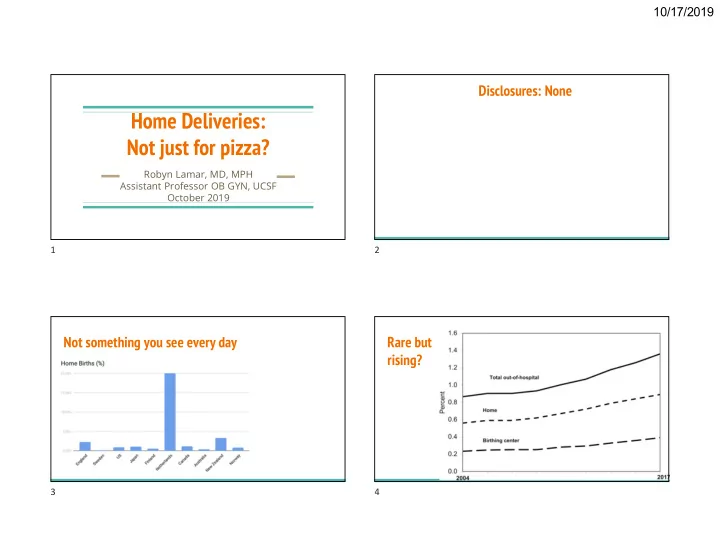
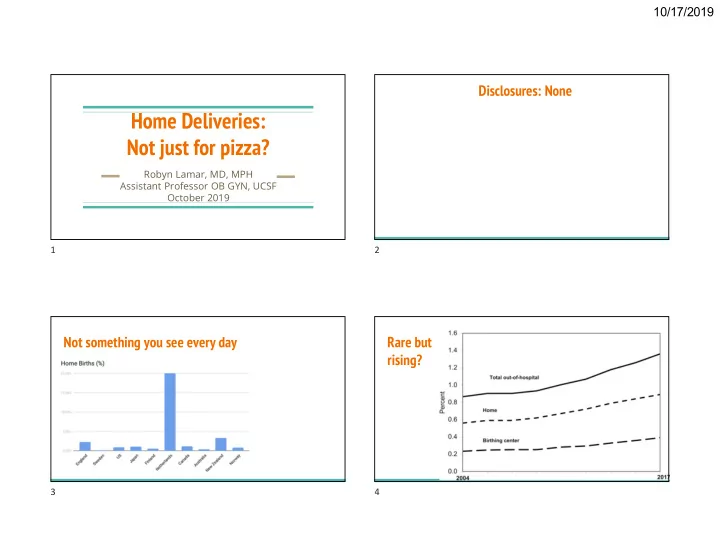
10/17/2019 Disclosures: None Home Deliveries: Not just for pizza? Robyn Lamar, MD, MPH Assistant Professor OB GYN, UCSF October 2019 1 2 Not something you see every day Rare but rising? 3 4 1
10/17/2019 LIstening to Mothers in California, 2017 survey What does the Evidence Tell US? Why do some women choose home birth? How do they fare? How do their children fare? What factors are critical for safe maternity care? 5 6 But first: What exactly is home birth like? Planned Home Birth Basics Most attended by midwives ● Comprehensive prenatal care, including ultrasound, is the norm ● Intermittent fetal monitoring is standard ● GBS prophylaxis can be administered ● Midwives bring supplies including emergency medications for ● hemorrhage, oxygen tank, IV supplies, etc ACNM ( & SF community) standard is for two providers with current NRP ● and CPR training to attend the birth Lidocaine, suturing available if needed ● Vitamin K, erythromycin can be given ● 7 8 2
10/17/2019 Part I: What Women Want Women increasingly desire fewer medical interventions in childbirth 9 10 But intervention rates have risen Many women feel pressured to have interventions 11 12 3
10/17/2019 1 in 12 So why do women choose home birth? women [hint: not about glamor] experiences harsh treatment during childbirth And rates 13 14 Which factors do women cite as most important? Which factors do women cite as most important? #2: Control & #1: Previous negative experiences with hospital care Empowerment 1. Conflicts between a woman’s belief birth is a natural 1. “I feel competent to make process, and the experience of interventions of decisions for myself” questionable utility 2. “I want control over the 2. Difficulty handling multiple interruptions, meeting things that are done to my multiple strangers body” 3. Unhappiness with care perceived as disrespectful 15 16 4
10/17/2019 Which factors do women cite as most important? How do women choosing home birth rate their care? #3: Benefits of the home environment The literature is sparse 1. Comfortable, peaceful, quiet, familiar In the small studies that have looked at this: 2. Support people are invited--changes the power ● Women report very high satisfaction with their care dynamic ● This remains true even in the subset requiring intrapartum transfer of care, when compared to women planning hospital birth who require escalation of intrapartum care 17 18 Part II: Safety Methodological Challenges Outcomes RCT not feasible ● Multiple challenges in observational studies ● Selection bias ○ Misclassification (especially planned versus unplanned home births) ○ Choosing the best comparison group ○ Identifying & controlling for all relevant confounders ○ Health systems differences make international comparisons challenging ● Training & experience of home birth providers ○ Established criteria for home birth ○ Integration of health system ○ Transport/physical distances ○ 19 20 5
10/17/2019 How do mothers fare who Findings are consistent: they fare better plan a home birth? ● Lower rate of cesarean OR 0.35 (0.27-0.46) ● Lower rate of op vaginal delivery OR 0.37 (0.24-0.58) ● Lower rate of severe perineal trauma OR 0.57 (0.40-0.81) ● Lower rate of PPH > 1000ml OR 0.55 (0.55-0.96) 21 22 Name, year Country Study Design N home N hospital Quality What Studies tell us this? Birthplace in England UK Prospective cohort 16,810 19,706 High 2011 Blix 2012 Norway Retrospective cohort 1,631 16,310 High Bolten 2016 Netherlands Prospective cohort 2,050 1,445 High Davis 2011 New Zealand Comparative descriptive 1,830 11,503 High Haldansdottir 2015 Iceland Retrospective matched 307 921 High cohort Hiraizumi 2013 Japan Retrospective cohort 168 340 Moderate Homer 2014 Australia Retrospective population- 742 242,936 High based cohort Miller 2012 New Zealand Retrospective matched 109 116 Moderate cohort Wiegerinck 2015 Netherlands Retrospective cohort 23,323 29,306 Moderate 23 24 6
10/17/2019 Birthplace in England Birthplace in England: Key Takeaways for Mothers aOR ( 99 % CI) Inclusion criteria: ● “Healthy women with low risk pregnancies,” defined before labor ○ Op Vag 0.43 (0.32-0.57) Attended by an NHS midwife at onset of labor ○ 37 weeks, singleton, live at onset of labor ○ C/s 0.31 (0.23-0.41) Sample: prospective cohort from all NHS trusts providing intrapartum ● care at home + a stratified random sample of obstetric units, 2008-2010 Exposure: planned place of birth at the start of labor Epis 0.33 (0.28-0.39) ● Analysis: by intention to treat ● Outcomes ● 3rd/4th 0.77 (0.57-1.05) Primary: composite of perinatal mortality + specific morbidities ○ Secondary: maternal morbidities, interventions, and mode of birth ○ Transfusion 0.72 (0.47-1.12) Planned subgroup analysis by parity ○ 25 26 What about US Data? Snowden et al, 2015 ● Inclusion criteria: cephalic, singleton, term, nonanomalous ● Sample: population-based, retrospective cohort study of all births that occurred in Oregon during 2012 and 2013 ● Exposure: planned place of birth from birth certificate ● Analysis: by intention to treat ● Outcomes ○ Perinatal mortality and morbidity (low apgars, seizure, ventilator support, NICU admit) ○ Maternal morbidity, interventions, and mode of birth 27 28 7
10/17/2019 Snowden: Key takeaways for Mothers How do babies fare in planned home birth? aOR ( 95 % CI) Op Vag 0.24 (0.17-0.34) C/s 0.18 (0.16-0.22) ICU Admit 1.00 (0.31-3.21) 3rd/4th 0.69 (0.49-0.98) Transfusion 1.91 (1.25-2.93) 29 30 How do babies fare in planned home birth? How do babies fare? US data Findings are split depending on the study type: ● Historic data challenges due to: ○ Fractured health care system ● Registry-based data (mostly from other countries) ○ Birth certificates didn’t Most show no differences in stillbirth, early indicate planned place of neonatal death, or NICU admission birth ● Two more recent studies using ● US Birth Certificate data new birth certificate data show: Higher risk of stillbirth, early neonatal death, ○ Higher perinatal mortality seizures, and NICU admission ○ Higher neonatal morbidity 31 32 8
10/17/2019 Snowden: Key Takeaways for Babies Grunebaum et al, 2016 aOR (99% CI) Inclusion criteria: singleton, term, nonanomalous with birthweight >2.5kg ● Sample: population-based, retrospective cohort study of all births 2009- ● Perinatal death 2.43 (1.37 to 4.30) 2013 in states that used the 2003 revised birth certificate Exposure: planned place of birth as indicated on birth certificate ● Apgar <4 1.75 (1.07-2.86) Outcome: neonatal death (liveborn infant who dies before day 28 of life) ● at 5 minutes Analysis by individual risk factors ● Parity NICU admit in 0.71 (0.55 to 0.92) ○ first week Maternal age ○ Gestational age ○ Neonatal 3.60 (1.36 to 9.50) Presentation ○ seizure Prior cesarean ○ 33 34 Grunebaum: Key Takeaways for Babies How do babies fare? Registry-based data Findings are largely consistent across studies in multiple countries and a variety of study designs: babies fare well ● Same low rate of stillbirth OR 0.94(0.76-1.17) ● Same low rate of neonatal death OR 1.00 (0.78-1.27) ● Fewer NICU admissions OR 0.71 (0.55-0.92) 35 36 9
10/17/2019 Scarf et al: Systematic review & meta-analysis 2018 De Jonge 2015: Key Takeaways for Babies Name, year Country Study Design N home N hospital Quality aOR ( 99 % CI) Nullip Multip Birthplace in England UK Prospective cohort 16,810 19,706 High 2011 Blix 2012 Norway Retrospective cohort 1,631 16,310 High Perinatal death 0.99 (0.79– 1.16 (0.87– 1.24) 1.55) Burns 2012 UK Prospective cohort 2,964 4,130 High Apgar <4 0.87 (0.71– 0.92 (0.70– Davis 2011 New Zealand Comparative descriptive 1,830 11,503 High at 5 minutes 1.07) 1.20) De Jonge 2015 Netherlands Retrospective cohort 466,122 276,958 High NICU admit in 1.04 (0.91– 0.74 (0.62– first week 1.18) 0.87) Haldansdottir 2015 Iceland Retrospective matched 307 921 High cohort Serious adverse 0.93 (0.84– 0.76 (0.66– Homer 2014 Australia Retrospective population- 742 242,936 High outcome* 1.04) 0.87) based cohort 37 38 Birthplace in England: Key Takeaways for Babies Hutton et al 2016 aOR (99% CI) Inclusion criteria: ● Prenatal care booked with registered midwife in Ontario ○ All 1.16 (0.76-1.77) No more than 1 prior cesarean ○ Sample: retrospective cohort of all such pregnancies planning home birth ● Nullips 1.75 (1.07-2.86) at start of labor, matched for parity and prior c/s to low risk group planning hospital birth 2006-2009 (N = 11, 493 in each group) Exposure: planned place of birth at the start of labor ● Multips 0.72 (0.41-1.27) Analysis: by intention to treat ● Outcomes ● Composite outcome includes: Primary: composite of perinatal death, 5 min Apgar < 4; chest compression; PPV ○ Stillbirth, early neonatal death, Secondary: intrapartum intervention, mode of delivery, maternal morbidity ○ HIE, mec aspiration syndrome, brachial plexus injury, fractured humerus or clavicle 39 40 10
Recommend
More recommend