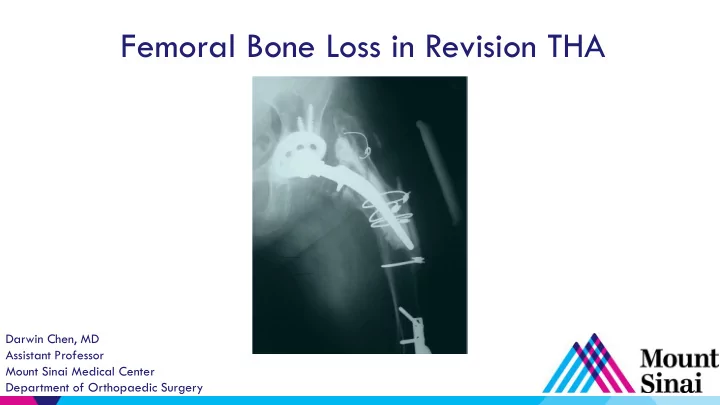
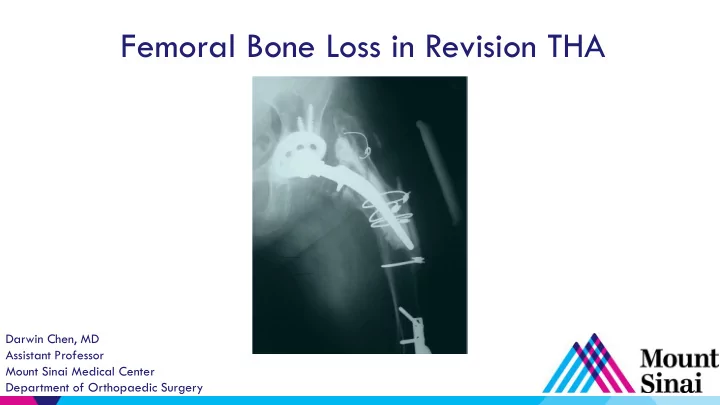
Femoral Bone Loss in Revision THA Darwin Chen, MD Assistant Professor Mount Sinai Medical Center Department of Orthopaedic Surgery
Disclosures ▶ Monogram Orthopedics Consultant –
The Challenge of Femoral Revision ▶ Proximal femoral bone loss – Osteolysis – Stress shielding – Implant removal – ETO ▶ Loose stems - varus and retroverted femoral remodeling ▶ Goal: Stable distal fixation and preservation of bone stock
Paprosky Classification ▶ Reliable, reproducible ▶ Predicts intraoperative bone loss ▶ Quantifies remaining femoral host bone ▶ Guides reconstructive options ▶ Can easily turn a I/II into a III with iatrogenic damage!
Paprosky I ▶ Minimal metaphyseal bone loss ▶ Diaphysis intact ▶ Tx: standard stem – Cementless or cemented
Paprosky I
Paprosky I
Paprosky II ▶ Metaphysis d amaged, non- supportive ▶ Isthmus fully intact ▶ Diaphyseal cortices supportive ▶ Tx – diaphyseal engaging stem, +/- proximally fixed
Paprosky II ▶ Proximally coated, distally fixed - SROM
Paprosky II ▶ Diaphyseal engaging – modular tapered Ti
Paprosky III (A vs. B) ▶ Metaphysis is severely damaged and non-supportive ▶ Diaphysis intact – 3A >4cm of isthmus – 3B <4cm ▶ Diaphyseal fixation ▶ Tx: 3A - fully coated cylindrical 3B – tapered fluted (Wagner)
Paprosky IIIA ▶ >4cm isthmus - fully coat cylindrical
Paprosky IIIA
Paprosky IIIB ▶ <4cm isthmus - tapered fluted Ti – Monobloc (Wagner type) vs. modular
Paprosky IV ▶ Extensive meta-diaphyseal damage ▶ Nonsupportive isthmus ▶ Analogous to Vancouver B3 ▶ Tx – Megaprosthesis – APC – Tapered fluted Ti Stem?
Paprosky IV ▶ Megaprosthesis – Salvage
Extended Trochanteric Osteotomy (ETO) ~ 12-15cm ▶ Facilitates – Exposure – Component/cement removal – Reaming/insertion of revision stem
The Workhorse: Modular Tapered Ti Stem ▶ Applicable for almost every revision case (Type 1-3b, some 4s) ▶ Reliable, reproducible, simple – New gold standard? ▶ “Pot” the distal stem where it wants to go ▶ “Build” up with the proximal body – Length, offset, version, proximal fill
Not All Modular Tapered Stems Are Created Equal! ▶ Taper angle – Axial stability – 2 to 3.5 degrees ▶ Spline design – Rotational stability – Sharp/flat/variable ▶ Distal geometry – Kinked/bowed/beveled
Not All Modular Tapered Stems Are Created Equal! ▶ Modular junction problems – Breakage – Corrosion? ▶ Subsidence ▶ Cost
What is the Limit of a Modular Tapered Stem? ▶ B/l loose hemis, severe varus remodeling (R cemented, infected)
What is the Limit of a Modular Tapered Stem? ▶ Vancouver B3 periprosthetic fx / Paprosky IV (1cm isthmus left)
Technique Tips – Mod Tapers ▶ ETO for implant removal or varus remodeling ▶ Distal prophylactic cable if ETO or any doubt ▶ Ream on power vs hand? ▶ Ream to a mid size proximal modular body ▶ Low threshold for intraop XR
Technique Tips – Mod Tapers ▶ Be wary of anterior distal stem perforation
Technique Tips – Mod Tapers ▶ Make sure to bottom out the proximal body reamer
Conclusions ▶ Diaphyseal fixation is key for femoral revisions ▶ ETO for safe implant removal, deformity correction, and easier reaming ▶ Modular tapered Ti stems are the workhorse for most revisions ▶ “Pot” and “build” ▶ Be watchful for subsidence, perforation, junctional failures
Thank You Darwin Chen, MD Assistant Professor Mount Sinai Medical Center Department of Orthopaedic Surgery
Recommend
More recommend