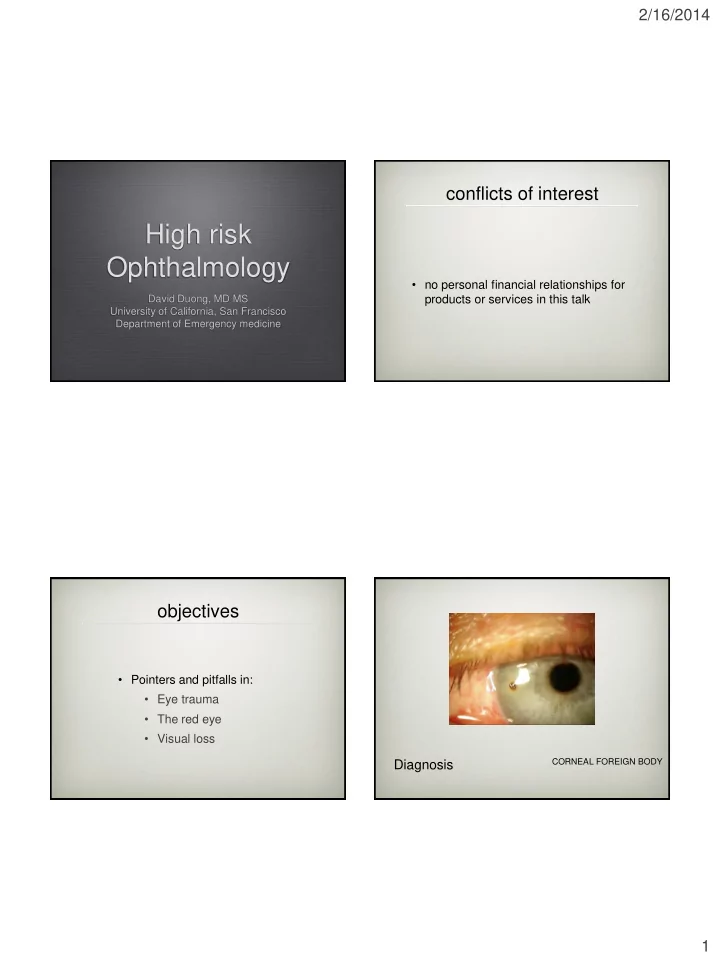
2/16/2014 conflicts of interest High risk Ophthalmology • no personal financial relationships for David Duong, MD MS products or services in this talk University of California, San Francisco Department of Emergency medicine objectives • Pointers and pitfalls in: • Eye trauma • The red eye • Visual loss CORNEAL FOREIGN BODY Diagnosis 1
2/16/2014 Pearls for Rust Rings • Rust Rings do not have to be removed QuickTime™ and a decompressor immediately are needed to see this picture. • Removal is often easier 1-2 days after the injury and with a corneal drill • Homatropine can help with ciliary spasm foreign body removal • Arrange follow-up in 1-2 days after removal Can J Rural Med 2013 QuickTime™ and a decompressor are needed to see this picture. everting the lid 2
2/16/2014 corneal Foreign Body pitfalls • Not everting the lid • Not considering an intraocular FB • Not considering corneal laceration subtarsal foreign body ophtho or plastics need to be involved for lacerations involving the: tarsal plate lid margin nasolacrimal system ALL OF THEM anatomy high risk lacerations? 3
2/16/2014 eyelid laceration pitfalls so get Va, assess EOM, RAPD, etc. Va helps to risk stratify for eye emergencies • Not assuming there are other ocular injuries • Not obtaining visual acuity canalicular laceration EM Clin NA. 2008 globe rupture • decreased Va • RAPD • eccentric pupil • bullous subconjunctival hemorrhage • extrusion of vitreous Globe rupture • hyphema • Seidel test 4
2/16/2014 key actions globe rupture • Consult ophthalmology and order CT QuickTime™ and a decompressor • Protect the eye (eye shield, avoid eye are needed to see this picture. manipulation) • Avoid ocular extrusion (antiemetics, pain meds, sedation) • Antibiotic prophylaxis • Tetanus prophylaxis seidel test HYPHEMA TREATMENT good prognosis microhyphema eye shield HOB >30 deg cycloplegia <33% (Grade 1) 90% visual acuity prognosis 20/50 or better. ophtho referral HOB >30 deg to prevent synechiae cycloplegia only if no incr IOP referral to monitor for incr IOP and rebleeding within 5 days. no NSAIDS HYPHEMA Diagnosis 33-50% (Grade 2) 5
2/16/2014 HYPHEMA HYPHEMA TREATMENT PITFALLS ophtho consult >50% (Grade 3 & 4) eye shield • Not obtaining an IOP or asking about HOB >30 deg topical B-blocker if increased sickle cell disease or trait IOP. ↑ IOP (>24) c/s may also recommend • Discharging with NSAIDs steroid drops no NSAIDS • Neglecting close ophthalmology follow- up • Not considering globe rupture or IOFB sickle cell case of red eye The Red Eye • 52-yo F with 1 day of severe right eye pain, and decreased vision. On exam, you see corneal cloudiness and diffuse conjunctival injection with ciliary flush. 6
2/16/2014 medical treatment of acute angle glaucoma • How do you use the drops? • How many times can you repeat the drops? • What about acetazolamide and mannitol? medical treatment of acute medical treatment of acute angle glaucoma angle glaucoma • Give separate eye drops 1 minute apart • Goal IOP is 35 mmHg or >25% (timolol, apraclonidine, prednisolone, presenting IOP pilocarpine are acceptable) • Consider mannitol IV if IOP is still high • Give acetazolamide PO early • Call ophthalmology again • Repeat drops once in 15 minutes Choong et al. Eye. 1999 7
2/16/2014 QuickTime™ and a decompressor vision loss are needed to see this picture. floaters Hollands et al. JAMA 2009 approach to floaters and flashes • Bottom line is to determine when to PVD can lead to retinal tears refer a vision threatening condition to 14% prevalence 33-46% of retinal tears lead prevent further vision loss or restore to retinal detachment vision Hollands et al. JAMA 2009 8
2/16/2014 discuss evidence behind JAMA meta-analysis subjective visual acuity recommendations from the JAMA paper worse vision 45% probability of retinal tear • floaters vs flashes vs both is not baseline 14% diagnostically helpful for retinal tear prevalence of • older age (>60) is not associated with retinal tear in those with increased risk of retinal tear; younger PVD age is not less likely to have retinal tear 9% probability of no change retinal tear Hollands et al. JAMA 2009 vitreous hemorrhage or pigment Key actions need pictures or videos or vitreous hemorrhage and pigment - assess via slit lamp or direct ophthalmoscopy (Shafer’s or Shaffer’s sign) vitreous hemorrhage root atlas has a video of retinal detachment LR = 10 62% probability of retinal tear • Assess subjective visual acuity baseline 14% besides allergy and glaucoma - there is no absolute prevalence of contraindication for pupillary • Assess visual acuity and peripheral dilation for a good exam. retinal tear in 1 gtt tropicamde + 1 gtt phenylephrine and wait 20 vision minutes those with • Fundiscopic exam +/- slit lamp PVD 88% probability vitreous pigment of retinal tear LR = 44 9
2/16/2014 pitfalls in the case of floaters and flashes Case of vision loss • Not referring to ophthalmology with only subjective visual acuity loss • 72-yo F with sudden painless, decreased left eye vision 2 hours. Va OS = cannot read the eye chart or • Not giving return precautions with a count fingers, but can see hand motion. PVD diagnosis (more floaters or vision reduction) key actions CRAO • Rule-out temporal arteritis (including ESR & CRP) • Consider ocular massage (within 24 hrs) • Ophtho consult (to consider AC paracentesis or thrombolytics) CENTRAL RETINAL Diagnosis ARTERY OCCLUSION Fraser et al. Cochrane review. 2009 10
2/16/2014 pitfalls CRAO Case of vision loss • Failing to consider embolic source of • 38-yo F with decreased left eye vision CRAO for 2d with mild eye pain. She has • ECG for AFib decreased Va, a + RAPD on the left, and swollen optic disc. nl slit lamp • carotid imaging exam. • cardiac evaluation key actions optic neuritis QuickTime™ and a decompressor are needed to see this picture. • Neurology consult for MS and NMO ONTT - 457 patients with optic neuritis IV methylprednisolone was associated with faster recovery in visual fxn and a work-up lower 2-year risk of development of multiple sclerosis. but did not affect long term outcome • Consider MRI with gadolinium Oral prednisone was associated with an increased incidence of recurrent optic neuritis and did not improve visual outcomes compared to placebo • Consider IV steroids relative afferent pupillary defect Beck et al. NEJM. 1993 Cochrane. 2012 11
2/16/2014 summary www.rootatlas.com • Key Actions and Pitfalls in: • Eye trauma podcasts@ucsf • The red eye • Vision loss thank you for your particular thanks to those attention who gave consent to be photographed for david.duong@emergency.ucsf.edu educational purposes 12
2/16/2014 CORNEAL ABRASION pediatrics PITFALL Video of a baby crying before this slide? • CORNEAL ABRASIONS • Return precautions • antibiotic ointments lubricate • RED FLAG: persistent pain or • consider 1 drop of cycloplegia unwillingness or open the eye after 1 day of treatment • consider codeine elixir pediatric Eye trauma PITFALL pediatric vision testing • Consider sedation to fully evaluate the • Pediatric Eye Chart eye • Fix and Follow (F/F) • Ketamine: total dose <3mg/kg does not • Blink to Light (BTL) raise IOP Nagdeve. J Ped Ophth Strab. 2006 13
2/16/2014 QuickTime™ and a QuickTime™ and a decompressor decompressor are needed to see this picture. are needed to see this picture. Can start to fix and follow at 2 months fixation target Fix and follow References • 1. Magauran. Emerg Med Clin N Am. 2008; 26; 23. QuickTime™ and a • 2. Carley. Emerg Med J. 2001; 18: 273. decompressor are needed to see this picture. • 3. Guess S et al. Ocul Surf. 2007; 5(3): 240. • 4. Choong YF et al. Eye. 1999; 13: 613 • 5. Hollands et al. JAMA. 2009; 302(20): 2243. • 6. Germann et al. AJEM. 2007; 25: 834. • 7. Fraser et al. Cochrane Database of systematic reviews. 2009. • 8. Mohamed et al. Ophthalmology. 2007; 114(3):507. • 9. Nagdeve et al. J Ped Ophth Strab. 2006; 43(4):219. • 10. Brock G et al. Can J Rural Med. 2013; 18(4) • 11. Gharaibeh A et al. Cochrane Database of systematic reviews. 2013. cells and flare • 12. Halstead SM et al. Acad EM. 2012; 19:1145-1150 • 13. Gal RL et al. Cochrane Database of systematic reviews. 2012. 14
Recommend
More recommend