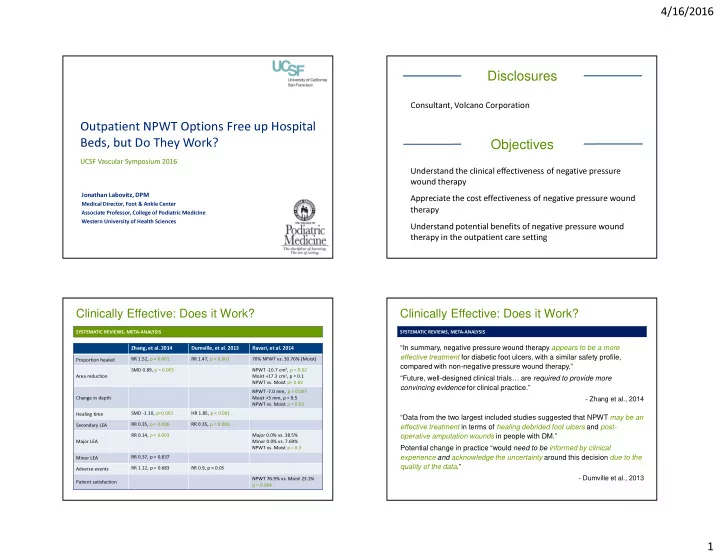
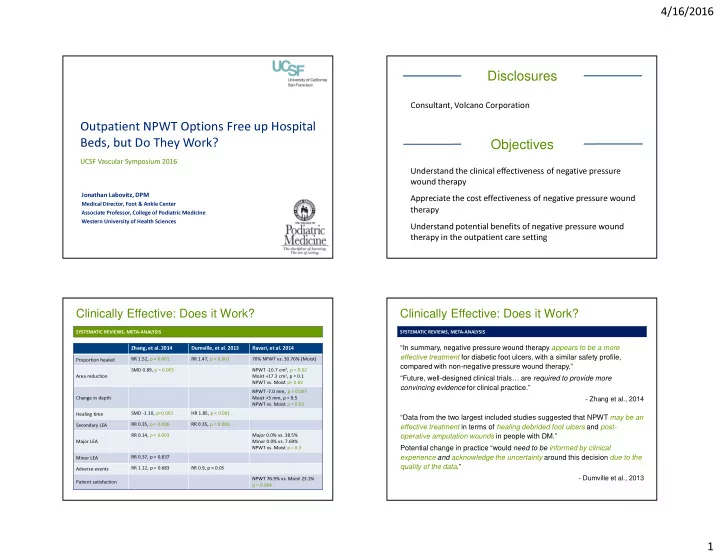
4/16/2016 Disclosures Consultant, Volcano Corporation Outpatient NPWT Options Free up Hospital Objectives Beds, but Do They Work? UCSF Vascular Symposium 2016 Understand the clinical effectiveness of negative pressure wound therapy Jonathan Labovitz, DPM Appreciate the cost effectiveness of negative pressure wound Medical Director, Foot & Ankle Center therapy Associate Professor, College of Podiatric Medicine Western University of Health Sciences Understand potential benefits of negative pressure wound therapy in the outpatient care setting Clinically Effective: Does it Work? Clinically Effective: Does it Work? SYSTEMATIC REVIEWS, META-ANALYSIS SYSTEMATIC REVIEWS, META-ANALYSIS “In summary, negative pressure wound therapy appears to be a more Zhang, et al. 2014 Dumville, et al. 2013 Ravari, et al. 2014 effective treatment for diabetic foot ulcers, with a similar safety profile, RR 1.52, p < 0.001 RR 1.47, p < 0.001 70% NPWT vs. 30.76% (Moist) Proportion healed compared with non-negative pressure wound therapy.” NPWT -10.7 cm 2 , p = 0.02 SMD 0.89, p = 0.003 “Future, well-designed clinical trials… are required to provide more Moist +17.3 cm 2 , p = 0.1 Area reduction NPWT vs. Moist p= 0.03 convincing evidence for clinical practice.” NPWT -7.0 mm, p = 0.007 - Zhang et al., 2014 Change in depth Moist +3 mm, p = 0.5 NPWT vs. Moist p = 0.02 “Data from the two largest included studies suggested that NPWT may be an SMD -1.10, p=0.003 HR 1.85, p < 0.001 Healing time effective treatment in terms of healing debrided foot ulcers and post- RR 0.35, p = 0.006 RR 0.35, p = 0.006 Secondary LEA operative amputation wounds in people with DM.” RR 0.14, p = 0.003 Major 0.0% vs. 38.5% Major LEA Minor 0.0% vs. 7.69% Potential change in practice “would need to be informed by clinical NPWT vs. Moist p = 0.3 experience and acknowledge the uncertainty around this decision due to the RR 0.37, p = 0.837 Minor LEA quality of the data .” RR 1.12, p = 0.683 RR 0.9, p > 0.05 Adverse events - Dumville et al., 2013 NPWT 76.9% vs. Moist 23.1% Patient satisfaction p = 0.004 1
4/16/2016 Clinically Effective: Does it Work? Recommendations for use SYSTEMATIC REVIEWS, META-ANALYSIS INTERNATIONAL EXPERT PANEL RECOMMENDATIONS (INDUSTRY SPONSORED) CLINICAL GUIDELINES “… sufficient evidence to conclude that healing of diabetes associated Canadian Diabetes Association, 2013 A Must be considered as advanced therapy for Univ. Texas Grade 2 or 3 post-op DM feet w/out ischemia No Recommendation chronic lower extremity wounds can be accelerated with use of NPWT.” • A Insufficient evidence for any recommendation for routine DFU management Achieve healing by secondary intention • - Xie et al., 2010 Some evidence for post-op use after extensive debridement B Stop when wound healing progressed so wound can be healed by surgical means AHRQ, 2012 (United States) Grade C B Consider in an attempt to prevent amputation or re-amputation • “Although the number of patients in this study was limited, the results May increase complete wound closure compared to standard wound dressings • obtained from this study and satisfaction of the patients allowed us to Associated with lower risk secondary to infections IDSA, 2012 (Infectious Disease) Weak (level), Low (quality) conclude the V.A.C. is a suitable treatment modality in the management of • Consider for selected DFU slow to heal consider using NWPT diabetic foot ulcers.” - Ravari et al., 2014 NHMRC, 2011 (Australian) Grade B • Use in specialist centers as part of comprehensive wound program “ Moderate quality evidence suggests that NPWTs improve healing of NICE, 2011 (United Kingdom) Low Quality DFUs and non-healing post-amputation wounds compared to standard • Clinical trials and rescue therapy (when amputation only option) - Not used routinely wound care.” SIGN, 2010 (Scottish) Grade B • Consider in active DFU or post-operative wounds “Many questions remain regarding the ideal patient population and cost effectiveness .” - Braun et al., 2014 Cost Effective? Cost Effective? Cost Outcomes Cost Outcomes DRIVER ET AL., 2014 HUTTON ET AL., 2011 CONCLUSION Cost-effective non-healing DFU treatment 16 weeks Recalcitrant wounds, high efficiency NPWT, > 1 home health wounds ≥ 12 weeks visits = fewer amputations, more QALYs at lower costs Higher NPWT efficiency � Lower resource utilization = Cost effectiveness � Lower procedure expenditures COST-EFFECTIVENESS MARKOV MODEL WHITEHEAD ET AL., 2010 � Improved healing rates ulcer free months, QALYs, cost/patient � Cost sensitive to hospital stay , # infected DFU NPWT = lower costs w/ additional QALYs and fewer LEA 2
4/16/2016 Outpatient efficacy: Is data analysis possible? AHRQ HTA: NPWT Technologies, June 2014 Time Closure NPWT Moist P value OUTPATIENT NPWT USE to � Most studies care setting is vague 100% 96 days Undeterminable 0.001 heal � If inpatient & outpatient population, unable to analyze separately 75% 58 days 84 days 0.014 NPWT vs. Moist Therapy for Stage 2 or 3 DFU Ford et al., 2002 PRESSURE ULCERS PRESSURE ULCERS Schwien et al., 2005 100% Home health records database Randomized 22 patients, 35 ulcers NPWT 95.3% stage III/IV non-healing ulcers 89.5% in 6 week trial 80% Moist therapy � NPWT (n = 60) � NPWT (n=20) 60% � No NPWT (n = 2,288) 62.1% � Healthpoint topical gel (n=15) 51.2% 40% 43.2% 16.9% 13.6% 50% 10.2% 28.9% 48% 20% 4.1% 40% NPWT 30% 35% 0% No NPWT Complete healing 75% healing Secondary LEA Adverse events Outpatient therapy 20% days 8% 5% 10% 14% 0% 0% NPWT greater efficacy, fewer secondary amps than moist Admission Admission Emergent therapy rate care BLUME ET AL., DIABETES CARE 2008 Outpatient efficacy: Is data analysis possible? Outpatient efficacy: Is data analysis possible? Outpatient NPWT vs. Moist Therapy ALL CARE SETTINGS APELQVIST ET AL., AM J SURG 2008 OUTPATIENT CARE SETTING Cost difference p < 0.001 35% of patients ≥ 8 weeks 125 APELQVIST ET AL., AM J SURG 2008 therapy had inpatient care � Dressing changes � Abx costs 118 100 � RCT, 16 weeks therapy or All costs Outpatient costs unknown NPWT complete healing � Cost analysis not by care setting 75 � Staff time � Procedures Moist Therapy � DFU S/P partial foot � Total therapy days 89.1% outpatient 50 amputation p < 0.05 41 NPWT (n=77) 25 � 11 NPWT vs. Moist Therapy, All Care Settings Moist wound therapy (n=85) � 4 60 0 Clinic visits Dressing ∆ 55.8 54 NPWT Moist Therapy % of patients 46 40 $38.8 38.8 DRESSING CHANGES $26.0 � 42.1% home care � ≈ 80% done by professionals 20 � 24.4% inpatient � ≈ 20% done by non-professionals 7 2 2 0 0 � 18.3% outpatient clinic % healed Therapy days Re-amputation Major Cost in USD (% of total days) re-amputation (x1,000) 3
4/16/2016 Resource Use and Economic Costs NPWT with Instillation + INSTILLATION = BENEFICIAL CONCLUSION Adjunctive therapy to cleanse wound bed decreasing bacterial � post- Treatment of diabetic patients with bioburden amputation wounds using NPWT resulted in lower resource utilization greater Indicated for all wound types with bioburden, wound bed debris, and a � proportion of patients obtaining wound healing heavy exudate, contaminated/infected wounds at a lower overall cost of care when compared Improved # of debridement, LOS, length of therapy, time to wound � to moist wound healing closure, improved culture results, decreased cost NPWT + Instillation = adjunctive therapy � APELQVIST ET AL., AM J SURG 2008 All studies are based on inpatient care or undefined populations � Gupta et al. Int Wound J 2016 ; Kim et al., Plast Reconstr Surg 2013; Kim et al., Plast Reconstr Surg 2014; Gabriel et al., Int Wound J 2012; Timmers et al., Wound Rep Reg 2009 Medicare LCD: Ulcers & Wounds Home Setting Is it Safe Outpatient? MAUDE - Manufacturer and User Facility Device Experience, Accessed April 8, 2016 ADVERSE EVENTS BY EVENT TYPE TOTAL ADVERSE EVENTS BY EVENT TYPE, 2011-2016 ULCER & WOUND TYPES Stage III or IV pressure ulcer Venous or arterial insufficiency G 1200 300 April 2011-Mar 2012 Neuropathic Chronic, mixed etiology (present > 30 days) 1000 April 2012-Mar 2013 250 April 2013-Mar 2014 800 736 Must have tried or considered & ruled out complete wound therapy April 2014-Mar 2015 200 program described by Criterion 1 and Criteria 2, 3, or 4 April 2015-Mar 2016 600 150 Criteria 2, 3, or 4 Criterion 1 400 100 200 22 Address, apply, or consider & R/O 2. Stage III or IV pressure 50 0 � Document evaluation, care, wound � Turned & positioned appropriately 0 measurements by licensed � Group 2 support surface for extremities Death Injury Malfunction NA Other professional � Moisture & incontinence managed � Apply dressings to maintain moist TOTAL FDA REPORTED ADVERSE EVENTS ASSOCIATED WITH NPWT OVER 5 YEAR PERIOD (2011-2016) 3. Neuropathic environment 1040 1200 � Comprehensive diabetic mgmt. program � Debride necrotic tissue if present 1000 � Pressure reduced using proper modalities 800 � Evaluate and provision for 600 398 adequate nutritional status 4. Venous 253 400 163 122 104 200 � Compression bandages applied consistently 0 � Leg elevation and ambulation encouraged April 2011-Mar 2012 April 2012-Mar 2013 April 2013-Mar 2014 April 2014-Mar 2015 April 2015-Mar 2016 Grand Total 4
Recommend
More recommend