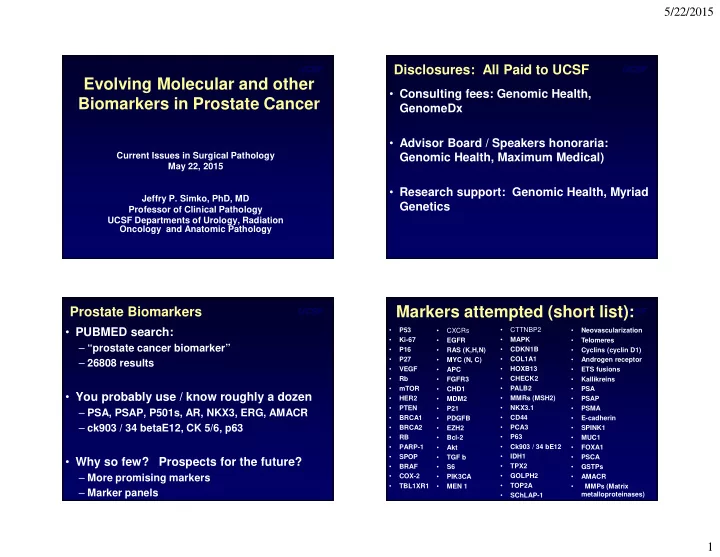
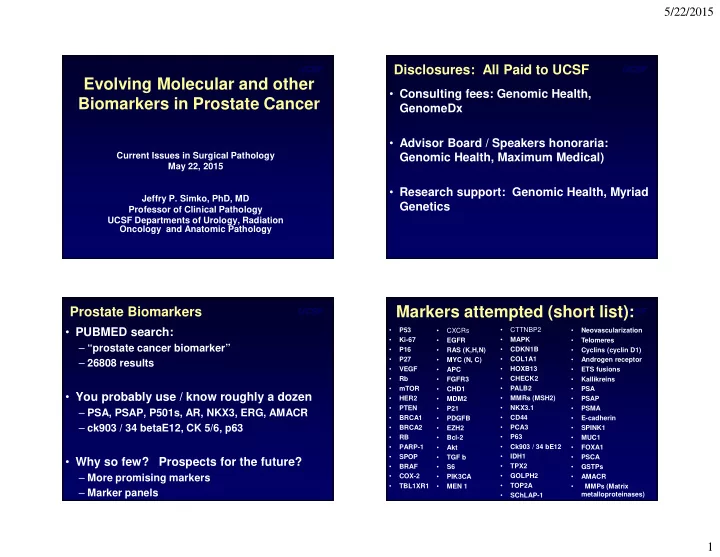
5/22/2015 UCSF UCSF Disclosures: All Paid to UCSF Evolving Molecular and other • Consulting fees: Genomic Health, Biomarkers in Prostate Cancer GenomeDx • Advisor Board / Speakers honoraria: Current Issues in Surgical Pathology Genomic Health, Maximum Medical) May 22, 2015 • Research support: Genomic Health, Myriad Jeffry P. Simko, PhD, MD Genetics Professor of Clinical Pathology UCSF Departments of Urology, Radiation Oncology and Anatomic Pathology UCSF Markers attempted (short list): UCSF Prostate Biomarkers • PUBMED search: P53 • CTTNBP2 • • CXCRs • Neovascularization • Ki-67 • MAPK • EGFR • Telomeres – “prostate cancer biomarker” • P16 • RAS (K,H,N) • CDKN1B • Cyclins (cyclin D1) • COL1A1 • P27 • MYC (N, C) • Androgen receptor – 26808 results • VEGF • HOXB13 • APC • ETS fusions • Rb • CHECK2 Kallikreins • FGFR3 • • PALB2 • mTOR • CHD1 • PSA • You probably use / know roughly a dozen HER2 • MMRs (MSH2) • • MDM2 • PSAP • PTEN • NKX3.1 • P21 • PSMA – PSA, PSAP, P501s, AR, NKX3, ERG, AMACR • BRCA1 • PDGFB • CD44 • E-cadherin – ck903 / 34 betaE12, CK 5/6, p63 • PCA3 • BRCA2 • EZH2 • SPINK1 • RB • P63 • Bcl-2 • MUC1 • PARP-1 • Ck903 / 34 bE12 FOXA1 • Akt • • IDH1 • SPOP • TGF b • PSCA • Why so few? Prospects for the future? BRAF • TPX2 • • S6 • GSTPs – More promising markers • COX-2 • GOLPH2 • PIK3CA • AMACR • TBL1XR1 • MEN 1 • TOP2A • MMPs (Matrix – Marker panels metalloproteinases) • SChLAP-1 1
5/22/2015 UCSF UCSF Markers (by pathway, e.g. akt): Markers use (diagnosis): • P53 • CTTNBP2 • P53 • CTTNBP2 • CXCRs • Neovascularization • CXCRs • Neovascularization • Ki-67 EGFR • MAPK • Telomeres • Ki-67 EGFR • MAPK • Telomeres • • • CDKN1B • CDKN1B • P16 • RAS (K,H,N) • Cyclins (cyclin D1) • P16 • RAS (K,H,N) • Cyclins (cyclin D1) • P27 • COL1A1 • P27 • COL1A1 • MYC (N, C) • Androgen receptor • MYC (N, C) • Androgen receptor • VEGF • HOXB13 • ETS fusions • VEGF • HOXB13 • ETS fusions • APC • APC CHECK2 CHECK2 • Rb • FGFR3 • • Kallikreins • Rb • FGFR3 • • Kallikreins • PALB2 • PALB2 • mTOR • CHD1 • PSA • mTOR • CHD1 • PSA • HER2 • MMRs (MSH2) • HER2 • MMRs (MSH2) • MDM2 • PSAP • MDM2 • PSAP • PTEN P21 • NKX3.1 • PSMA • PTEN P21 • NKX3.1 • PSMA • • • CD44 • CD44 • BRCA1 • PDGFB • E-cadherin • BRCA1 • PDGFB • E-cadherin • BRCA2 • PCA3 • BRCA2 • PCA3 • EZH2 • SPINK1 • EZH2 • SPINK1 • RB • P63 • MUC1 • RB • P63 • MUC1 • Bcl-2 • Bcl-2 Ck903 / 34 bE12 Ck903 / 34 bE12 • PARP-1 • Akt • • FOXA1 • PARP-1 • Akt • • FOXA1 • IDH1 • IDH1 • SPOP • TGF b • PSCA • SPOP • TGF b • PSCA • BRAF • TPX2 • BRAF • TPX2 • S6 • GSTPs • S6 • GSTPs • COX-2 • PIK3CA • GOLPH2 • AMACR • COX-2 • PIK3CA • GOLPH2 • AMACR / P504s • TOP2A • TOP2A • TBL1XR1 • MEN 1 • MMPs (Matrix • TBL1XR1 • MEN 1 • MMPs (Matrix metalloproteinases) metalloproteinases) Markers (Prognosis): UCSF Markers use (Panels): UCSF P53 • CTTNBP2 P53 • CTTNBP2 • • CXCRs • Neovascularization • • CXCRs • Neovascularization • Ki-67 • MAPK • Ki-67 • MAPK • EGFR • Telomeres • EGFR • Telomeres • P16 • RAS (K,H,N) • CDKN1B • Cyclins (cyclin D1) • P16 • RAS (K,H,N) • CDKN1B • Cyclins (cyclin D1) • COL1A1 • COL1A1 • P27 • MYC (N, C) • Androgen receptor • P27 • MYC (N, C) • Androgen receptor • VEGF • HOXB13 • VEGF • HOXB13 • APC • ETS fusions • APC • ETS fusions • Rb • CHECK2 Kallikreins • Rb • CHECK2 Kallikreins • FGFR3 • • FGFR3 • • PALB2 • PALB2 • mTOR • CHD1 • PSA • mTOR • CHD1 • PSA HER2 • MMRs (MSH2) HER2 • MMRs (MSH2) • • MDM2 • PSAP • • MDM2 • PSAP • PTEN • NKX3.1 • PTEN • NKX3.1 • P21 • PSMA • P21 • PSMA • BRCA1 • PDGFB • CD44 • E-cadherin • BRCA1 • PDGFB • CD44 • E-cadherin • PCA3 • PCA3 • BRCA2 • EZH2 • SPINK1 • BRCA2 • EZH2 • SPINK1 • RB • P63 • RB • P63 • Bcl-2 • MUC1 • Bcl-2 • MUC1 • PARP-1 • Ck903 / 34 bE12 FOXA1 • PARP-1 • Ck903 / 34 bE12 FOXA1 • Akt • • Akt • • IDH1 • IDH1 • SPOP • TGF b • PSCA • SPOP • TGF b • PSCA BRAF • TPX2 BRAF • TPX2 • • S6 • GSTPs • • S6 • GSTPs • COX-2 • GOLPH2 • COX-2 • GOLPH2 • PIK3CA • AMACR • PIK3CA • AMACR / P504s TOP2A • TBL1XR1 • MEN 1 • TOP2A • MMPs (Matrix • TBL1XR1 • MEN 1 • • metalloproteinases) Pollack, et al., Clin Cancer Res. 20(24): 6379-88 (2014) • SChLAP-1 2
5/22/2015 UCSF UCSF Clinically significant ones: Biomarker uses (General): • P53 • CTTNBP2 • CXCRs • Neovascularization • Ki-67 EGFR • MAPK • Telomeres • • Screening (serum PSA) • CDKN1B • P16 • RAS (K,H,N) • Cyclins (cyclin D1) • P27 • COL1A1 • MYC (N, C) • Androgen receptor • Diagnosis (Bx) • VEGF • HOXB13 • ETS fusions • APC ??? CHECK2 • Rb • FGFR3 • • Kallikreins • Prognosis • PALB2 • mTOR • CHD1 • PSA • Predictive (Likelihood of response to Rx) • HER2 • MMRs (MSH2) • MDM2 • PSAP • PTEN P21 • NKX3.1 • PSMA • – Reimbursement most likely • CD44 • BRCA1 • PDGFB • E-cadherin • BRCA2 • PCA3 • EZH2 • SPINK1 – Develop drugs based on targets • RB • P63 • MUC1 • Bcl-2 • Disease monitoring Ck903 / 34 bE12 • PARP-1 • Akt • • FOXA1 • IDH1 • SPOP • TGF b • PSCA • BRAF • TPX2 • S6 • GSTPs • COX-2 • PIK3CA • GOLPH2 • AMACR / P504s TOP2A • • TBL1XR1 • MEN 1 • Clinical Indications: Summary Map of therapies UCSF UCSF Why little success in Prostate? • Specific Clinical Indication – What application? (disease state) Inc. – Localized disease: Clinical parameters already PSA do a decent job (Gleason = high bar to reach). – Metastatic Disease: Success with anti- androgens and lack of study material Dx: Active Docetaxel surveillance http://www.onclive.com/publications/obtn/2012/december-2012/ • Tumor Multifocality sequencing-of-novel-prostate-cancer-agents-is-a-work-in-progress/2 3
5/22/2015 UCSF UCSF PCa at Primary Diagnosis PCa at Primary Diagnosis “Continuum of aggressiveness” “Continuum of aggressiveness” “Indolent Tumors” “Indolent Tumors” “Aggressive tumors” “Aggressive tumors” GS < 7 GS < 7 GS > 3+4 = 7 GS > 3+4 = 7 Primary Primary No treatment Primary No treatment Primary Treatment & Treatment & needed ? Treatment needed ? Treatment ? additional ? additional curable? curable? treatment treatment Active Active Prostatectomy Prostatectomy needed? needed? surveillance Radiation surveillance Radiation UCSF UCSF Active Surveillance as Rx: • Epstein Criteria (JHU): Insignificant Cancer – cT1c, No Gleason > 3, PSAD<0.15ng/mL, < 3 cores +, < 50% Ca/core • Multiple Other Criteria: – D’Amico: PSA < 10, cT2a or less, No Gleason >3 Outcome chart – Dall’Era: No Gleason > 3, PSA < 10, <33% + cores, < 50% / core – Van As: cT2a or less, PSA<15, GS<=7,< 50% cores + • F/U schedule? Rare deaths: All had PSA doubling time < 2 years Bastian et al., Eur Urol 55: 1321-1332 (2009) Klotz, J Clin Oncol. 28: 126-31 (2010) 4
5/22/2015 UCSF UCSF Kattan: Preoperative Nomogram for BCR after RP Risk assessment Tools: • Kattan Nomograms: PSA, c stage, GS • CAPRA: PSA, c stage, GS, of + cores, Age Kattan nomograms • NCCN: PSA, c stage, GS http://www.tri-kobe.org/nccn/guideline/urological/english/prostate.pdf • Many others: Partin Tables, D’Amico, Stephenson, etc. Graefen, J Clin Oncol. 20(15): 3206-3212 (2002) Lughezzani, et al., Eur Urol 57(4): 562-8 (2010) CAPRA: Preoperative prediction of BCR after RP UCSF UCSF CAPRA CAPRA Cooperberg, et al., Cancer 107(10): 2384-2391 (2006) Cooperberg, et al., Cancer 107(10): 2384-2391 (2006) 5
5/22/2015 UCSF UCSF Tumor Heterogeneity and Sampling: Tumor Multifocality: What gets biopsied? • Did the cancer get sampled? • Did the clinically significant cancer? Clinical Indications: Summary Map of therapies UCSF UCSF Marker Examples: • Management of localized disease – ETS Fusions – PTEN – Various Marker Panels Inc. PSA • Management of Systemic Disease – AR-V7 Dx: Active Docetaxel surveillance http://www.onclive.com/publications/obtn/2012/december-2012/ sequencing-of-novel-prostate-cancer-agents-is-a-work-in-progress/2 6
Recommend
More recommend