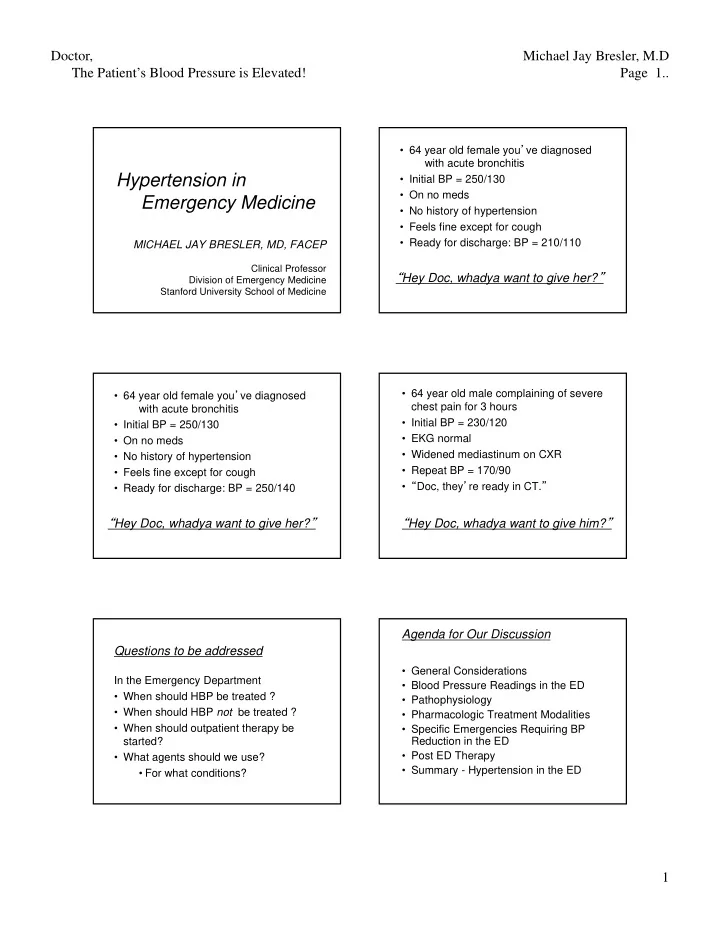
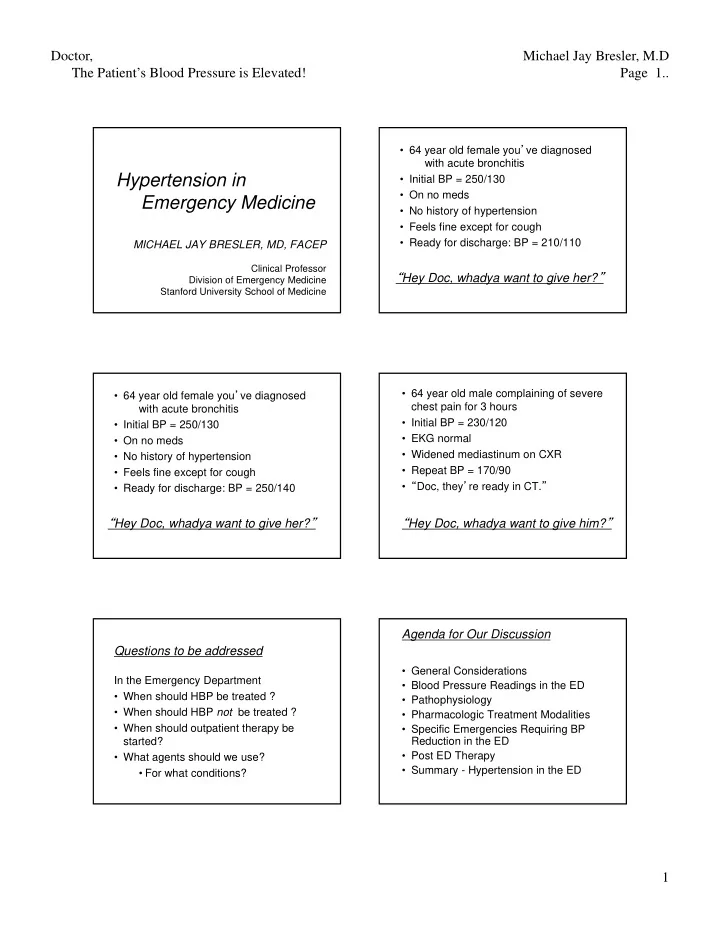
Doctor, Michael Jay Bresler, M.D The Patient’s Blood Pressure is Elevated! Page 1.. • 64 year old female you ’ ve diagnosed with acute bronchitis Hypertension in • Initial BP = 250/130 • On no meds Emergency Medicine • No history of hypertension • Feels fine except for cough • Ready for discharge: BP = 210/110 MICHAEL JAY BRESLER, MD, FACEP Clinical Professor “ Hey Doc, whadya want to give her? ” Division of Emergency Medicine Stanford University School of Medicine • 64 year old male complaining of severe • 64 year old female you ’ ve diagnosed chest pain for 3 hours with acute bronchitis • Initial BP = 230/120 • Initial BP = 250/130 • EKG normal • On no meds • Widened mediastinum on CXR • No history of hypertension • Repeat BP = 170/90 • Feels fine except for cough • “ Doc, they ’ re ready in CT. ” • Ready for discharge: BP = 250/140 “ Hey Doc, whadya want to give her? ” “ Hey Doc, whadya want to give him? ” Agenda for Our Discussion Questions to be addressed • General Considerations In the Emergency Department • Blood Pressure Readings in the ED • When should HBP be treated ? • Pathophysiology • When should HBP not be treated ? • Pharmacologic Treatment Modalities • When should outpatient therapy be • Specific Emergencies Requiring BP started? Reduction in the ED • Post ED Therapy • What agents should we use? • Summary - Hypertension in the ED • For what conditions? 1
Doctor, Michael Jay Bresler, M.D The Patient’s Blood Pressure is Elevated! Page 2.. • I will use primarily generic names • But I will also include on the slides the brand names since these are most I have no financial relationship commonly used in the real world - where we practice with any drug company • When there are several brand names I will try to include them all • I have no idea which companies make which drugs What is Normal Blood Pressure ?? Prehypertension General 130-139/80-90 Considerations • Compared with normal BP –Double the risk for developing hypertension. • Lifestyle & diet intervention warranted Joint National Committee on Hypertension,2003 Incidence of Hypertension in U.S.A. Scope of the Problem • Normotensive people at age 55 have a • > 140/90 (HTN) 90% lifetime risk of developing HTN –27% of adults ( Ref: Vasan) • > 130/90 (pre HTN + HTN) • Between age 40-70, the risk of –60% of adults! cardiovascular disease doubles for every (independent variables) –88% > 60 years old –20 mm Hg systolic above 115 –40% ages 18-39 !! –10 mm Hg diastolic above 70 Wang Arch Intern Med 2004 »Lewington Lancet 2002 2
Doctor, Michael Jay Bresler, M.D The Patient’s Blood Pressure is Elevated! Page 3.. Should BP Rise with Age? BP and Gender • Estrogens protect NO !! • After menopause, women catch up with men and eventually surpass In societies with natural diet, less salt, and the men less obesity, more exercise (in blood pressure that is….) –BP does not rise with age • Diet is a particular problem - –We love our unhealthy diet! BP and Ethnicity High Blood Pressure Readings in • Incidence of HTN the Emergency Department – 1.5 - 2 x more common in Blacks • 1 in 3 African Americans • 1 in 4-5 Caucasian and Hispanic Americans • ? Asians • African Americans – HTN begins earlier – More end organ damage – ACEI ’ s & ARB ’ s less effective Is that reading real? Question • Asymptomatic E.D. patients with BP >140/90 – BP at home bid – > 1/2 continued >140/90 Are ED BP readings – Most of rest continued at pre-hypertensive level accurate & reliable for – Independent of pain or anxiety in E.D. » Tanabe Ann Emerg Med 2008 screening asymptomatic patients for HTN? • E.D. patients with BP >140/90 followed in clinic – 54% continued >140/90 » Cline Acad Emerg Med 2000 3
Doctor, Michael Jay Bresler, M.D The Patient’s Blood Pressure is Elevated! Page 4.. ACEP Clinical Policy Question • Level B Recommendation –If SBP persistently > 140 or Do asymptomatic –If DPB persistently > 90 patients with elevated BP Refer for follow up of possible HTN benefit from rapid and BP management lowering of their BP? Ann Emerg Med. 2006;47:237-249 ACEP Clinical Policy HBP in the ED • Level B Recommendation –Initiating Tx in the ED is not necessary • Most useful terminology if F/U is available –Hypertensive Emergency –Rapid lowering of BP is not necessary and may be harmful –Hypertensive Urgency –When Tx is initiated, BP should be –Elevated Blood Pressure lowered gradually and should not be expected to be normalized during the ED visit Why is this the most useful classification? Ann Emerg Med. 2006;47:237-249 HBP in the ED Hypertensive Emergency • Hypertensive Emergency • By definition – Treated in ED with IV meds – Evidence of acute end organ damage • Hypertensive Urgency – Usually brain, heart, or kidney – May be treated in ED - oral meds OK • Definition implies that organ dysfunction – Usually give prescription is caused by acute HPB, rather than • Elevated Blood Pressure vice versa – Not treated in ED • Systolic usually > 220 – May or may not give prescription • Diastolic usually > 130 – We should refer for further evaluation 4
Doctor, Michael Jay Bresler, M.D The Patient’s Blood Pressure is Elevated! Page 5.. Hypertensive “ Urgency ” Hypertensive Urgency • Major elevation of BP • Treatment may be administered in the ED if BP remains very elevated (roughly in range of >220/>120) but –Controversial –Without evidence of acute organ failure –Trend toward not treating in the ED –No acute symptoms directly • Outpatient treatment should generally attributable to elevated BP be initiated, however • Basic studies may be indicated Diagnostic Studies in the ED • Incidental finding of moderate HBP –ED workup not necessarily indicated -> refer Pathophysiology • If initiating outpatient treatment –Basic studies in ED may be considered of Hypertension –CBC, lytes, renal, glucose, UA, EKG • If ED treatment required –Basic studies usually indicated • If hypertensive emergency - basic plus –Studies specific to disorder (CT, etc.) Regulation of Blood Pressure Inherent stiffness of arterial wall A Balance Between Cardiovascular risk factors lead to: • Replacement of elastin in arterial walls by collagen and fibrous tissue-> • Inherent stiffness of the arterial wall – Decreased compliance – Increased resistance • Vasodilation • Vasoconstriction • Endothelial dysfunction 5
Doctor, Michael Jay Bresler, M.D The Patient’s Blood Pressure is Elevated! Page 6.. Pathophysiology Acute Regulation of BP BP --> Endothelial wall stretch/stress BP --> Endothelial wall stretch/stress • Vasodilation –Beta-2 adrenergic innervation –Nitric oxide c-AMP Endothelial Dysfunction Endothelial Dysfunction • Vasoconstriction Capillary permeability Capillary permeability –Alpha-1 adrenergic innervation Depletion of NO Depletion of NO –Circulating catecholamines Inflammation Inflammation –Angiotensin II Renin-Angiotensin-Aldosterone Renin-Angiotensin-Aldosterone Angiotensin II Angiotensinogen • Powerful vasoconstrictor Renin • Release of aldosterone • Inflammatory response Angiotensin I • Hypertrophy of smooth muscle cells ACE • Decreased nitric oxide -> Angiotensin II further vasoconstriction Autoregulation and Hypertensive Crisis Organ-specific autoregulation Auto-Regulation and • Normally maintains capillary pressure Hypertensive Crisis & flow within an acceptable range –Increased systemic BP -> vasoconstriction –Decreased systemic BP -> vasodilation 6
Doctor, Michael Jay Bresler, M.D The Patient’s Blood Pressure is Elevated! Page 7.. Cerebral Autoregulation, Hypertension, Autoregulation of Cerebral Blood Flow and Excessive Correction • Cerebral arterial resistance varies directly Hypertensive with BP to maintain cerebral perfusion within Person acceptable limits • “ Set point ” rises with chronic HBP • Rapid ED reduction of BP may drop CPF Normotensive below adequate level Person • Lower BP gently, • And usually never < 110 diastolic – Except • with aortic dissection Mean Arterial Pressure Adapted from Elliott:Crit Care Clin 2001;17:435 Pharmacologic Treatment Autoregulation and Hypertensive Crisis Modalities Hypertensive crisis Autoregulation fails -> Endothelial dysfunction • Capillary permeability & edema • Inflammatory response • Prothrombotic response • Decreased nitric oxide Cell necrosis • Release of vasoconstrictors Pharmacologic Treatment Modalities • Parenteral Vasodilators • Beta Blockers Parenteral • Calcium Channel Blockers • Angiotensin Converting Enzyme Inhibitors Vasodilators • Angiotensin II Receptor Blockers • Direct Renin Inhibitors • Diuretics • Others 7
Recommend
More recommend