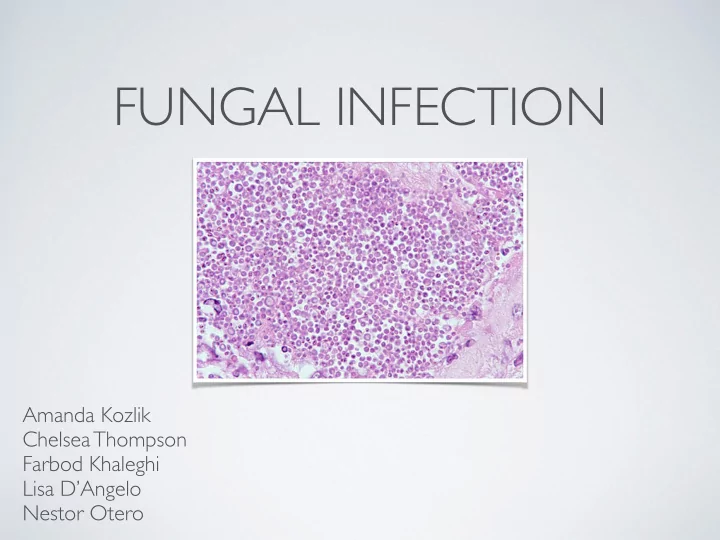
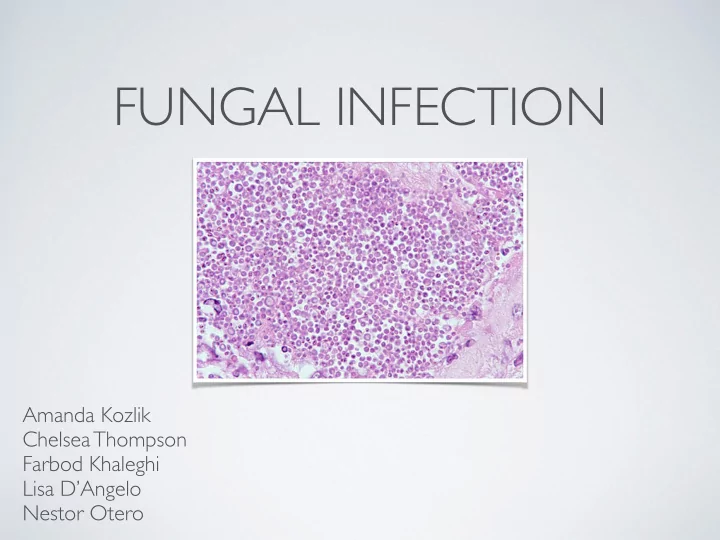
FUNGAL INFECTION Amanda Kozlik Chelsea Thompson Farbod Khaleghi Lisa D’Angelo Nestor Otero
PATIENT PRESENTATION • HPI: WM is a 66 y/o male who initially presented to the hospital for an upper GI bleed in September. The pt. had to be intubated and his admission was complicated by concurrent Providencia stuarti pneumonia, esophagitis, intermittent fevers and the presence of yeast on a blood culture. He was seen by ID, treated for 2 wks for Candida glabrata fungemia and had his IJ Perm-A-Cath removed. He was discharged from the hospital off of all antibiotics/antifungals as he had completed his course of antibiotics and micafungin. 2
PATIENT PRESENTATION • PMH: • Agitation • Cognitive impairment with anoxic metabolic • GI bleed secondary brain injury (since 2012) to esophagitis • Type 1 DM • Providencia stuarti pneumonia • End Stage Renal Disease • Candida glabrata • Anemia in CKD fungemia 3
PATIENT PRESENTATION • Allergies: no known allergies • ROS: unable to be completed; pt. seems to be at baseline mental status where he turns his head to his name, but is not really verbal or interactive 4
PATIENT PRESENTATION • Medication List: • Heparin 5000 units SQ TID • Lorazepam 0.5 mg PO daily PRN • Calcitriol 0.25 mg PO daily • Famotidine 20 mg PO BID • Insulin NPH 12 units SQ QAM and 14 units • Sevelamer 800 mg PO TID with meals SQ QHS • Darbepoetin 60 mcg/mL SQ weekly on • Insulin aspart 2 units SQ TID 5-15 mins Tuesday before meals • Midodrine 5 mg PO daily PRN prior to • Hold if NPO dialysis • If BG: < 70, give 0 units; 71-99, 3 units; • Docusate 100 mg/10 mL PO BID 100-140, 5 units; 141-180, 6 units; 181-220, 7 units; 221-260, 8 units; • Bisacodyl 10 mg suppository rectally daily 261-300, 9 units; 301-340, 10 units; > PRN 341, call MD 5
PATIENT PRESENTATION • Hospital Course: On 11/17, WM returned to the ER where he was found to be tachypneic, hypotensive and less responsive with a white count of 28.7, lactate of 3 and glucose level of 666. • His presentation was initially concerning for meningitis due to complaints of stiff neck. He was given IV ceftriaxone, vancomycin and fluids and admitted to the ICU. No further ABX were given since there was no clear source of infxn; lumbar puncture was not performed. • Radiology (performed 11/17): • Brain CT w/o contrast: no acute abnormalities • Chest x-ray: patchy airspace disease in left lung, which has been there since time of last admission (no significant changes since then) 6
PATIENT PRESENTATION • Hospital Course: On 11/23, WM was weaned off the vent and transferred out of the ICU. Central line is now out. Pt. has PEG tube for feeding. ID recommended removing the right groin femoral line, obtaining a TTE & additional ophthalmology exam and consulting pharmacy. • Since then, preliminary reports of both sets of blood cultures have returned. • Cultures (collected 11/23): • Blood Cultures (right arm) : preliminary reports from 11/24 show 4/4 bottles growing Candida glabrata • Blood Cultures (right arm): preliminary reports from 11/25 show 1/4 bottles growing Gram Positive Cocci • Pharmacy Consult (11/25) — recommending levofloxacin for GPCs 7
LABS 11/17: 28.7 11/24: 11.4 Timeline of WBC Levels 11/23: 12.9 11/25: 13.4 11/17 PM: 98.1°F 11/23 AM: 97.8°F 11/25 AM: 101.4°F Timeline of Temperature 11/22 PM: 102°F 11/23 PM: 101.6°F 8
OTHER LABS • SCr was elevated upon admission: • SCr 7.9 (on 11/17) → 2.0 (on 11/23) • CBC confirms anemia due to CKD: • Hgb, Hct: 9.8, 29.9% (on 11/25) • CrCl = 28.7 mL/min (dialysis MWF) 9
PHYSICAL EXAMINATION (11/25) VS: T 101.4ºF, P 95, RR 18, BP 122/60, Ht. 66 in., Wt. 123 lb., O 2 97% (RA) Gen: chronically ill, nontoxic, turns head to voice, in NAD HEENT: anicteric sclera, pale conjunctiva, dry mucus membranes CV: RRR Lungs: clear Abd: soft, NT, G-tube is in place Neuro: tracks with his eyes, turns to voice, does not follow any commands 10
PROBLEM LIST 1. Candida glabrata fungemia 2. Inappropriate levofloxacin recommendation 3. Inappropriate renal dosing 11
PROBLEM #1: FUNGEMIA 12
ASSESSMENT • Initial Assessment: • WM has a history of Candida glabrata fungemia • Pt. is febrile (T 101.4°F) with leukocytosis (WBC 13.4) • Medications: • Previously received a 2-week course of micafungin for the Candida glabrata fungemia in September 13
PERTINENT +/- • Pertinent Positives: • Fever 101.4°F • HR 95 • WBC 13.4 • BP 122/60 • 4/4 bottles growing Candida glabrata • Pertinent Negatives: • Pt. is normotensive and pulse is WNL 14
GOALS OF THERAPY • Promptly recognize and treat fungemia without delay (within 12 hours) upon receipt of positive blood cultures • Eradicate presence of Candida glabrata in blood • Minimize adverse effects of anti-fungal therapy • Reduce risk of mortality 15
RISK FACTORS • Risk Factors for Invasive Candidiasis with Candida glabrata : • Recent antibiotic/antifungal use • Foreign devices (i.e. chemo port, central venous cath) • Neutropenia • Receiving parenteral nutrition • Sepsis • Mechanical ventilation • ICU stay • Hemodialysis Leon C, et al. Crit Care Med . 2006; 34: 730-737. Gupta A, et al. Indian J Crit Care Med. 2015; 19(3): 151-154. 16
SEPSIS • WM meets 3 SIRS criteria: • T > 38°C → WM: 101.4°F • HR > 90 → WM: 95 3 → WM: 13,400/mm 3 • WBC > 12,000/mm • BP is stable, so no new interventions are needed at this time • BP & Temp should continue to be monitored to assess any hemodynamic instability 17
TREATMENT APPROACH • Until susceptibilities return, an appropriate antifungal with coverage for Candida glabrata should be selected • 2009 IDSA Guidelines → “For infection due to Candida glabrata, an echinocandin is preferred. (B-III)” • Echinocandin Options: Caspofungin, Micafungin, Anidulafungin 18 Pappas PG, et al. Clin Infect Dis . 2009; 48(5): 503-535.
TREATMENT APPROACH • Azoles → variable susceptibility • Flucytosine → susceptible, but reserved for invasive endocarditis or meningitis • Amphotericin B → variable susceptibility • Echinocandins → 1st line for C. glabrata 19 Pappas PG, et al. Clin Infect Dis . 2009; 48(5): 503-535.
ECHINOCANDINS • Administration: IV once daily • Metabolism: minimal hepatic metabolism • Elimination: non-enzymatic degradation • None of the echinocandins are renally adjusted in patients with renal insufficiency or dialysis 20 Pappas PG, et al. Clin Infect Dis . 2009; 48(5): 503-535.
ECHINOCANDINS • As a class, echinocandins have relatively mild adverse effects • Common Adverse Effects: • GI upset (N/V/D) • Thrombocytopenia • Headache • Fever 21 Pappas PG, et al. Clin Infect Dis . 2009; 48(5): 503-535.
PAPPAS PG, ET AL. 22 Pappas PG, et al. Clin Infect Dis . 2007; 45(7): 883-893.
PAPPAS PG, ET AL. • Background: international, randomized, double-blind trial • Setting: 595 patients in North America, Europe, Brazil & India assigned in 1:1:1 ratio to receive one of the following interventions • Possible Interventions: • Micafungin 100 mg IV once daily • Micafungin 150 mg IV once daily • Caspofungin 70 mg IV (Day 1) then 50 mg IV once daily 23 Pappas PG, et al. Clin Infect Dis . 2007; 45(7): 883-893.
PAPPAS PG, ET AL. • Inclusion Criteria: • Candidemia ( ≥ 1 positive blood culture with Candida organisms) • At least 1 of following: T ≥ 38°C or < 36°C, SBP < 90, s/sx of inflammation, x-ray findings suggesting invasive Candidiasis • Exclusion Criteria: • Pregnant/nursing • Liver disease • Life expectancy < 5 days • Candida endocarditis, osteomyelitis, meningitis • Receipt of cyclosporin or echinocandin within past month 24 Pappas PG, et al. Clin Infect Dis . 2007; 45(7): 883-893.
PAPPAS PG, ET AL. Time to Negative Groups Treatment Success Culture Micafungin 100 mg 76.4% 2 days Micafungin 150 mg 71.4% 3 days Caspofungin 72.3% 2 days Most appropriate option: micafungin 100 mg IV once daily 25 Pappas PG, et al. Clin Infect Dis . 2007; 45(7): 883-893.
SUMMARY • Micafungin is an appropriate choice for WM’s candidemia • Micafungin requires specific monitoring parameters due to possible adverse effects • Refer for ophthalmology consult to rule out Candidal endophthalmitis 26
PROBLEM #2: INAPPROPRIATE LEVOFLOXACIN RECOMMENDATION 27
ASSESSMENT • Initial Assessment: • Preliminary reports of blood cultures (from 11/25) show 1/4 bottles growing Gram Positive Cocci • Pharmacy recommended levofloxacin 28
PERTINENT +/- • Pertinent Positives: • 1/4 bottles growing Gram Positive Cocci • Pertinent Negatives: • VS are WNL 29
GOALS OF THERAPY • Ensure antibiotics are being utilized appropriately for a specific indication • Prevent collateral damage from unnecessary antibiotic use 30
TREATMENT APPROACH • The presence of Gram Positive Cocci in only 1 of the 4 bottles indicates it is likely a contamination due to Staph epidermidis • Gram (+) Cocci in clusters • Catalase (+) • Coagulase (-) 31
TREATMENT APPROACH • Await culture results to confirm contamination with Staph epidermidis • Levofloxacin therapy is not indicated for WM at this time 32
PROBLEM #3: INAPPROPRIATE RENAL DOSING 33
Recommend
More recommend