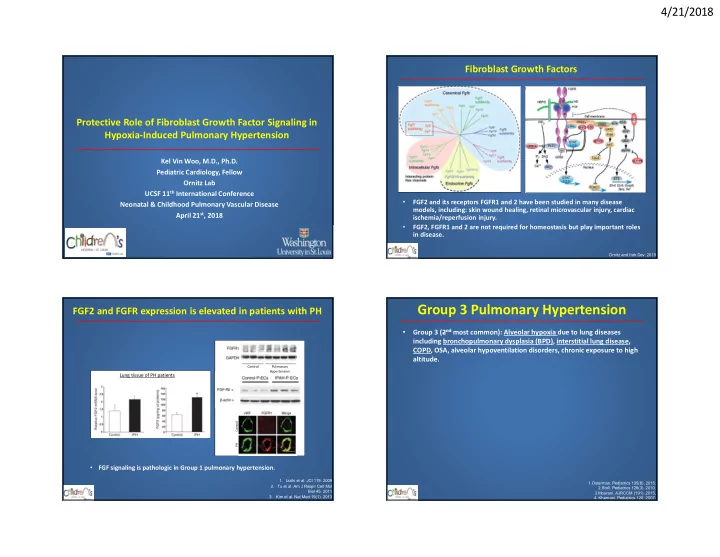
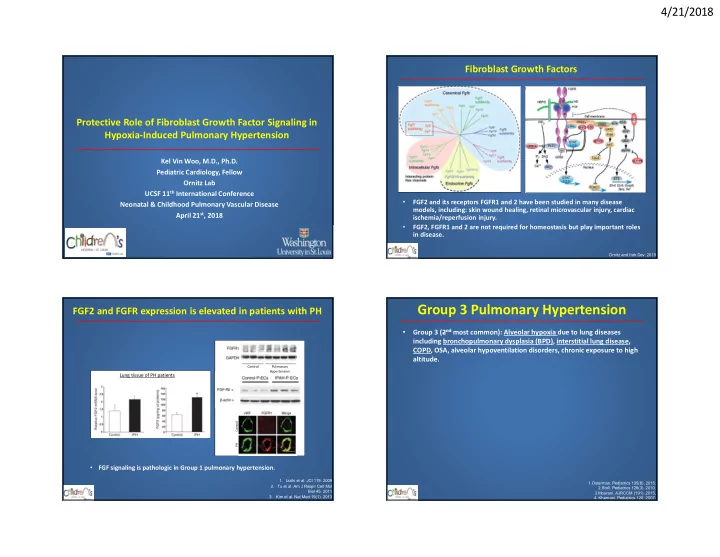
4/21/2018 Fibroblast Growth Factors Protective Role of Fibroblast Growth Factor Signaling in Hypoxia-Induced Pulmonary Hypertension Kel Vin Woo, M.D., Ph.D. Pediatric Cardiology, Fellow Ornitz Lab UCSF 11 th International Conference • FGF2 and its receptors FGFR1 and 2 have been studied in many disease Neonatal & Childhood Pulmonary Vascular Disease models, including: skin wound healing, retinal microvascular injury, cardiac April 21 st , 2018 ischemia/reperfusion injury. • FGF2, FGFR1 and 2 are not required for homeostasis but play important roles in disease. Ornitz and Itoh.Dev. 2015 Group 3 Pulmonary Hypertension FGF2 and FGFR expression is elevated in patients with PH Group 3 (2 nd most common): Alveolar hypoxia due to lung diseases • including bronchopulmonary dysplasia (BPD), interstitial lung disease, COPD, OSA, alveolar hypoventilation disorders, chronic exposure to high altitude. Control Pulmonary Hypertension Lung tissue of PH patients Control PH • FGF signaling is pathologic in Group 1 pulmonary hypertension. 1. Izziki et al. JCI 119. 2009 1.Osterman. Pediatrics 135(6). 2015. 2. Tu et al. Am J Respir Cell Mol 2.Stoll. Pediatrics 126(3). 2010. Biol 45. 2011 3.Mourani. AJRCCM (191). 2015. 3. Kim et al. Nat Med 19(1). 2013 4. Khemani. Pediatrics 120. 2007. 1
4/21/2018 Why we need to study Group 3 PH Group 3 Pulmonary Hypertension Group 3 (2 nd most common): Alveolar hypoxia due to lung diseases • Majority of studies to date have focused on Group 1 PH. • including bronchopulmonary dysplasia (BPD), interstitial lung disease, • All 3 classes of PH drugs are targeted toward Group 1. COPD, OSA, alveolar hypoventilation disorders, chronic exposure to high • Randomized clinical trials show failure of current PH altitude. therapies in Group 3 PH patients: • 550,000 premature infants are born in the United States annually. 1 1) Bayer. 2016: RCT, Riociguat, increased adverse events and mortality • Up to 60% of premature infants develop BPD. 2 2) Raghu et al. 2013: RCT, Ambrisentan, patients with PH had no change in • 29-42% of infants with BPD go on to develop PH. 3 time to disease progression • Infants with BPD and PH have a 2-year mortality of 33-48%. 4 3) Krowka et al. 2007: inh. Iloprost, no difference in 6MWT, NYHA class, dyspnea score, exercise O2sat 4) Jackson et al. 2010: Sildenafil, no difference in 6MWT 5) Zisman et al. 2010: Sildenafil, no improvement in 6MWT 1.Osterman. Pediatrics 135(6). 2015. 2.Stoll. Pediatrics 126(3). 2010. 3.Mourani. AJRCCM (191). 2015. adapted from Nathan R. ACC 2017. 4. Khemani. Pediatrics 120. 2007. Increased FGF2 expression in Group 3 PH Increased FGF2 expression in Group 3 PH • • Increased FGF2 expression in premature infants BPD+PH Increased FGF2 expression in premature infants BPD+PH 400 400 FGF2 Concentration (pg/ml) FGF2 Concentration (pg/ml) 300 300 200 200 100 100 0 0 -100 -100 Control BPD + PH Control BPD + PH • Hypoxia-induced PH mouse model: 1,2 1. Chang. Cardiovasc Res. 2015 2.Gore. PLOS ONE. 2015. 2
4/21/2018 Method Hypothesis • Determine whether endothelial FGFR1 and FGFR2 signaling contribute to the development of hypoxia-induced Endothelial FGF signaling is important for the pulmonary hypertension pathogenesis of Group 3 hypoxia-induced pulmonary hypertension. • Mouse CV Phenotyping Core - Echocardiogram - Cardiac Cath • IHC + Quantify - PA muscularization - RV hypertrophy 2 weeks, 10% vs 21% FiO2 2 weeks hypoxia-induced PH 2 weeks hypoxia-induced PH • Mice challenged with 10% oxygen (hypoxia) or room air • Mice challenged with 10% oxygen (hypoxia) or room air (normoxia). (normoxia). • RV systolic pressure measured by cardiac catheterization • RV systolic pressure measured by cardiac catheterization – DCKO: Tie2-Cre;FGFR1-flox/flox;FGFR2-flox/flox – DCKO: Tie2-Cre;FGFR1-flox/flox;FGFR2-flox/flox – DFF: FGFR1-flox/flox;FGFR2-flox/flox – DFF: FGFR1-flox/flox;FGFR2-flox/flox 3
4/21/2018 Echocardiogram analysis of 2 weeks hypoxia-induced PH Loss of FGFR1,2 worsens smooth muscle hyperplasia • Fgfr1 and Fgfr2 knockout (DCKO) + 2 weeks hypoxia causes • Pulmonary Artery Acceleration (PAAT) = time to maximal velocity of RV increased tunica media/smooth muscle hyperplasia. ejection. H&E • PAAT is an accepted non-invasive measure of pulmonary hypertension in Normoxia Hypoxia both patients and mouse models. DFF DCKO Loss of FGFR1,2 worsens smooth muscle hyperplasia Loss of FGFR1,2 increases numbers of muscularized vessels • Fgfr1 and Fgfr2 knockout (DCKO) + 2 weeks hypoxia causes • Fgfr1 and Fgfr2 knockout (DCKO) + 2 weeks hypoxia increases proportion of muscularized vessels. increased tunica media/smooth muscle hyperplasia. CD31 + SMA H&E SMA Normoxia Hypoxia Normoxia Hypoxia DFF DCKO DFF DCKO Non- Partially Fully Muscularized Muscularized Muscularized p<0.05 Fully Muscularized %Vessels Muscularized 0.8 p<0.001 100 Partially Muscularized Media/CSA(20-50um) Non-Muscularized 0.6 (20-50um) * * 0.4 50 *p<0.001 0.2 A - / A B 0 0.0 DFF DCKO DFF DCKO DFF DCKO DFF DCKO Normoxia Hypoxia Normoxia Hypoxia 4
4/21/2018 FGFR1 signaling prevents hypoxia-induced PH FGF2-KO hypoxia-induced PH • Global FGF2-knockout 1 (FGF2KO) mice • Induced expression of constitutively active FGFR1 • Tie2Cre; Rosa rtTA ; Tre-caFgfr1 p<0.01 60 p<0.01 *p<0.05 60 *p<0.05 RVSP (mmHg) 40 RVSP (mmHg) 40 20 20 0 0 WT FGF2KO WT FGF2KO WT caFGFR1 WT caFGFR1 Normoxia Hypoxia Normoxia Hypoxia 1. Zhou et al. 1998. Nat Med. FGF2-KO hypoxia-induced PH Proposed Model • FGFs (FGF2) exerts independent effects on ECs and SMCs, • Global FGF2-knockout 1 (FGF2KO) mice and may influence EC-SMC interaction *p<0.05 60 55 *p<0.01 *p<0.05 RV Pressure (mmHg) RVSP (mmHg) 50 40 45 20 40 0 35 WT FGF2KO WT FGF2KO DCKO FGF2KO Hypoxia Normoxia Hypoxia 1. Zhou et al. 1998. Nat Med. 5
4/21/2018 Endothelial-Smooth Muscle Interaction Endothelial-Smooth Muscle Interaction • EC-SMC microfluidics co-culture • EC-SMC microfluidics co-culture – Pulmonary-ECs, SMCs isolated by FACs – Pulmonary-ECs, SMCs isolated by FACs Brightfield EC-GFP SMA-tdTomato DFF 24 hours Endothelial-Smooth Muscle Interaction Endothelial-Smooth Muscle Interaction • EC-SMC microfluidics co-culture • EC-SMC microfluidics co-culture – Pulmonary-ECs, SMCs isolated by FACs – Pulmonary-ECs, SMCs isolated by FACs Brightfield EC-GFP SMA-tdTomato Brightfield EC-GFP SMA-tdTomato Brightfield EC-GFP SMA-tdTomato DFF DFF DFF 24 hours 24 hours 48 hours EC-DCKO EC-DCKO EC-DCKO 6
4/21/2018 Summary Future Directions • Loss of Fgfr1 and Fgfr2 in endothelial cells worsens pulmonary 1. Investigate role of FGFs on neonatal (P0-P14) hypoxia-induced PH. hypertension in vivo and alters smooth muscle cell activity in 2. Investigate the applicability of human iPS derived ECs and SMCs in vitro . microfluidic devive • Loss of Fgf2 leads to more severe pulmonary hypertension than 3. Evaluate effects of FGF signaling on whole lung vascular distribution with high resolution Xray microscopy. endothelial deletion of Fgfr1 and Fgfr2 , and overexpression of constitutively active FGFR1 prevents the phenotype, suggesting: 1) a protective role for FGF2-FGFR1/2 signaling axis, or FGFR1 signaling, 2) FGF therapy might be beneficial for Group 3 PH, the opposite effect of previous reports in Group 1 PH . Acknowledgements Tre-caFgfr1 • • Mentor: David Ornitz Support: – Ornitz Lab members: Oliver Langenberg Pediatric Physician Scientist Training Program – Stacey House, Yin Yongjun – Drew Hagan, Lu Yang – Children’s Discovery Institute – Richard Li Postdoctoral Fellowship – Craig Smith, Stefan Traian, Ling Li • Collaborators – American College of Cardiology – Mouse Cardiovascular Phenotyping Research Award Core: Attila Kovacs, Carla Weinheimer – Steven George (UC Irvine), Aziz Traore – Washington University ICTS – Child – Dept of Engr: Mark Meacham Health Forum Challenge – Gautam Singh, Phil Levy • Chimeric receptor: FGFR3c(R248C) mutant extracellular and – – NIH (T32) Pediatric Cardiovascular WUCCI: James Fitzpatrick, Matt Joens transmembrane domain fused to the FGFR1 tyrosine kinase and Pulmonary Research Training • Committee Members domain (caFGFR1). Program – Mark Grady • FGFR3c(R248C) mutation confers ligand-independent dimerization – Patrick Jay – Washington University Center for = constitutively active FGFR1 intracellular tyrosine kinase domain. – Steve Brody Cellular Imaging Microgrants – Robert Mecham Cilvik et al. PLOs One. 2013 7
4/21/2018 Pulmonary Hypertension Echocardiogram analysis of 2 weeks hypoxia-induced PH • Clinically diagnosed as elevated pulmonary artery pressures (>25mmHg) • Pulmonary Artery Acceleration (PAAT) = time to maximal velocity of RV • High pulmonary pressure -> increased right heart workload -> right ejection heart failure • PAAT is an accepted non-invasive measure of pulmonary hypertension in both patients and mouse models. Non-Linear Regression Fit Model • Endothelial dysfunction, excessive vascular remodeling, inflammation -> increased pulmonary vascular resistance and gradual vessel occlusion 1. Lai et al. Circ Res, 2016. 8
Recommend
More recommend