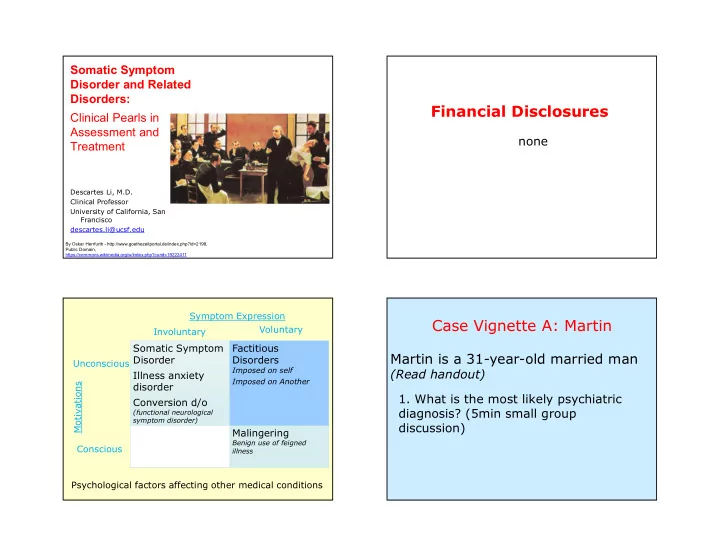
Somatic Symptom Disorder and Related Disorders: Financial Disclosures Clinical Pearls in Assessment and none Treatment Descartes Li, M.D. Clinical Professor University of California, San Francisco descartes.li@ucsf.edu By Oskar Herrfurth - http://www.goethezeitportal.de/index.php?id=2198, Public Domain, https://commons.wikimedia.org/w/index.php?curid=19222411 Symptom Expression Case Vignette A: Martin Voluntary Involuntary Somatic Symptom Factitious Martin is a 31-year-old married man Disorder Disorders Unconscious Imposed on self (Read handout) Illness anxiety Imposed on Another disorder Motivations 1. What is the most likely psychiatric Conversion d/o diagnosis? (5min small group (functional neurological symptom disorder) discussion) Malingering Benign use of feigned Conscious illness Psychological factors affecting other medical conditions 1
Somatic Symptom Disorder Keep in mind A. Somatic Symptoms: One or more somatic • Get a careful history, including pt’s perspective. symptoms that are distressing and/or result in • Prior responses, and consequences. significant disruption in daily life. B. One or more of: Excessive thoughts, feelings, • Consider the diagnosis in individuals with multiple and/or behaviors related to these somatic complaints, such as pain, fatigue, or symptoms or associated health concerns: gastrointestinal problems. 1) Disproportionate and persistent thoughts about the seriousness of one’s symptoms (thoughts) • Individuals often have both a diagnosed medical 2) Persistently high level of anxiety about health or condition and abnormal behaviors and thoughts symptoms (feelings) related to this condition. 3) Excessive time and energy devoted to these symptoms or health concern (behaviors) • These individuals are genuinely suffering. C. Chronicity: Although any one symptom may not be continuously present, the state of being symptomatic is persistent and lasts > 6 months . Comments? Examples of Disease Entities That Overlap Behavior Perspective with Somatic Symptom and Related Disorders Behavior Specialty Disease Entity Primary care Chronic fatigue syndrome Fibromyalgia Cardiology Atypical chest pain Gastroenterology Irritable bowel syndrome Choice Urology Interstitial cystitis Immunology Multiple chemical sensitivities ENT Temporomandibular joint syndrome Neurology Psychogenic non-epileptic seizures Consequences (Conversion disorder) Rumination increased likelihood Consequent beh worsened symptoms 2
Challenges Case Vignette:: Martin Hint: How do you think someone would feel if they were in Martin’s situation? How might Martin feel once he is told that he has this disorder? • invalidated 2. Patients may have strong reactions to having • abandoned and worried about being referred elsewhere. this kind of disorder. What are they and how can • uncertainty and lack of trust physicians help them with these reactions? • very alone and confused How do you think Martin might feel about the situation? Tips on how to manage SSD Tips on how to manage SSD Normal lab tests: Avoid direct confrontation about the truthfulness of the symptoms – Are reassurance that nothing catastrophic is going on, Reassure pts that: – Are useful because they have “ruled out” many • You understand that the symptoms are of the important diseases distressing – Do NOT mean that what the patient is • you won’t abandon them – pts may feel very experiencing isn’t happening. isolated and often have chronic illnesses that must be managed • You understand how confusing it is to have • Help the person identify creative and practical symptoms and yet not know if they are portend a solutions and coping strategies serious illness or if they are just normal bodily • Remember that since they may feel alone and symptoms isolated, support groups, exercise/physical therapy, or psychotherapy can be helpful 3
Tips on how to manage Case Vignette A: Martin countertransference 3. What is it like to be in the role of Dr. Smith? Learn more about the disorder Other physician wellness techniques Any tips to share about how to manage countertransference? How do you think Dr. Smith might feel about the situation? How might Dr. Smith feel about approaching Martin with the diagnosis and treatment plan? Principle/intervention Comment (yes/no, then discussion) The focus should be complete No, care rather than cure Case Vignette A: Martin remission of symptoms. Discuss social issues that may Yes, Somatic symptoms may be a means by which be distressing with patient. patients can discuss psychosocial issues. 4. Discuss each of the following clinical principles/interventions and their applicability in Have a high threshold for Yes, attempt to have diagnostic and therapeutic ordering tests conservatism. Review old records, “laying on of this patient: hands” Be especially conservative with ordering high-risk. low-yield evaluations. Instruct patient to return to No, better to have standing, regularly scheduled clinic for follow-up “as visits during which the physician focuses on needed”. “function and coping” , not the symptom experience itself, so as not to inadvertently reinforce somatic How do you think Dr. Smith might feel about the situation? How might Dr. Smith symptoms production and perpetuation feel about approaching Martin with the diagnosis and treatment plan? Instruct patient to go to No, as above Emergency Department “as needed”. 4
Principle/intervention Comment (yes/no, then discussion) Thus far Liberally use benign Yes, recommendation and use of benign remedies may remedies help the patient to feel supported. Consider routine use of physical/occupational/recreational therapy • Martin: Somatic Symptom Disorder* Refer to psychiatrist as soon No, patient may feel complaints are invalidated. as possible. Psychiatric consultation helpful for: 1) specific psychiatric co-morbidity and/or 2) if recommendations about pharmacotherapy are needed. Special attention to stable and Yes , s omatic symptom disorder is a complex illness that consistent healthcare calls for consistent and reassuring relationships with relationships confident and supportive healthcare providers Family engagement Yes, family members may perpetuate maladaptive coping and can assist an individual with somatic symptom disorders with ongoing support and understanding of the principles of treatment *note resolution of the case DSM-5 Criteria for Case Vignette B: Robin Illness Anxiety Disorder A. Preoccupation with having or acquiring a 1. What is the most likely psychiatric serious illness. B. Somatic symptoms are not present or are only diagnosis? mild (Read handout) C. High level of anxiety about health, and easily alarmed about personal health status. D. Excessive health-related behaviors or maladaptive avoidance E. at least 6 months F. Not better explained by another disorder. 5
Behavior Perspective Former diagnosis: hypochondriasis Behavior Superseded by: -somatic symptom disorder (75%) Choice -illness anxiety disorder (25%) Consequences Rumination increased likelihood Consequent beh worsened symptoms What is the difference between Keep in mind somatic symptom disorder and illness anxiety disorder? • Get a careful history, including pt’s perspective. • Prior responses, and consequences. • Consider the diagnosis in individuals with multiple • Both may present with anxiety complaints, such as pain, fatigue, or • Illness anxiety disorder with no symptoms (or gastrointestinal problems. only mild), and fears developing an illness • Individuals often have both a diagnosed medical • Somatic symptom disorder often has a medical condition and abnormal behaviors and thoughts condition with symptoms, but the reaction to related to this condition. these symptoms is maladaptive • These individuals are genuinely suffering. 6
[Examples of Disease Entities That Overlap Case Vignette B: Robin with Somatic Symptom and Related Disorders] 2. How is Robin’s clinical presentation different Specialty Disease Entity Primary care Chronic fatigue syndrome from Martin’s? Fibromyalgia Cardiology Atypical chest pain Gastroenterology Irritable bowel syndrome 3. What other psychiatric disorders should we Urology Interstitial cystitis consider Robin’s case? Immunology Multiple chemical sensitivities ENT Temporomandibular joint syndrome Neurology Psychogenic non-epileptic seizures (Conversion disorder) Can be conceptualized as “contested illnesses” See Dumit 2006. Illnesses you have to fight to get: Facts as forces in uncertain, emergent illnesses. Social Science & Medicine 62 (2006) 577–590 Key rule outs 1. Psychosis for somatic symptom disorder – Work with psychiatrist to and related disorders manage delusions 1. Psychosis – If psychosis with poor insight, recommend: I 2. Anxiety disorders, especially OCD Am Not Sick, I Don't Need 3. Depression Help: How To Help Someone 4. Cultural syndromes With Mental Illness Accept Treatment, by Xavier 5. Factitious disorders* Amador – Consider diagnoses Each has a different management besides schizophrenia approach. *separate section on factitious disorders 7
Recommend
More recommend