23.1% 32.6% percentile plus 5 mm Hg percentile plus 5 mm Hg Creatinine > 2.5 mg/dl 1.9% 4.0% 6.5% >5 mm Hg above 99 th percentile >5 mm Hg above 99 th percentile Stage 2 hypertension Stage 2 hypertension 0.8% 1.6% 0.7% Chronic Dialysis Renal Transplant 0.3% 0.8% 2.9% 4 th Task Force Data, Pediatrics, 2004 2
9/30/2016 Ambulatory Blood Pressure Monitoring BP measurement standards � Measure BP in all children ≥3 years old or � Oscillometric measurement of BP <3 years old with chronic illness over a 24 hour period � Auscultation is preferred method � Daytime: every 20-30 min � Use appropriate BP cuff size � Nighttime: every 30-60 min � length should cover 80%-100% of the upper arm circumference � Standards are established for normals based on European � bladder width ≥ 40% of arm circumference pediatric patients ages 6-17 � High BP must be confirmed on repeated measurement � Results are expressed as Systolic and Diastolic Load � BP >90th percentile obtained by oscillometric device should be repeated by auscultation Ambulatory Blood Pressure ABPM classification Monitoring 3
9/30/2016 Hypertension in pediatric solid organ Masked Hypertension transplants � BP <95% in office setting but >95% by ABPM � Prevalence ~8% in unselected pediatric population � Prevalence in pediatric solid organ tx patients is ~26-46% � Associated with higher LV mass in children � Risk of LVH as high as in those with ambulatory HTN Tainio, JCH, 2015 Nocturnal Hypertension Hypertension across all transplants � Multifactorial: � Impaired renal function � BP should decrease 10-20% at night � Medication induced hypertension (Calcinurin-inhibition and � BP which does not decrease at night is considered non- corticosteroids) dipping with diagnosis of nocturnal hypertension � Fluid overload � Risk of LVH is equal to those with ambulatory HTN � Obesity � Hypertensive BP values can occur at night even in patients taking anti-hypertensive medications 4
9/30/2016 Impaired Renal Function Medication-induced hypertension � Renal perfusion compromised by hemodynamic instability, � Calcinurin inhibitors causes vasoconstriction of the afferent hypotension and prolonged cross-clamp time can lead to and efferent glomerular arterioles, reduction in renal blood ischemia and AKI flow and thereby decreased GFR � Repeated episodes of AKI, regardless of interim return to � Impairment of endothelial cell function leads to reduced baseline function, are associated with impaired renal function production of vasodilators and enhanced release of and progression to CKD vasoconstrictors � hypertension is a hallmark of CKD and is independently � Sodium retention and sensitivity is related to afferent associated with CKD progression glomerular arteriole vasoconstriction and activation of sodium chloride co-transporter � Strict BP control can substantially slow CKD progression Matloff, CGR, 2015 Choice of Antihypertensive Drug Based on Likely Etiology Classes of Antihypertensive Drugs � Diuretics � Fluid overload, steroid therapy Diuretics � Direct acting vasodilators � Renal injury/scarring ACE I, ARB � Hydralazine, minoxidil, nitroprusside � Sympathetic blockers � Renal artery stenosis ACE I, ARB � Central: clonidine � CSA, Prograf Calcium channel blockers � β receptor: propranolol, metoprolol � CNS disease Clonidine � α and β receptor: labetalol � Angiotensin blockade � Adolescents Once daily therapy � ACE I: enalapril, benazapril � ARB: candesartan � Calcium channel blockers � Nifedipine, amlodipine, nicardipine 5
Recommend
More recommend