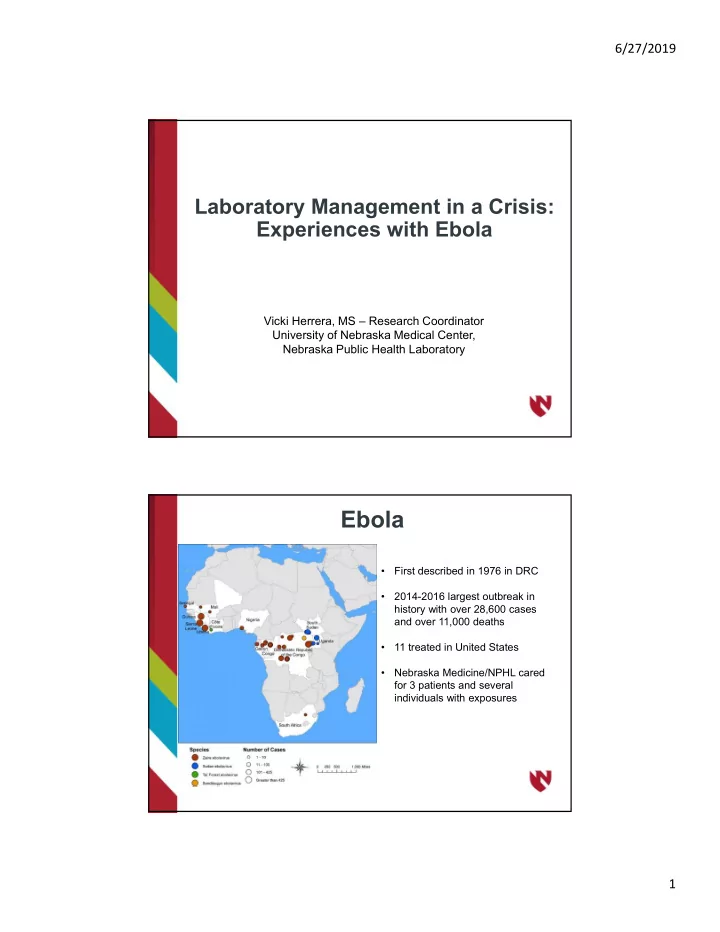
6/27/2019 Laboratory Management in a Crisis: Experiences with Ebola Vicki Herrera, MS – Research Coordinator University of Nebraska Medical Center, Nebraska Public Health Laboratory Ebola • First described in 1976 in DRC • 2014-2016 largest outbreak in history with over 28,600 cases and over 11,000 deaths • 11 treated in United States • Nebraska Medicine/NPHL cared for 3 patients and several individuals with exposures 1
6/27/2019 Objectives • Lab Management • Lessons Learned • Moving Forward Background • 1997 Public Health Laboratory moves to Omaha • 2005 Nebraska Biocontainment Unit Opens • July 2014 – State Department visited to assess readiness • August 2014 Emory receives 2 patients infected with Ebola virus to their Biocontainment Unit • September 4, 2014 Nebraska receives first patient infected with Ebola virus 2
6/27/2019 Why Nebraska Public Health Lab (NPHL)? • NPHL was designated as the lab to test specimens for the NBU • Integrated into UNMC/Nebraska Medicine • Proximity to NBU • BSL-3 lab • Contact with CDC • Part of LRN • Tests initially provided • iSTAT (electrolytes) • Malaria smears Challenges • Expand the test menu • Train staff • Comply with regulatory requirement • Short time frame 3
6/27/2019 Lines of communication Infectious NBU Critical Care Disease Nursing Physicians Personnel Staff Hospital Hospital Admin Lab Staff Pharmacy / Environ. IRB Services NPHL Pharm. Industrial Companies Hygienists Shipping CDC Couriers Federal DSAT State HHS Depart. HHS Expand Test Menu • Define essential list of test • Liver function • Coagulation • Define where testing could safely be performed • Define who could safely perform testing 4
6/27/2019 Performing a Risk Assessment • Is there a potential for aerosol generation? • Vortexing • Pipetting • Centrifugation • Opening and closing tubes • Are sharps used? • Are appropriate PPE available? • Face shields, gowns, gloves, respiratory protection, booties, bonnet • Are staff trained in the utilization of the PPE? • Doffing and donning • Is a protocol for waste disposal available? Results of Our Risk Assessment • Chemistry automated analyzer • Initial centrifugation did not use sealed rotors • centrifuge in BSL-3 with sealed rotor • Coagulation automated analyzer • Required open tube testing • POC Instrumentation (Hemochron analyzer) in BSL-3 • Blood Bank • Cross matching required open tube centrifugation • Perform blood type by slide agglutination in BSL-3 5
6/27/2019 Test menu before Risk Assessment Test menu after Risk Assessment 6
6/27/2019 Staff Training Requirements Trained in BSL-3 practices Trained in PPE Trained on POC analyzers NPHL Staff = 3 ½ Plus Director PPE N95 Mask Double Glove Impermeable Gown Hair Bonnet Shoe Covers Face Shield 7
6/27/2019 Lab Safety Buddy System Lab Safety 8
6/27/2019 Lab Safety Lessons Learned after 1 st patient • Needed more trained staff • Needed a laboratory within the NBU • Communication is key • Shipping was challenging • Support for Laboratory staff 9
6/27/2019 Benefits of Moving Lab to NBU • Reduced TAT for Tests • Increased Communication between departments establishing a Team atmosphere • Better patient management for physicians/nurses 10
6/27/2019 Successes • Increased POC testing options • Increased staffing • Laboratory integrated into the NBU • Successful care of patients Challenges • Shipping specimens • Training • Sustainability • Funding • Staffing 11
6/27/2019 Moving Forward • Increased testing options • Increased our staff training program • Participate in local, state and national drills • Building a successful program to train other laboratorians within the State and the Nation • Members of national committees addressing different areas of concern • Be Flexible!! Laboratory Management During a Crisis: Experiences with Zika Andrew Cannons, Ph.D., HCLD(ABB) Laboratory Director Bureau of Public Health Laboratories (BPHL) Tampa 6/27/2019 12
6/27/2019 Outline • Zika Testing –The Process Broken Down • Managing the Zika Response • What, Where, When • Identification of Successes and Challenges at Each Step • Moving Forward, experiences in 2017 • Final Thoughts Zika Sample Collection/Testing/Reporting ‐ The Simplistic View! 2: Samples to Lab Serum, urine 1: Case Identification 3: Testing Symptomatic PCR/ELISA Travel History Asymptomatic pregnant with/without travel Diagnosis 4: Reporting to Submitters 13
6/27/2019 Zika Sample Collection/Testing/Reporting ‐Where the Challenges Were! 2: Samples to Lab Serum, urine 1: Case Identification 3: Testing Symptomatic PCR/ELISA Travel History Asymptomatic pregnant with/without travel Diagnosis 4: Reporting to Submitters 1. Case Identification and Review: Epidemiology Surveillance and Local Response Challenges • Guidance documents produced for partners: • Need a more efficient process to circulate quicker • Better use of surveillance tools 1: Case Identification Symptomatic • Case review process Travel History Asymptomatic pregnant with/without travel • Complicated, changing algorithm • Better use of surge staff • Communications • Particularly with laboratories about incoming samples/priority testing 14
6/27/2019 2. Samples to Laboratory Successes 2: Samples to Lab Serum, urine • Initially able to deal with increased volume of samples: • Samples received mainly from usual submitters • Receiving and accessioning area set up in laboratories • Used testing algorithm to determine where samples went for testing • With local case identification: • Large increase in submitted samples • Mobilized staff to help with increase load • BPHL‐Miami set up triage area to re‐route samples to Jacksonville and Miami • Able to continue receiving and accession all non‐Zika samples 2. Samples to Laboratory Challenges 2: Samples to Lab Serum, urine • Sample delivery: • Boxes delivered from new submitters • Laboratory/department not always identified • Large increase in numbers • Specimen Integrity: • Some poor samples delivered • Leaking, broken tubes • Criteria for satisfactory vs. unsatisfactory not established • Accessioning: • Testing algorithm changed • Testing algorithm required interpretation and slowed down accessioning 15
6/27/2019 2. Samples to Laboratory Challenges 2: Samples to Lab Serum, urine • Sample Submission form: • Initially our sample submission form did not work for Zika testing • Not always complete information provided • Incomplete information held up data entry into Labware ‐initially • High Priority: • Determining high priority samples was difficult early on • Development of an Excel file helped with this • Blood Bank samples: • Always ended up with two sets of samples and two sets of submission forms that were confusing to link up • Difficult to confirm • Commercial Lab Samples: • Confirming positives added to high sample burden 2. Samples to Laboratory Challenges to Successes 2: Samples to Lab Serum, urine Guidance documents developed for those submitting samples: • Developed guidance documents for sample submission • Help with what sample types, how to package, how and where to ship • Developed FAQ documents for those submitting samples • Answered the commonly asked questions Updated sample submission form to work for Zika testing 16
6/27/2019 3. Laboratory Testing Successes 3: Testing PCR/ELISA • Both BPHL‐Jacksonville and BPHL‐Tampa had PCR and ELISA test (set up in 2015) • BPHL‐Miami brought on board in July 2016 with CDC Trioplex assay: • Urine surveys, serum/urine testing later on • Initially able to maintain testing of approximately 250 PCR and 250 ELISA per week • Maintained testing of all non‐Zika samples in laboratory 3. Laboratory Testing Successes 3: Testing • Utilized Surge Plan: PCR/ELISA • Internal Surge: mobilized staff in laboratory to help out with accessioning, processing, testing • External Surge: Epidemiology and CDC staff deployed on short term basis to help with paperwork, and non licensed testing • Shipped surge samples to CDC (over 1500 during 6 weeks) • Communications: • Overall worked well • Daily calls between the three laboratories • Input on Incident Management Team calls, via Operations 17
6/27/2019 3. Laboratory Testing Challenges 3: Testing • Testing Platform: PCR/ELISA • Urged to switch to FDA approved PCR assay (Trioplex) during the outbreak • Brought challenges including approved sample types, reporting to CDC, licensing issues • Huge increase in sample load: • Equipment in place not designed for high throughput • Not enough staff for high throughput (initially staff doing accessioning were same staff doing testing) • Staff needing to work extra hours –fatigue, low moral 3. Laboratory Testing Challenges to Successes 3: Testing Instrumentation: PCR/ELISA • At the beginning of 2016 BPHL was not geared for Zika surge testing • Equipment not designed for high throughput • Added later in the year: • PCR extraction capacity increased – added MagnaPure 96 robots in each laboratory • ELISA testing increased – added additional plate washers and readers in each laboratory 18
Recommend
More recommend