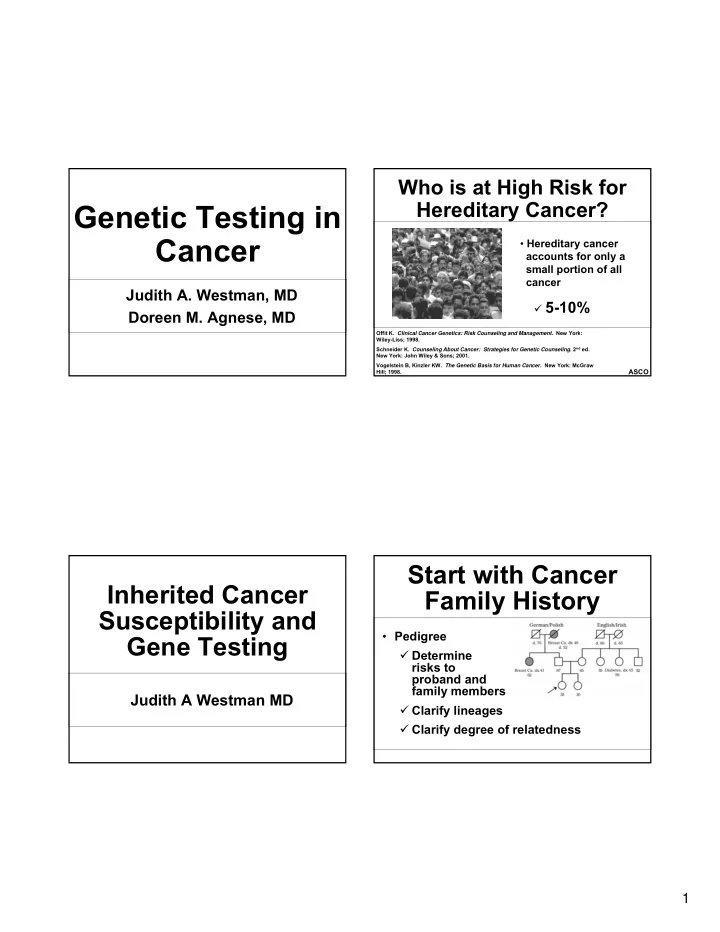
Who is at High Risk for Hereditary Cancer? Genetic Testing in Cancer • Hereditary cancer accounts for only a small portion of all cancer Judith A. Westman, MD � 5-10% Doreen M. Agnese, MD Offit K. Clinical Cancer Genetics: Risk Counseling and Management. New York: Wiley-Liss; 1998. Schneider K. Counseling About Cancer: Strategies for Genetic Counseling. 2 nd ed. New York: John Wiley & Sons; 2001. Vogelstein B, Kinzler KW. The Genetic Basis for Human Cancer. New York: McGraw ASCO Hill; 1998. Start with Cancer Inherited Cancer Family History Susceptibility and • Pedigree Gene Testing � Determine risks to proband and family members Judith A Westman MD � Clarify lineages � Clarify degree of relatedness 1
When to Suspect Hereditary Information to Obtain About Cancer Syndrome Affected Relatives • Current age • Constellation of tumors consistent with specific • Age at diagnosis and date of diagnosis/death cancer syndrome (e.g., breast and ovary) • Type, location, stage, and laterality of primary • Evidence of autosomal dominant transmission, i.e. cancer(s) � Multiple affected generations • Second cancer: metastasis or new primary? � Presence of congenital anomalies or • Environmental exposures (e.g., smoking, sun) syndrome-associated benign lesions • Ethnicity/race Olopade OI, Cummings S. Princ Pract Oncol. 1996;10:1-13. Lindor NM et al. J. Natl Cancer Inst. 1998;90:1039-1071. Schneider K. Counseling About Cancer: Strategies for Genetic Counseling. Schneider K. Counseling About Cancer: Strategies for Genetic Counseling. 2 nd ed. New York: John Wiley & Sons; 2001. 2 nd ed. New York: John Wiley & Sons; 2001. ASCO ASCO When to Suspect Hereditary When Should Genetic Testing Cancer Syndrome Be Considered? • Patient has a reasonable likelihood of • Cancer in two or more close relatives (on the same side of family) carrying an altered cancer susceptibility gene • Early age at diagnosis • Genetic testing is available that can be • Multiple primary tumors in the same individual adequately interpreted • Bilateral or multiple rare cancers • Results will influence medical management or aid in the diagnosis of a hereditary cancer syndrome Lindor NM et al. J. Natl Cancer Inst. 1998;90:1039-1071. Schneider K. Counseling About Cancer: Strategies for Genetic Counseling. 2 nd ed. New York: John Wiley & Sons; 2001. ASCO American Society of Clinical Oncology. J Clin Oncol. 2003;21:2397-2406 ASCO 2
Features That Indicate Increased Likelihood of Having BRCA Mutations • Multiple cases of early onset breast cancer Hereditary Breast and • Ovarian cancer (with family history of breast or Ovarian Cancer ovarian cancer) • Breast and ovarian cancer in the same woman Syndrome • Bilateral breast cancer • Ashkenazi Jewish heritage • Male breast cancer ASCO BRCA1 -Associated Hereditary Breast and Cancers: Lifetime Risk Ovarian Cancer Breast cancer 50% 85% (often early age at onset) Other genes BRCA1 (16%) (62%) Second primary breast cancer 40% 60% Ovarian cancer 15% 45% 7-10% BRCA2 (32%) Sporadic Possible increased risk of other Hereditary cancers (eg, prostate, colon) ASCO 3
BRCA2 -Associated Pathology Cancers: Lifetime Risk • BRCA1 breast tumors � 80% basal subtype (triple negative ER/PR/HER2) breast cancer • BRCA2 breast tumors (50% 85%) male breast � Typical distribution of molecular subtypes cancer • Ovary ovarian cancer (6%) (10% 20%) � Predominantly papillary serous adenocarcinoma � May originate from fimbria and fallopian tubes Increased risk of prostate, � Prognosis may be better than for sporadic ovarian cancer laryngeal, and pancreatic cancers (magnitude unknown) Narod SA, Offit K J Clin Oncol ASCO 2005; 23:1656-1663 BRCA1 -Linked Hereditary Other Genetic Conditions Associated Breast and Ovarian Cancer with Increased Breast Cancer Risk Syndrome Gene 92 Breast, dx 45 86 Li-Fraumeni TP53 d. 89 Cowden PTEN Noncarrier Ovary, dx 59 Breast, 73 68 71 d. 62 dx 59 BRCA1 -mutation Peutz-Jeghers STK11 carrier Affected Ataxia-telangiectasia ATM with cancer Breast, 36 (heterozygous carriers) dx 36 ASCO ASCO 4
NCCN Testing Cancer Risk Assessment Guidelines for BRCA1/2 (a.k.a. genetic counseling) Individual from family with known BRCA1/2 mutation • • Educates patient in understanding: Personal history of breast Ca plus one or more… • � Risk of having an inherited type of cancer � Dx <45yr � Dx <50yr with >1 “close” relative with breast Ca <50yr or >1 close � Mode of inheritance relative with ovarian/fallopian/primary peritoneal Ca � 2 breast primaries with one <50 � Finding the appropriate person to initiate � >2 close relatives with breast and/or ovarian* testing � Close male relative with breast � Financial and psychological costs of testing if � Personal history of ovarian* risk sufficient � Founder population with higher mutation frequency Personal hx of ovarian/fallopian/primary peritoneal • � Cancer risks to other family members Personal hx of male breast cancer • https://familyhealthlink.osumc.edu Cancer Risk Assessment (a.k.a. genetic counseling) • Informed consent for DNA testing � Likelihood of positive result � Likelihood of negative result � Likelihood of variant of uncertain significance 5
Results Disclosure Which family member would you want to test first? • Time of high anxiety for most at-risk women or women concerned about having passed risk on to next generation Prostate, dx BrCa, dx 82 • Disclosure method 70 � Face-to-face � Support person present who is not biologically related (strongly recommended) � Telephone results only if set as appointment BrCa, dx 38 BrCa, dx 44 OvCa, dx 66 Throat, dx 64 OvCa, dx 54 with patient in a private seated location (not driving) and with support person � Results should be given by health care 31 provider prepared to answer questions Results: Disclosure and Use 6
Duty to Warn Family Members • Safer v Estate of Pack (1996) � Familial adenomatous polyposis � Daughter developed CRC, sued � Physician must take reasonable steps to guarantee that immediate family members are warned • Molloy v Meier (2004) � Fragile X syndrome in previous child � “A physician’s duty regarding genetic testing and diagnosis extends beyond the patient to biological parents who foreseeably may be harmed by a breach of that duty” JAMA 292:1469-1473 (Sep 22/29, 2004) Duty to Warn Family Members Duty to Warn Resolution • Patient must be informed that other family • HIPAA ultimately prevails members are at risk • AMA: Physicians should “make themselves available to assist patients in communicating � Availability of medical interventions to with relatives to discuss opportunities for reduce the risk of developing a disease or counseling and testing, as appropriate.” to lessen the ensuing harm • ASCO: “The cancer care provider’s obligations to • Pate v Threlkel (1995) at-risk relatives are best fulfilled by communication of familial risk to the person � Familial medullary thyroid cancer undergoing testing.” � Daughter developed MTC, sued, won • Recommend written documentation to patient � Physician needed to inform patient of risks and maintained in file as part of pre-testing to family informed consent and at time of results disclosure JAMA 292:1469-1473 (Sep 22/29, 2004) 7
Medical Decision Making Individuals with a • BRCA1/2 normally involved in signaling and BRCA mutation and repairing if double strand DNA damage present in cell breast cancer • PARP1 – poly[ADP-ribose]polymerase 1 � Involved in repair of single strand DNA damage � If PARP1 not working, BRCA1/2 system corrects errors in DNA Doreen M. Agnese M.D. � If neither system working, cell death occurs • Preliminary evidence that use of PARP inhibitors in people with BRCA1/2 mutations has impressive reduction of tumor size Primary prevention of breast Surgical Decision Making cancer if BRCA1/2 mutation If positive for BRCA1 or BRCA2: • Prevents cancers from occurring in the first place • Woman may choose mastectomy rather • Prophylactic mastectomy than lumpectomy/radiation � 95-98% reduction • May choose simultaneous contralateral prophylactic mastectomy • Pre-menopausal oophorectomy (<40 years) � 40-60% risk for a contralateral primary � 40-60% reduction in breast cancer risk � One recovery period • Chemoprevention (tamoxifen) � Even reconstruction � 50% reduction in breast cancer risk in both BRCA1 and BRCA2 • Gene test results available in 1-3 weeks 8
Recommend
More recommend